INTRODUCTION
A high-risk pulmonary embolism (PE) is a life-threatening medical emergency characterized by the sudden obstruction of one of the major or more pulmonary arteries by acute thrombus or by a large embolus, leading to persistent cardiogenic shock, hypoxia and respiratory failure. It requires a rapid and effective management strategy to improve patient outcomes and reduce mortality rates. In this case report, we highlight the challenges and strategies involved in managing a patient with massive pulmonary embolism with cardiogenic shock.
CASE REPORT:
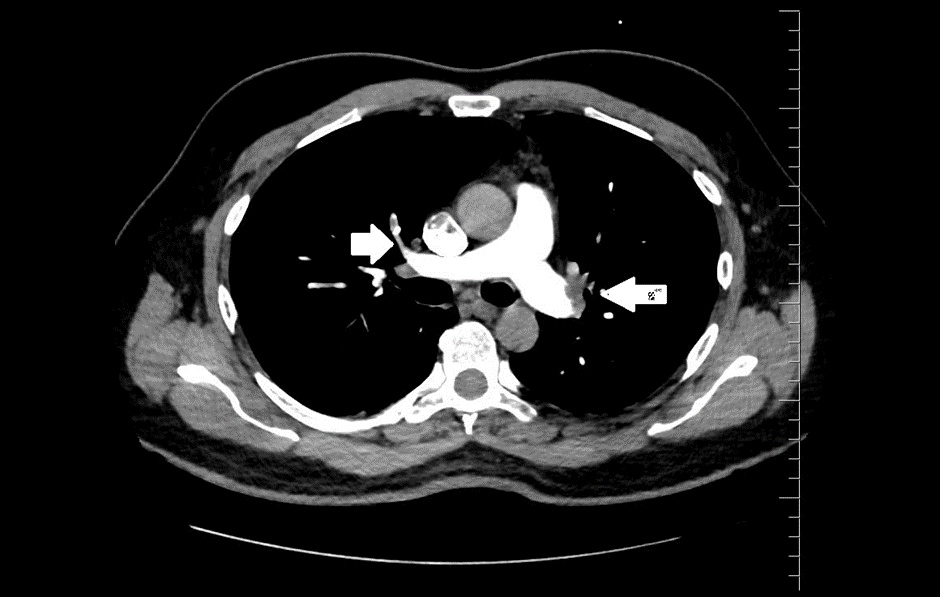
A 48yr old male with no previous past medical history presented to the Emergency room with sudden onset breathlessness and giddiness for 4 hours. On arrival his blood pressure was 70/30mmHg, pulse rate was 130/minute with saturation of 80% in room air. He was started on large boluses of Intravenous fluids and inotropes – Nor-adrenaline and dopamine and started on high flow oxygen support. An electrocardiogram was done showed sinus tachycardia with right bundle branch block, S1Q3T3 pattern (FIGURE: 1). 2D- ECHO done showed grossly dilated Right atrium and ventricle, dilated main pulmonary artery, severe tricuspid regurgitation with pulmonary artery systolic pressure of 90mmHg, Adequate LV systolic function (FIGURE ). ECMO was kept on standby. Given the echo findings, immediate IV Heparin 10000 IU and Thrombolysis was initiated with Alteplase, while fluid resuscitation and inotropic support was continued. Following partial hemodynamic stability patient underwent an immediate CT- Pulmonary Angiogram which revealed thrombotic occlusion in bilateral pulmonary arteries suggestive of High- risk pulmonary embolism. He was continued on heparin infusion. Inotropes were slowly tapered and stopped by the next day. The saturation and blood pressure recovered by second day post thrombolysis and became hemodynamically stable with no other complications. Bilateral lower limb venous doppler done was normal. Malignancy was ruled out. Prothrombotic causes of pulmonary embolism was done revealed hyper-homocystenemia and vitamin B12 deficiency. He was started on Apixaban at discharge, vitamin B12, Folate supplements and asymptomatic since then on follow up.
