Abstract
Eucalyptus oil is a traditional herbal medicine widely used for a number of common ailments. Extreme toxicity following ingestion is well-documented, but public awareness is generally lacking. The toxic symptoms are rapid in onset, which include a burning sensation in the mouth and throat, abdominal pain, and spontaneous vomiting. The initial central nervous system (CNS) effects are giddiness, ataxia, and disorientation followed by loss of consciousness and convulsions occurring within 30 mins.
Case report
49 years female, known systemic hypertension, type 2 diabetes mellitus and hypothyroidism, presented to ER with alleged history of accidental ingestion of eucalyptus oil of approximately 10ml in her residence after which she had 3 episodes of watery vomiting followed by 2 epiodes of involuntary jerky movements involving all 4 limbs with uprolling of eyeballs, tongue bite and urinary incontinence.
On initial evaluation at ER
Patient in ictal state.
Airway
Threatened – suctioning done, Oropharyngeal airway inserted.
Breathing
RR – 28/ min, Spo2 – 66% RA – connected to high flow oxygen using NRBM.
B/L air entry equal, B/L wheeze with harsh vesicular sounds heard .
Circulation
BP – 170/ 100 mmHg. HR – 128/ min,
CVS -Tachycardic, S1S2 normal, no murmur, JVP – Normal,
PA – Soft, non-tender, no organomegally, bowel sounds heard.
Disability
Patient in status-Active GTCS+ , B/L PUPIL dilated.
CBG – 260 mg/dl
Exposure
Temp: 98.6o F
Tongue bite with bloody frothy secretions noted.
POC:
pH – 6.780
PCO2 – 72.9 mmHg
PO2 – 28 mmHg
BE – -24 mmol/ L
HCO3 – 10.8 mmol/ L
LAC – >20 mmol/ L
Na+ – 141 mmol/ L
K+ – 3.3 mmol/ L
Cl- – 104 mmol/ L
BUN – 7 mg/dL
CREAT – 1.1 mg/dL
Course in ER:
- Patient positioned in left lateral position, intravenous access commenced and injection lorazepam 4mg stat given.
- She had recurrent GTCS hence loaded on dual anti-epileptics after neurology consult.
- In view of status epilepticus, she was intubated and connected to mechanical ventilator.
- In view severe metabolic acidosis, she was also injection sodium bicarbonate 200mg bolus followed by infusion.
- After stabilization, With provisional diagnosis of Eucalyptus oil poisoning – Status epilepticus, Pneumonitis (Chemical vs Aspiration), patient shifted to ICU.
Repeat ABG:
pH – 7.34
PCO2 – 39 mmHg
PO2 – 110 mmHg
BE – -3 mmol/ L
HCO3 – 21.5 mmol/ L
LAC – 9.48 mmol/ L
Course in ICU:
- Patient GCS improved and extubated the very next day.
- In view of chemical pneumonitis, patient started on nebulisations.
- MRI brain and EEG – Normal.
- Anti-epileptics weaned off slowly.
- Patient discharged without any anti-epileptics and was normal in repeat follow ups.
Discussion:
- Eucalyptus oil is a widely used household item that comes in various forms such as essential oil, medicinal remedy, cleaning agent, inhalation/vaporizer fluid, or topical preparation. It’s essential to be aware that eucalyptus oil is highly toxic, and even small ingestions of as little as 5 mL can result in severe symptoms. The primary concerns with eucalyptus oil poisoning involve central nervous system (CNS) depression and respiratory issues. In children, typical side effects may include reduced consciousness levels, unsteady movements (ataxia), seizures, and vomiting.
- In a study conducted by K. Jagadish Kumar et al., involving 109 children who had ingested eucalyptus oil, it was found that 59% of them displayed symptoms. Among these cases, 30% exhibited mild poisoning, characterized by symptoms like ataxia, vomiting, and abdominal discomfort. Moderate poisoning, as indicated by a Glasgow Coma Scale score between 8 and 14, was observed in 25% of the cases. Major poisoning leading to a coma, with a coma scale rating between 3 and 7, was seen in 4% of the cases.
