Investigating the role of activity-based configurational developmental approach in managing mitochondrial leukodystrophy in children: A case study
M. Mahendran1, Bruno Raju2
1Consultant Paediatric Occupational Therapist, Hamsa Rehab for Kids, Kauvery Hospital, Trichy, India
2Consultant physician, Department of Physical Medicine and Rehabilitation, Hamsa Rehabilitation Centre, Trichy, Tamilnadu, India
Abstract
This case study looks at how an activity-based configurational developmental approach helps manage mitochondrial leukodystrophy in children at unit of Kauvery Hospital, Hamsa Rehab in Trichy, Tamil Nadu. Even though these disorders have different causes, children often experience similar symptoms. Improving their comfort and quality of life is a key goal, alongside medical treatments. This report presents a step-by-step approach for managing problems caused by leukodystrophies, covering how to evaluate, identify common issues, and manage care in a standardized way. Occupational therapists assess the child’s movement and create a sensory and extensor synergy pattern program for families to use. Therapy sessions focus on activities that encourage movement on both sides of the body. Tools like mean and standard deviation were used to measure how occupational therapy interventions helped the children. the study found that paediatric occupational therapy, especially play-based activities, helped improve developmental progress in children with mitochondrial leukodystrophy at Kauvery Hospital.
Keywords: Congenital; mitochondrial leukodystrophy; activity-based configurational developmental occupational therapy; standardized care approach
Introduction
Pediatric occupational therapy has seen significant growth in recent years, driven by an increasing recognition of its benefits in early childhood development and healthcare. As more families and healthcare institutions become aware of the positive impacts of these services, occupational therapy is establishing itself as a crucial intervention, especially for children facing developmental challenges. This rapid expansion is particularly evident in specialized areas like activity-based configurational developmental occupational therapy, which is increasingly implemented in healthcare settings such as Kauvery Hospital in Trichy, Tamil Nadu.
Mitochondrial leukodystrophy, a rare group of genetic disorders that affects the white matter of the brain and spinal cord, poses severe challenges to a child’s physical and cognitive development. These disorders often lead to progressive motor, sensory, and neurological deficits. Children diagnosed with mitochondrial leukodystrophy often experience deformities in both the upper and lower regions of the body, impairing movement, coordination, and muscle tone. While the genetic causes of leukodystrophies vary, many common symptoms like muscle weakness, spasticity, and cognitive impairment are shared across different cases. These complications severely impact the child’s quality of life. Occupational therapy plays a crucial role in the early intervention and management of these conditions. By focusing on restoring the child’s developmental profile, it aims to slow or reverse the progression of these deformities. The interventions are designed to enhance the child’s ability to participate in daily activities, improve mobility, and promote overall functional independence. Pediatric occupational therapists assess the child’s range of motion, posture, and physical alignment, including the shape of the head and limbs, to develop customized therapy programs. These programs often incorporate stretching exercises and activity-based developmental techniques that engage both the upper and lower body.
A key aspect of activity-based configurational developmental occupational therapy is the use of play and positioning strategies to stimulate dynamic movement. For instance, therapists encourage play activities that promote movement on both sides of the body, ensuring that children develop balance and coordination. This holistic approach not only addresses physical impairments but also improves cognitive and sensory processing, offering a more comprehensive form of rehabilitation. Early identification and treatment are essential to improving outcomes in children with mitochondrial leukodystrophy. While complete recovery may not always be possible, early intervention through these targeted Occupational Therapy techniques can greatly enhance the child’s motor and cognitive functions, reduce deformities, and improve their overall quality of life. Studies have shown that when such therapy is applied early in the disease progression, children can achieve significant developmental milestones, reducing the long-term impact of the condition.
In conclusion, the demand for pediatric occupational therapy, particularly activity-based configurational developmental occupational therapy, is growing due to its ability to address complex developmental issues like mitochondrial leukodystrophy. Through individualized care plans that involve extensor facilitation-play-based activities, and positioning strategies, therapists are helping children regain function, improve mobility, and live more fulfilling lives. Kauvery Hospital’s implementation of these interventions is a testament to the critical role Occupational Therapy plays in managing and treating developmental disorders in children
Important of paediatric occupational therapists – mitochondrial leukodystrophy
The intervention sessions using the activity-based configurational developmental approach were conducted over a period of 30 weeks, with each session lasting 45 min, 5 days a week. This consistent schedule was implemented to build trust and ensure the compliance of parents with their child’s therapy regimen. The sessions primarily focused on spatial play, which was used as a therapeutic tool to support the child’s overall development.
