Patient presentation
A 70-year-old male, presented to the ER with a history of fever, neck pain, and generalized tiredness. He has a known history of diabetes mellitus and no known drug allergies (NKDA). Upon examination, he was conscious, oriented, and febrile with a temperature of 100.2°F. His vitals were stable, with a pulse rate of 100/min, blood pressure of 130/70 mmHg, and oxygen saturation of 98% in room air. His capillary blood glucose was elevated at 434 mg/dl. Respiratory and cardiovascular examinations were unremarkable, with bilateral air entry and normal heart sounds (S1, S2). The abdomen was soft with bowel sounds present, and his neurological status showed minimal neck rigidity with no focal deficits.
Recent Medical History and Admission:
A 70-year-old male with a recent history of treatment for right superior orbital tissue syndrome (Tolosa-Hunt Syndrome) and cranial nerve palsy involving the right 2nd, 3rd, 4th, and 6th cranial nerves, presented with generalized malaise, fatigue, and an inability to walk. He also has a history of Type II diabetes mellitus and was under steroid treatment. On 12/08/2024, he was admitted to the ICU with high-grade fever. On examination, he exhibited neck rigidity and swelling in the left hand.
Initial Investigations and Treatment:
The patient was started on IV antibiotics, including Inj. Meropenem, Inj. Vancomycin, and Inj. Acyclovir. Blood investigations revealed elevated white blood cell count (WBC: 37320), elevated C-reactive protein (CRP: 311), and arterial blood gas (ABG) showed elevated lactate (3.8), indicative of sepsis. Urine routine analysis showed pus cells (8-10) and nitrite positivity. A CT chest scan revealed no significant abnormalities except for dependent changes, with no thoracic source of infection. Incidental findings of soft tissue density lesions with mild surrounding inflammation in the right supraclavicular region raised the possibility of lymphadenopathy, prompting a recommendation for a focused ultrasound (USG) correlation.
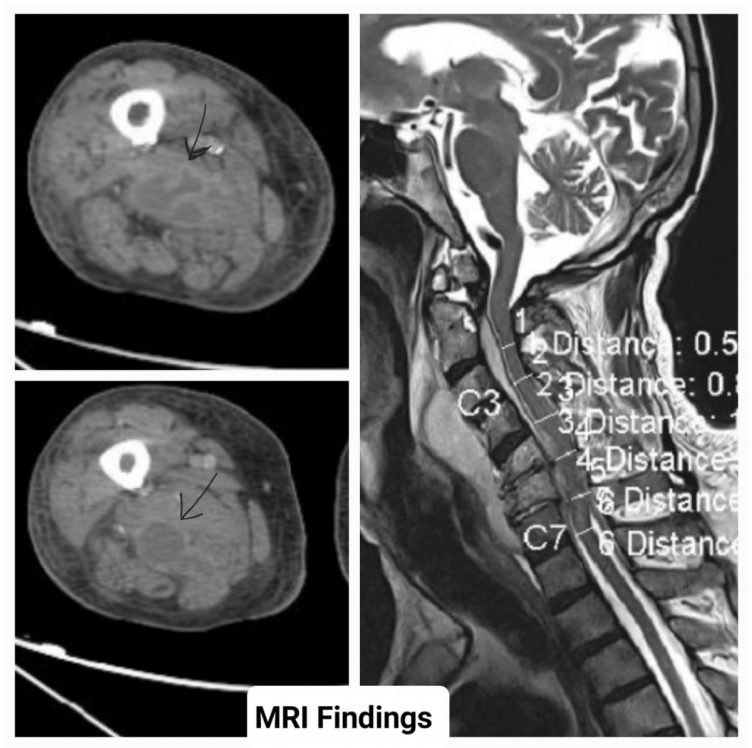
Imaging and Further Investigations:
A CT abdomen showed bilateral perinephric fat stranding, suggesting pyelonephritis, along with left renal cortical cysts, and no ascites or other solid organ or bowel abnormalities. Given the redness and localized swelling in the left dorsum of the hand, the plastic surgery team recommended a venous Doppler of the left hand, which revealed cephalic vein thrombosis up to the mid-forearm and complete thrombosis of the basilic vein. No deep vein thrombosis was observed in the right upper limb. A USG of the right hand showed tenosynovitis of the flexor digitorum superficialis of the third finger, with diffuse inflammatory changes involving the mid-palmar space, though no definable collection was noted. The patient underwent an incision and drainage procedure for the left-hand abscess.
