An elderly patient Mr A, 80 yrs, presented to emergency with severe stridor. He has been recently diagnosed to have supraglottic growth and he was awaiting a Direct laryngoscope and biopsy for the same by ENT surgeons.
On arrival to emergency, he had a room air saturation of 80% and with O2 around 90%. His higher functions, heart rate & blood pressure were stable. He had no other significant systemic illness.
An emergency surgical tracheostomy and a DL scopy with biopsy following it was planned. The patient was wheeled into Operating room immediately. After a brief discussion with ENT surgeons, it has been decided to try for an awake intubation to secure airway for oxygenation and ventilation.
Awake intubation is a technique used to secure airway without paralysing the muscles or in other words” securing airway in a spontaneously breathing awake patients”. This is a less common method used to secure the airway as anticipated difficult airway is its only indication. It can be achieved either with Fibre Optic Bronchoscope (FOB) or Video laryngoscope. We have decided to try with video laryngoscope. Also we have ensured difficult airway cart and instruments for FONA (front of neck access) are readily available.
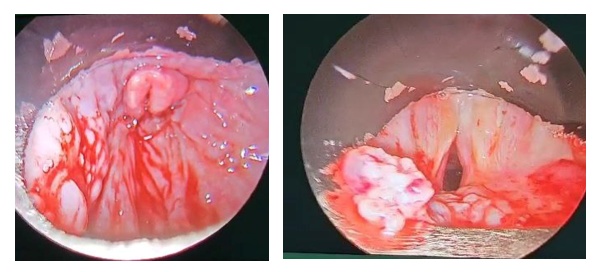
With intravenous line secured, monitors attached and under very mild sedation with fentanyl, 10% lignocaine spray applied to oropharynx and a gentle video laryngoscopy was done. We could not be able to appreciate the anatomy at all. What we could see was the supraglottic growth. With great difficulty during the second attempt, we could visualise a very small glottic opening through which we were able to pass a 5mmID endotracheal tube with a stilet inside it.
After confirming the placement with etCo2, general anaesthesia was administered. The surgical team proceeded with tracheostomy and a direct laryngoscopy & biopsy. It turned out to be a malignant lesion for which the patient is currently undergoing radiotherapy as advised.
Below are the images taken during DL scopy after tracheostomy which shows a supraglottic growth obstructing the airway.
Discussion:
Anticipated difficult airway in an elective setting can be handled by an expert in a more effective and successful manner than emergency situations. In an emergency where the patient is desaturating, airway has to be secured as quickly as possible. When such scenario is associated with a difficult airway, it becomes a challenge for the anaesthesiologist. Complications while attending such patients include hypoxia, hypercarbia, arrhythmias, cardiac arrest, airway trauma, bleeding, aspiration and CICV (Can’t ventilate can’t intubate) scenario. Options during such situations include awake fibre optic intubation, awake video laryngoscope intubation, emergency tracheostomy under local anaesthesia. If the patient desaturates fast while performing any of these options, then immediately front of neck access (FONA) has to be done. It is a life saving emergency procedure where a cricothyrotomy is done to introduce endotracheal tube through the neck. Fortunately, in our patient we were able to achieve intubation using a small sized tube with the help of a video laryngoscope.
 Dr. V. Murali Magesh, M.D, EDAIC
Dr. V. Murali Magesh, M.D, EDAIC
Consultant Anaesthesiologist
Kauvery Hospital Chennai