During these sessions, various social-emotional skills were targeted through structured play activities. These skills included basic social interactions such as greetings and salutations, turn-taking, expressing and recognizing emotions, and collaborating with others. The child was encouraged to engage in “hopeful” activities, which fostered a sense of optimism and perseverance. The therapist also worked on improving the child’s ability to focus for extended periods, follow spatial cues, and initiate conversations. All of these skills were carefully nurtured using play as an intermediary, making the activities both engaging and developmentally appropriate.
An activity schedule was also employed during the sessions, which helped reinforce learned skills and promote developmental movement patterns. The use of this schedule aimed to minimize abnormal postures and movements by guiding the child toward more appropriate physical responses. The activities supported the child’s motor and cognitive development by focusing on natural, coordinated movements that avoided undesirable positions.
Each session was recorded, either digitally or manually, for the purpose of reviewing and analysing the child’s progress. After each session, a debriefing was conducted, where the therapist and the team would discuss the outcomes, challenges, and successes observed during the session. This debriefing process was meticulously documented to ensure continuous monitoring of the child’s development and to make necessary adjustments to the treatment as needed.
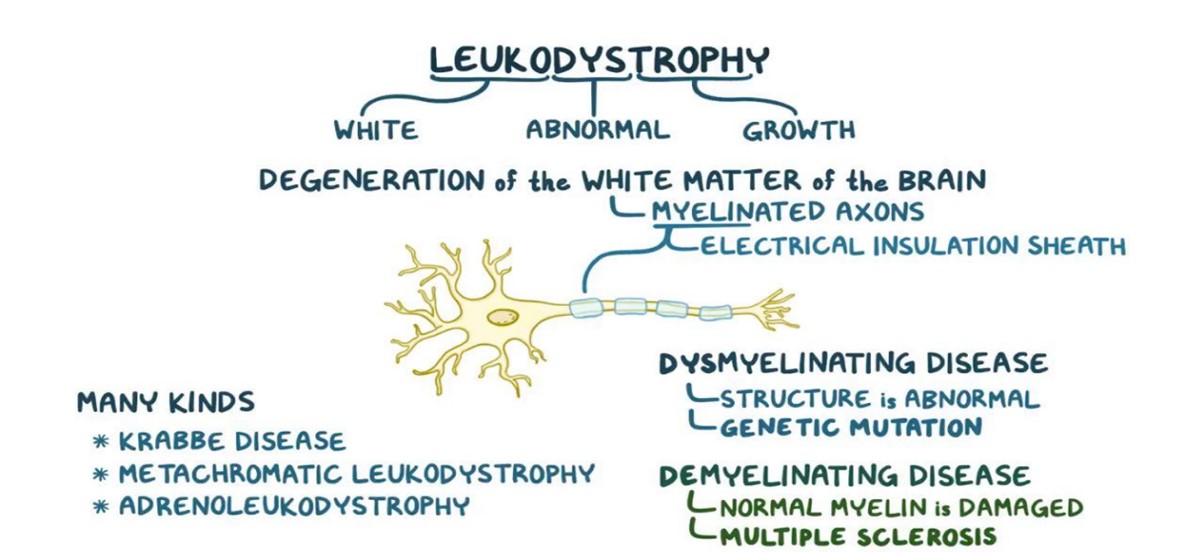

Fig. 1. Resource: w.w.w.osmosis.com
Comprehensive case report and treatment summary
A 2-year-old male child with a known history of mitochondrial disorder (genetically proven), global developmental delay, and dystonia was admitted to HAMSA rehabilitation centre for further management following treatment at Kauvery Hospital for an acute metabolic crisis. The child had frequent hospitalizations due to recurrent metabolic crises and was receiving mitochondrial supplements along with oral-T Pacitane. Presenting symptoms included difficulty moving both upper and lower limbs, lethargy, reduced activity, and the need for tracheostomy care. On admission to Kauvery Hospital, the child had a Glasgow Coma Scale (GCS) score of 5/15 and was treated for acute metabolic crisis, which included a blood transfusion (1 unit of PRBC) for decreased haemoglobin. After undergoing an MRI and tracheostomy on April 16, 2024, the child was transferred to HAMSA Rehabilitation Centre for ongoing therapy and care.