Neurological Findings:
MRI brain with contrast showed age-related changes, including thin, diffuse periventricular and patchy subcortical white matter ischemic changes, along with mild pachymeningeal enhancement. These findings suggested possible infection or post-dural puncture with intracranial hypotension. An MR angiogram showed no evidence of stenosis or occlusion. MRI orbit findings (reports enclosed) were also evaluated. A neurologist diagnosed subacute meningitis, leading to the cessation of Acyclovir, and antibiotics were adjusted to Inj. Flucloxacillin after consultation with infectious disease and critical care specialists for MSSA sepsis.
Cardiovascular Assessment:
A cardiologist was consulted, and the patient underwent a transesophageal echocardiogram (TEE) under IV sedation. No vegetations were observed. Dermatological consultation was obtained for redness and swelling in the hand, and treatment advice was followed. Ophthalmology consultation ruled out papilledema.
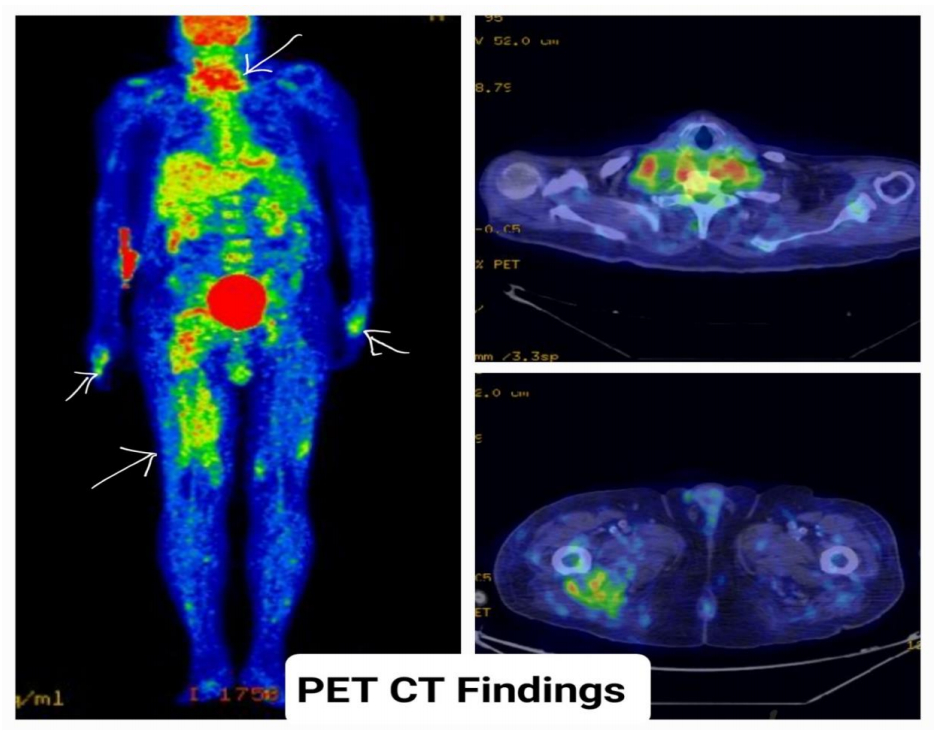
Rising WBC Count and PET-CT:
Although the WBC count initially showed a reducing trend, it began to rise again, leading to a PET-CT scan. The PET-CT showed a heterogeneous collection with air pockets in the prevertebral region and low-grade metabolic activity in the cervical spine (C4 level), paravertebral, and posterior perivertebral regions. A similar collection was seen in the right pelvis, extending into the right thigh. The findings suggested abscess formation, and further microbiological correlation was recommended.
Surgery and Postoperative Care:
Following a multidisciplinary team review, including critical care, spinal surgery, and plastic surgery teams, the decision was made to proceed with surgery. The patient underwent successful surgery after receiving anesthetist and cardiology clearance. He tolerated the procedure well, with 2 units of PRBC transfusion administered intraoperatively. On the third postoperative day (POD), he was transferred to the ward, where follow-up blood tests showed decreasing trends in inflammatory markers. Despite a gradual rise in WBC and CRP levels, further blood cultures showed no bacterial growth.