DISCUSSION:
High-risk pulmonary embolism (PE), which presents as shock or persistent hypotension, is a life-threatening disorder associated with high mortality and morbidity. The 30-day mortality rate of patients with PE who develop shock ranges from 16 to 25% and that of patients with cardiac arrest ranges from 52 to 65%. While the majority of pulmonary embolisms (PE) are caused by common risk factors such as deep vein thrombosis (DVT), malignancy and immobilization, there are some fewer common factors that can also lead to PE. These rare factors often involve specific medical conditions, genetic predispositions, or unique circumstances. Here are some rare factors leading to pulmonary embolism:
- Hypercoagulable Conditions: Paroxysmal nocturnal haemoglobinuria, antithrombin III deficiency, and protein C or protein S deficiency.
- Myeloproliferative Disorders: Polycythaemia vera, essential thrombocythemia, and primary myelofibrosis can cause the overproduction of blood cells, leading to an increased risk of thrombosis and pulmonary embolism.
- Heparin-Induced Thrombocytopenia (HIT)
- Antiphospholipid Syndrome:
- Elevated Homocysteine Levels:
- Catheter-Related Thrombosis:
- Air Embolism
- Amniotic Fluid Embolism
- Foreign Material Embolism
- Travel-Related PE
Pathophysiology
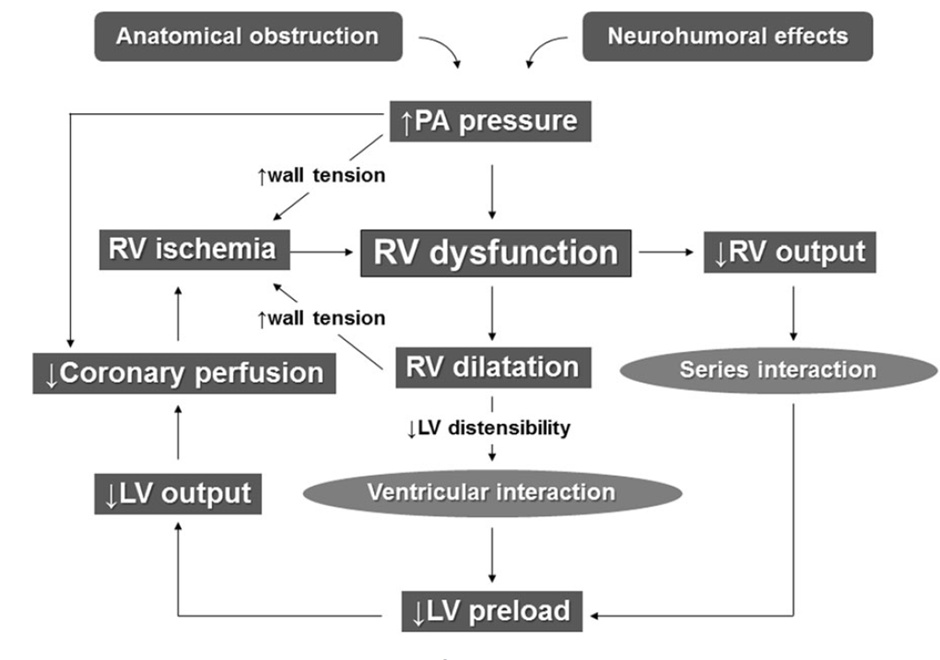
Early recognition, diagnosis, and immediate management is critical. High-risk pulmonary embolism, with its potential to cause cardiogenic shock, presents a dual threat to the cardiovascular system. Cardiogenic shock in the context of a massive PE, this typically occurs due to increased pressure in the right side of the heart and decreased left ventricular output, often leading to acute right heart failure. As a result, patients present with profound hypotension, tachycardia, hypoxia and severe respiratory failure. The series of events is explained in the algorithm below.
DIAGNOSIS
Diagnosing a massive PE with cardiogenic shock can be challenging because symptoms can mimic those of other cardiac and respiratory conditions. However, several diagnostic tools are essential in identifying this critical condition:
- CT Pulmonary Angiography (CTPA)
- Echocardiography
- Biomarkers: Elevated D-dimer levels and cardiac troponins, can indicate the presence of a massive PE and associated cardiac injury.