- Many species of the genus Eucalyptus from the Myrtaceae family (Eucalyptus citriodora (EC), Eucalyptus tereticornis (ET), and Eucalyptus globulus (EG)) are used in Brazilian and Indian native medicine for the treatment of various medical conditions such as cold, flue, fever, and bronchial infections. α-pinene, myrcene, cineole, fenchone, α-terpinolene, and β-terpinyl acetate are well described in true eucalyptus oil, with cineole being the main constituent. Eucalyptus oil, derived from the genuine eucalyptus tree, is devoid of camphor. On the other hand, eucalyptus oil produced from the cineole fraction of camphor laurel, often referred to as “imitation eucalyptus oil,” may potentially include camphor. It’s worth noting that camphor, similar to eucalyptus oil, has the potential to induce epileptic seizures.
- Eucalyptus oil finds widespread use as an over-the-counter remedy in many countries, and it also has various applications in pharmaceuticals, flavorings, pesticides, perfumes, and industries. However, the allowable limits for its presence are often not well-regulated. Similarly, the utilization of camphor follows a similar pattern. Surprisingly, even healthcare professionals are often unaware of the potential toxicity associated with these seemingly harmless substances. It is crucial to establish strict regulations governing the permissible levels of these ingredients in products containing them. Additionally, products containing eucalyptus oil or camphor should be required to carry explicit warnings about their potential toxic effects, including the risk of seizures.
- In 1898 , the first case report of Eucalyptus oil induced seizure was reported from kerala. Most healthcare professionals are unaware of the epileptogenic potential of eucalyptus oil. If a proper history is not obtained there is every possibility to label the seizures as Idiopathic seizures and patient may have to take long term antiepileptic drugs. These seizures don’t recur and AED can be safely withheld after two weeks.
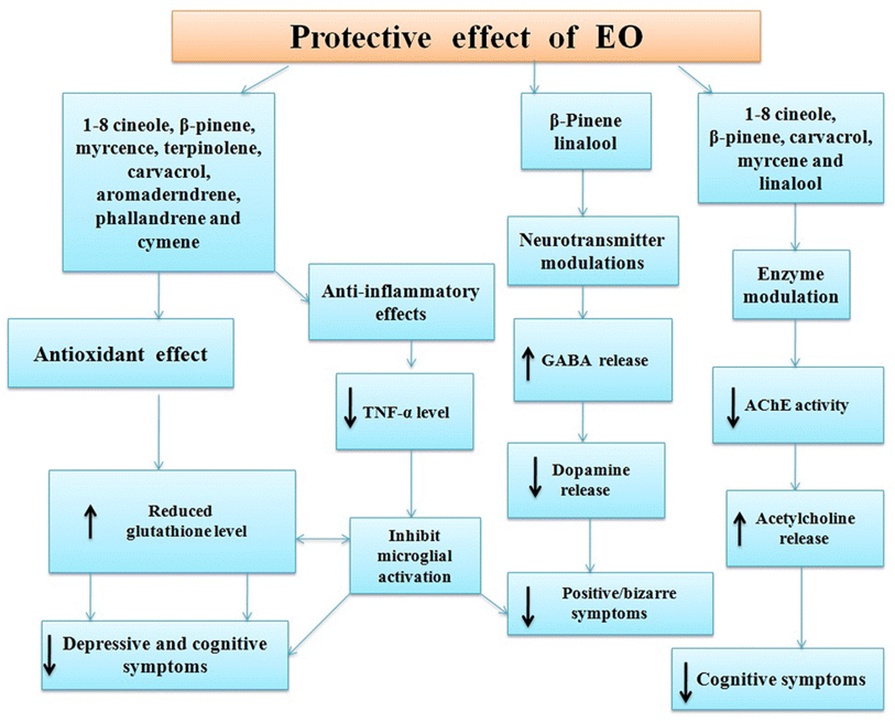
Pathophysiology of Eucalyptus Oil-Induced Seizures:
- Exposure to Eucalyptus Oil:
Eucalyptus oil is commonly used in aromatherapy, topical ointments, and as a remedy for various respiratory conditions.