Surgical details:
A series of five different complex and successful surgical interventions were carried out to expertly manage the patient’s severe abscesses and spinal complications. The left forearm was meticulously explored and debrided, with necrotic tissue excised and a drain strategically placed to ensure optimal recovery. A challenging cervical corpectomy of C5 and C6 was performed with precision, removing the diseased disc and securing a Globus expandable cage and cervical plate, all while maintaining structural integrity and reducing infection risk. The palmar abscess in the right hand was expertly drained, ensuring preservation of the flexor tendon sheath through careful decompression. The right thigh abscess was skillfully incised and drained, removing 200 ml of pus and placing a drain to promote healing. In a remarkable display of surgical proficiency, the cervical plate was revised due to bone resorption and cage migration, with the placement of a larger, more secure plate and screws, ensuring structural stability and long-term success. Each procedure demonstrated a high level of expertise, contributing to the patient’s recovery and stability.
Postoperative Imaging:
A CT cervical spine scan showed an anterior spinal fixation device at the C4-C7 level, with residual prevertebral, paravertebral, and epidural collections. A CT abdomen revealed bilateral renal cortical cysts and minimal perinephric fat stranding. A CT scan of the right thigh showed a reduction in the size of the abscess compared to a previous MRI, though further assessment with USG or MRI was recommended. Repeat blood cultures revealed gram-positive cocci and Enterococcus, for which Inj. Teicoplanin was initiated.
Antibiotic Therapy and Discharge:
The patient was started on a regimen of Inj. Ceftazidime-Avibactam-Aztreonam for MDR Klebsiella and continued for 5 days. Pus cultures revealed Staphylococcus aureus, prompting continuation of flucloxacillin. His vital signs, electrolytes, and inflammatory markers were closely monitored. With improving clinical signs and reduced inflammatory markers, the patient’s condition stabilized. The infectious disease specialist recommended completing a course of Inj. Ampicillin for 12 days, Cefazolin for 4 weeks, and Ceftazidime-Avibactam for an additional 2 days.
Discharge Plan:
The patient showed significant clinical improvement, with reduced fever, tachycardia, and no evidence of further complications. The drainage tube and catheter were removed, and the patient was discharged with a follow-up plan and specific discharge medications including continuing IV Antibiotic course covering Staphylococcus aureus, Enterococcus fecalis, MDR Klebsilla organisms.
Review:
The patient came at 1 week review, performing well, tolerating the IV Antibiotics with decreasing WBC trend, getting regular physiotherapy and other supportive care, advised to continue and complete the course of IV Antibiotics.
FINAL DIAGNOSIS:
– METHICILLIN SENSITIVE STAPHYLOCOCCUS AUREUS SEPSIS—[CERVICAL – EPIDURAL ABSCESS C4 TO C6, MULTIPLE LEVEL OSTEOMYELITIS WITH BONE EROSION, MULTIPLE SOFT TISSUE WOUND INFECTION (S. AUREUS), RIGHT THIGH ABSCESS, RIGHT HAND PALMAR ABSCESS, LEFT FOREARM INFECTED THROMBOPHLEBITIS, BILATERAL PYELONEPHRITIS]
– ENTEROCOLLUS FECALIS – BACTEREMIA
– MDR – KLESIELLA PNEUMONIA – UROSEPSIS
– TYPE II DIABETES MELLITUS
– SYSTEMIC HYPERTENSION
– DYSLIPIDEMIA
PROCEDURE DONE:
– S/P EXPLORATION AND DEBRIDEMENT LEFT FOREARM ABSCESS
– S/P ACCF C5 AND C6 CORPECTOMY