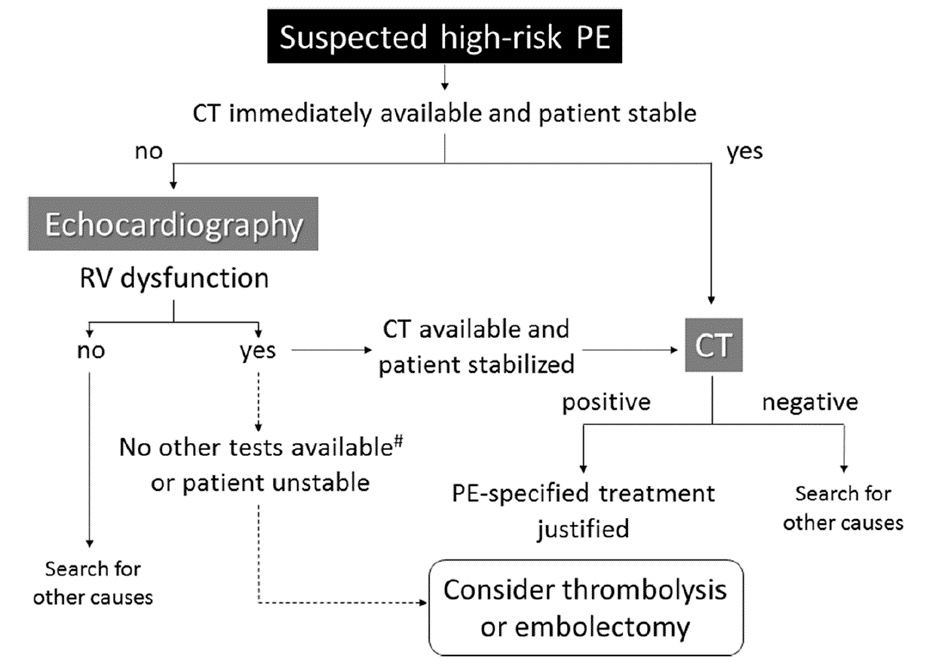
PROPOSED DIAGNOSTIC ALGORITHM FOR PATIENTS WITH SUSPECTED HIGH-RISK PE.
TREATMENT STRATEGIES
Managing a patient with massive pulmonary embolism and cardiogenic shock requires a multidisciplinary approach, involving emergency physicians, interventional cardiologists, radiologists, and intensivists. Here are the key treatment strategies:
- Stabilization: The immediate goal is to stabilize the patient’s vital signs. This often involves administering intravenous fluids, vasopressors, and inotropes to maintain blood pressure and cardiac output.
- Systemic Thrombolysis: In many cases, systemic thrombolysis with medications like tissue plasminogen activator (tPA) is the preferred treatment option. Though it carries a risk of bleeding complications and must be carefully weighed against the potential benefits.
- Catheter-Directed Therapy: In cases where thrombolysis is contraindicated or unsuccessful, catheter-directed therapies such as catheter-directed thrombolysis, mechanical thrombectomy, or the use of retrievable inferior vena cava filters may be considered.
- Surgical Embolectomy: In extreme cases, when other therapies fail or are contraindicated, surgical embolectomy may be necessary. This involves open-heart surgery to remove the thrombus from the pulmonary arteries.
- Supportive Care: Patients with massive PE and cardiogenic shock often require intensive care unit (ICU) admission for close monitoring and support. Mechanical ventilation and extracorporeal membrane oxygenation (ECMO) may be necessary in severe cases.
CONCLUSION
Managing massive pulmonary embolism with cardiogenic shock is a complex and high-stakes endeavour that demands swift and coordinated action. Early recognition, appropriate diagnostic measures, and timely initiation of treatment are crucial for improving patient outcomes. Given the high mortality associated with PE, a systematic approach to care and access to advanced interventions are essential to increase the chances of survival for these critically ill patients.
FIGURE: 1– 12 Lead ECG showing Normal Sinus Rhythm, Heart rate – 130/minute, Right Bundle Branch block, S1Q3T3 pattern.
