As nephrologists, our primary goal in prescribing peritoneal dialysis (PD) is to tailor the treatment to each patient’s specific physiological needs and lifestyle. The effectiveness of PD is intricately linked to a detailed and individualized prescription, which must address multiple facets of the patient’s health and treatment goals. This article delves deeper into the complexities of peritoneal dialysis prescription, exploring the physiological principles, detailed components, and considerations necessary for optimal patient outcomes.
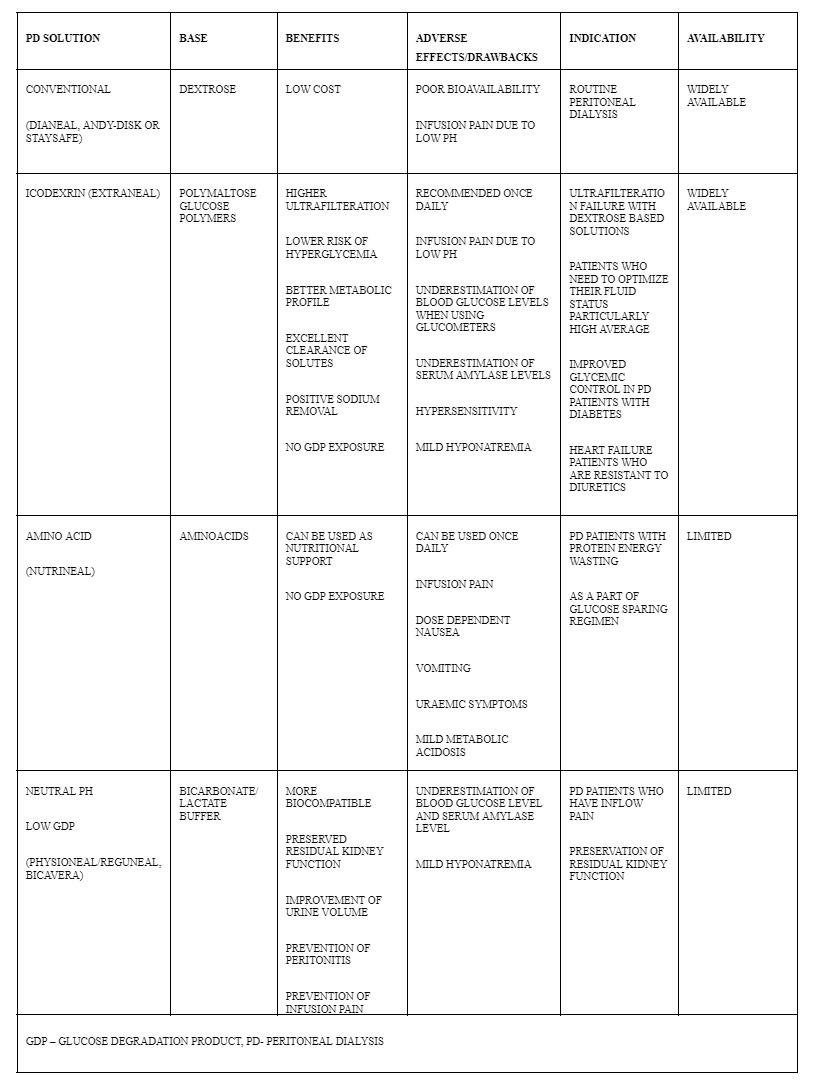
Dialysate in PD consists of glucose concentration, electrolytes, osmolarity, maintaining pH of the dialysate. Glucose acts as an osmotic agent to facilitate the removal of excess fluid from the body. The concentration of glucose in the dialysate determines the osmotic gradient between the blood and the dialysate. Typical glucose concentrations include 1.5%, 2.5%, and 4.25%. Higher concentrations increase ultrafiltration and fluid removal but may lead to glucose absorption and long-term metabolic complications such as hyperglycaemia and weight gain. Tailor glucose concentration based on the patient’s fluid balance, nutritional status, and glucose metabolism. For diabetic patients or those at risk of weight gain, using lower glucose concentrations or alternative osmotic agents like icodextrin may be appropriate.
The dialysate sodium concentration should match the patient’s serum sodium levels to avoid causing electrolyte imbalances. Adjust potassium levels in dialysate based on the patient’s serum potassium to prevent hyperkalaemia or hypokalaemia. Calcium and Magnesium should be adjusted to prevent disturbances in bone metabolism and cardiovascular health. The dialysate often contains calcium and magnesium at concentrations similar to those found in normal serum. Maintaining a pH between 5.0 and 5.5 is crucial to minimize peritoneal membrane irritation and to prevent complications like peritonitis. Proper osmolarity ensures that the dialysate does not cause significant osmotic shifts that could lead to complications such as electrolyte imbalances or dehydration.
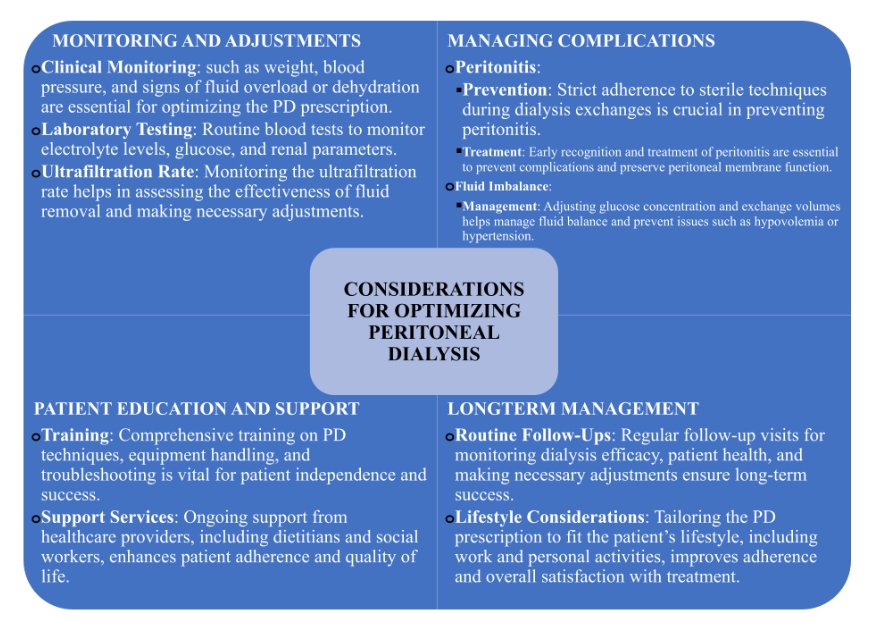
Peritoneal dialysis, when prescribed and managed with precision, offers a highly effective treatment for ESRD, providing patients with greater autonomy and flexibility. As nephrologists, our role in crafting and continuously refining the PD prescription is crucial to optimizing treatment outcomes. By carefully considering dialysate composition, exchange parameters, and patient-specific factors, we can enhance the efficacy of PD, manage potential complications, and support our patients in achieving the best possible quality of life. Regular monitoring, patient education, and individualized care remain at the heart of successful peritoneal dialysis management.
Author
 Dr C. Chaitra
Dr C. Chaitra
PG 1st Year, DrNB Nephrology
Kauvery Hospital, Chennai
Mentor
 Dr. R. Balasubramaniyam
Dr. R. Balasubramaniyam
Chief Nephrologist
Kauvery Hospital