– S/P RIGHT THIGH ABSCESS INCISION AND DRAINAGE
– S/P RIGHT PALMAR ABSCESS – EXPLORATION AND DRAINAGE OF ABSCESS
– S/P TRANSESOPHAGEAL ECHOCARDIOGRAM
– S/P RE-EXPLORATION AND CERVICAL PLATING
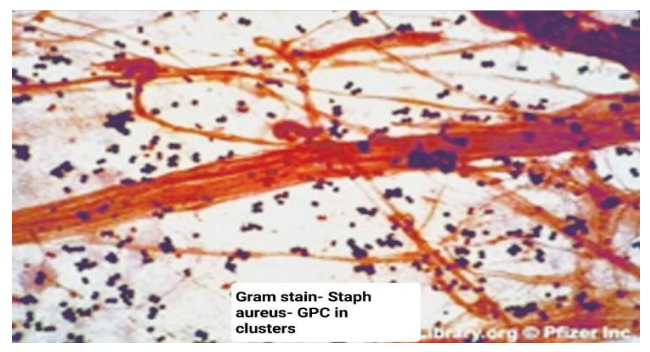
Brief about management of Staphylococcus aureus Bactremia
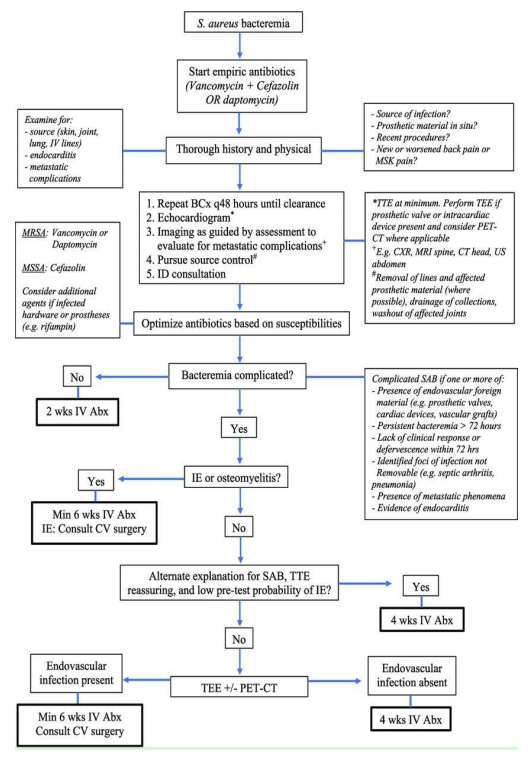
Effective management of **Staphylococcus aureus** infections requires immediate source control, such as removing indwelling devices and surgically draining abscesses, along with antimicrobial therapy tailored to the strain’s susceptibility and affected organs. Device removal is crucial, especially for coagulase-negative staphylococci (CoNS) due to biofilm formation. For patients with bacteremia, central venous catheters should be removed if bacteremia persists for over 72 hours. Antibiotic therapy duration varies, with at least 2 weeks for uncomplicated cases and 4 weeks or more for complicated ones.
Empirical therapy- When a staphylococcal infection is suspected in critically ill patients, empiric therapy targeting methicillin-resistant S. aureus (MRSA) is essential, especially in cases of septicemia, prior MRSA infection, known MRSA colonization, or risk factors like recent hospitalization, surgery, hemodialysis, and HIV infection. Proximity to indwelling medical devices also warrants MRSA coverage. Vancomycin is recommended for empiric treatment of coagulase-negative staphylococci (CoNS) due to high methicillin resistance. Patients should be monitored for clinical response and microbiologic results, with therapy tailored to pathogen susceptibility. If no improvement is seen within 72 hours, further evaluation for complications or resistant organisms is necessary.
For the treatment of MSSA bacteremia, first-generation cephalosporins like cefazolin and semisynthetic antistaphylococcal penicillins like cloxacillin are optimal. Vancomycin, though bactericidal, is less effective than beta-lactams unless there is a severe beta-lactam allergy. MRSA is defined by an oxacillin MIC of ≥4 μg/mL and is resistant to all beta-lactam antibiotics. Invasive MRSA infections should be treated with vancomycin, teicoplanin, or daptomycin. If specialized resistance testing is unavailable, methicillin resistance should be assumed.
Duration of therapy depends of the site of infection. For example, Bacteremia needs four to six weeks of therapy from the date of first negative blood culture, Osteomyelitis needs six weeks of therapy, Infective Endocarditis needs 2 weeks of therapy
Reference
https://www.researchgate.net/figure/Figure-Proposed-flow-diagram-for-
Staphylococcus-aureus-bacteremia-management-May-differ_fig1_364082368
Harrison Textbook of internal medicine
https://www.uptodate.com/contents/clinical-approach-to-staphylococcus-aureus-bacteremia-in-adults
https://www.ncbi.nlm.nih.gov/books/NBK441868/
 Dr. Vignesh. A. S
Dr. Vignesh. A. S
DNB General Medicine Resident
Kauvery Hospital, Chennai
 Dr. Jayaraman K
Dr. Jayaraman K
Senior Consultant Internal Medicine specialist and Diabetologist
Kauvery Hospital, Chennai
 Dr. Sridhar N
Dr. Sridhar N
Consultant Intensivist
Kauvery Hospital, Chennai
 Dr. Balamurali G
Dr. Balamurali G
Senior Consultant
Kauvery Hospital, Chennai
 Dr. Sathish Manivel
Dr. Sathish Manivel
Consultant Plastic and Aesthetic Surgeon
Kauvery Hospital, Chennai
 Dr. Vijayalakshmi Balakrishnan
Dr. Vijayalakshmi Balakrishnan
Senior Consultant, Infectious Diseases
Kauvery Hospital, Chennai
And Many more, from the Anesthetist, Staffs who were involved in this case