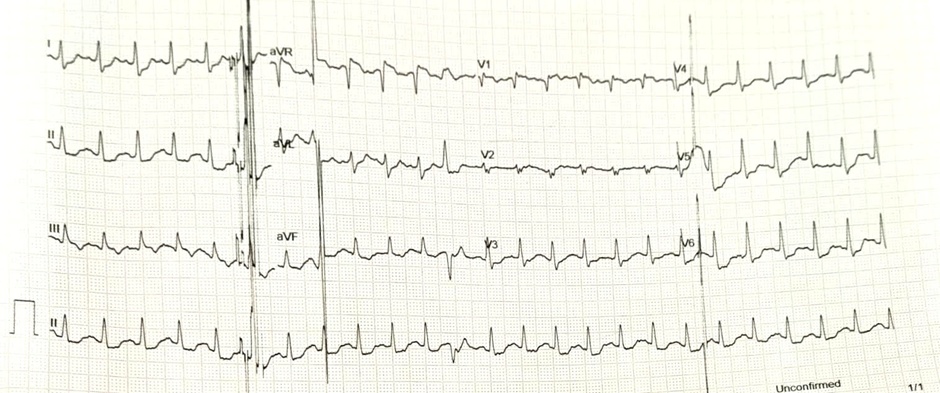
FIGURE:2– 2D- Transthoracic ECHO- showing Dilated Right atrium and ventricle(2A), D Shaped LV(2B).
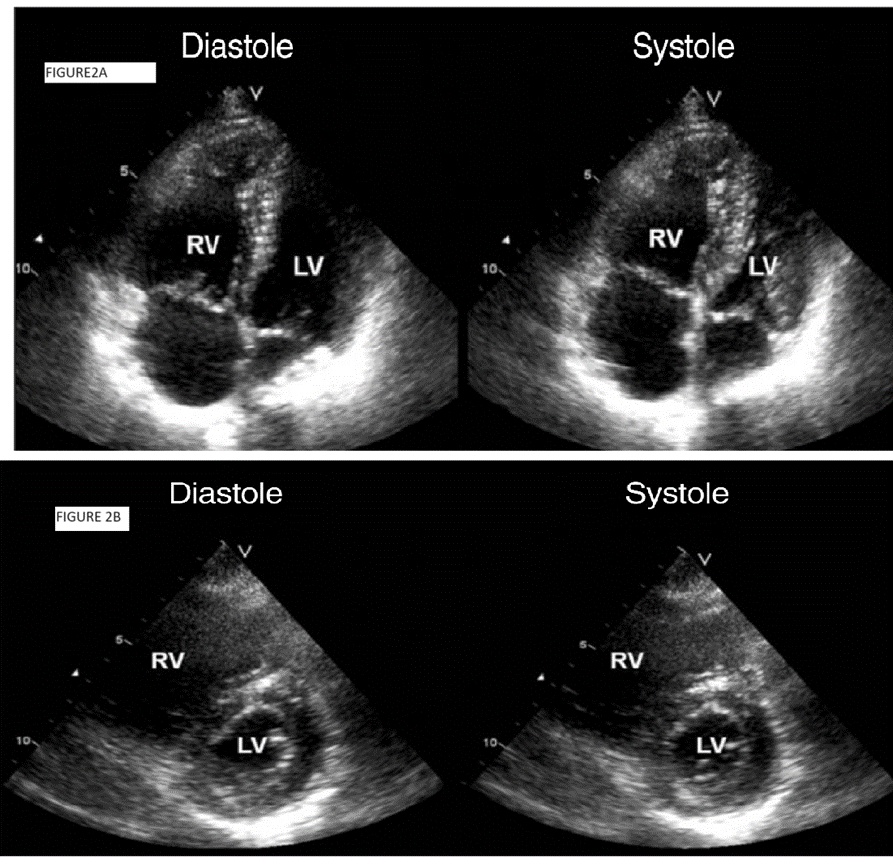
FIGURE:3– CT- Pulmonary Angiogram showing bilateral pulmonary artery with thrombotic occlusion (WHITE ARROWS showing the filling defect)