- Absorption and Distribution:
When eucalyptus oil is used, it can be absorbed through the skin, inhaled as vapor, or ingested in some cases.
- Main Active Ingredient:
The main active ingredient in eucalyptus oil responsible for potential seizures is often cineole (also known as eucalyptol).
- Neurological Impact:
Cineole can cross the blood-brain barrier and affect the central nervous system.
- Neurotransmitter Disruption:
Cineole may disrupt the balance of neurotransmitters in the brain, particularly by affecting gamma-aminobutyric acid (GABA) and glutamate.
- GABA Inhibition:
Cineole may reduce the inhibitory effects of GABA, an essential neurotransmitter that dampens neural activity and prevents excessive neuronal firing.
- Increased Glutamate Activity:
With reduced GABA inhibition, there can be an increase in glutamate activity, which is an excitatory neurotransmitter.
- Excitotoxicity:
The imbalance between GABA and glutamate can lead to a state of excitotoxicity, where excessive neuronal firing and hyperactivity occur.
- Seizure Threshold Lowering:
Excitotoxicity and neuronal hyperactivity can lower the seizure threshold in susceptible individuals.
- Seizure Onset:
In individuals with a lowered seizure threshold, the imbalance in neurotransmitters and hyperexcitability of neurons can trigger seizures.
- Seizure Manifestation:
Seizures may manifest in various forms, including tonic-clonic seizures, absence seizures, or focal seizures, depending on the specific brain regions affected.
- Individual Variability:
The susceptibility to eucalyptus oil-induced seizures can vary among individuals. Factors such as dosage, individual sensitivities, and pre-existing neurological conditions play a role.
 Conclusion:
Conclusion:
Every medical practitioner should possess knowledge about the potential toxic effects of eucalyptus oil, a substance commonly encountered in daily life in India. Given that there is no specific antidote available, it is imperative to provide supportive care in the emergency room. This care should include promptly addressing metabolic acidosis and ensuring the maintenance of hemodynamic parameters, which can lead to a swift recovery.
It’s worth noting that when eucalyptus oil is inhaled, CNS symptoms manifest more rapidly. This is due to the direct access of inhaled volatile oils to the brain, where they stimulate neurons. Consequently, it is essential to mandate warning labels on all products containing eucalyptus oil. Raising awareness about the health risks associated with eucalyptus oil among the public is crucial in order to prevent unnecessary complications.
Acknowledgement:
For guiding me with the article, I would like to thank,
Dr.Aslesha (Consultant & Clinical lead – Department Of Emergency Medicine)
“The author declares no conflict of interest”
Reference:
- Webb NJ, Pitt WR. Eucalyptus oil poisoning in childhood: 41 cases south-eastQueensland. J Paediatr Child Health. 1993;29:368–71. [PubMed] [Google Scholar].
- Patel S, Wiggins J. Eucalyptus oil poisoning. Arch Dis Child. 1980;55:405–6. [PMC free article] [PubMed] [Google Scholar].
- Flaman Z, Pellechia-Clark S, Bailey B, et al.Unintentional exposure of young children to camphor and eucalyptus oils. Paediatr Child Health. 2001;6:80–3.
- Kumar KJ, Sonnathi S, Anitha C, et al.Eucalyptus oil poisoning. Toxicol Int. 2015;22(1):170–1.
- Dhakad AK, Pandey VV, Beg S, et al.Biological, medicinal and toxicological significance of eucalyptus leaf essential oil: a review. J Sci Food Agric. 2018;98(3):833–48.
- Darben T, Cominos B, Lee CT. Topical eucalyptus oil poisoning. Australas J Dermatol. 1998;39(4):265–7.
- Manoguerra AS, Erdman AR, Wax PM. Camphor poisoning: an evidence-based practice guideline for out-of-hospital management. Clin Toxicol. 2006;44:357–70.

Dr. Silvera Samson Raj,
Emergency Resident,
Kauvery Hospital, Chennai.