At Hamsa, the child was conscious but not fully oriented, with mild fever, and remained on a tracheostomy and nasogastric (NG) tube. His GCS score improved to E4 VT M5. Fever spikes were managed with antipyretics, and paediatric specialists were consulted for sleep disturbances and restlessness. The child’s treatment plan included weaning off the tracheostomy, and no signs of active tracheal secretions or aspiration were noted. Oral feeding was initiated and tolerated well, with good swallowing function. On May 15, 2024, the child accidentally self-decannulated the tracheostomy tube, but post-decannulation, oxygen saturation was maintained on room air without distress, cough, or desaturation, and the NG tube was removed. Physiotherapy sessions included chest physiotherapy (all positions), tone facilitation techniques, and bed mobility and balance training, during which the patient’s vitals remained stable, and the hospital course was uneventful.
Following the initial evaluation on May 2, 2024, paediatric occupational therapy based on a developmental approach was initiated. The treatment focused on therapeutic activities designed to improve the child’s range of motion, integrate muscle tone, and enhance coordination. Functional mobility retraining was provided, along with multisensory semi-structured activities and tactile-kinaesthetic retraining. The caregivers received comprehensive instructions to ensure continuity of care at home, and an Individualized Educational Program (IEP) was implemented as part of the therapeutic plan. While the patient made some progress towards achieving the treatment goals, these were only minimally achieved by the time of discharge due to the child’s inpatient status at Hamsa Rehab.
Recommendations and follow up report
On May 25, 2024, the inpatient was discharged from Paediatric Occupational Therapy with recommendations to continue both Physical and Occupational Therapy sessions five times per week. It was also advised that daily therapy should be maintained at home to support the child’s developmental progress and prevent regression. The therapy follow-up plan includes exercises aimed at enhancing range of motion, improving muscle tone, and promoting overall motor coordination. Ongoing follow-up care with the Physical Medicine and Rehabilitation (PMR) Department is recommended to monitor the child’s progress and make necessary adjustments to the treatment plan. This approach ensures the child continues to receive the benefits of structured therapeutic interventions up to the present time.
Research methodology
Research involves a series of steps using which the researcher may find out the solution to the selected problem in such a way that the solution helps in the future occupational therapy of management. The procedure using which the researcher goes about occupational therapist work of describing, explaining and predicting phenomena is called methodology. It comprises of the procedures used for generating, collecting, processing and analysing data.
Objectives of the Study
Paediatric occupational therapy plays an important role in the management of congenital muscular torticollis. However, it was observed from the literature review that studies analysing the occupational therapy between these two variables significant in determining success are very scarce. Therefore, the researcher from the existing research gap recognized the above research problem. Based on the research problem identified, the following research objectives were formulated.
- Developmental occupational therapists analyse Spatial Play, Range of motion, developmental milestones.
- Planning manpower and activity well-informed therapists.
- Development Profile as early as possible to help reverse or stop the progression of Upper and Lower extremity deformity
- Evaluation sensory profile-2 performance and credible on an ongoing basis.
- Structure commitment on Supportive Behaviour, Developmental millstones based.
| Population | Sampling size | Sample techniques | Study place | Variables | Duration of the period |
|---|---|---|---|---|---|
| Accessible population was adapted in this study. | subjective sampling | Purposive sampling, is a non-probability sampling technique was adapted. | The subjects were selected from Hamsa rehab centre, Unit of Kauvery Hospital, Trichy, Tamil Nadu. | Independent variables activity based configurational developmental approach Dependent variables | Total duration of the study was 6 weeks. |
Procedure of study
This non-probability experimental research conducted on children with Mitochondrial leukodystrophy for 6 weeks. In this study, one children and age group between 2.6 years were included. Initially; permission for doing research was received from the subject’s parents or caregiver by getting consent form. Then details such as name, age, sex, history of Mitochondrial leukodystrophy was taken by using assessment form and the procedure was explained to the parents or caregiver. Pre and Post test data were collected through Child Sensory Profile – 2, Manual muscle power test (MMT), Activity based configurational developmental profile (ABCD-Profile) and were examined using Spatial play Based occupational therapy interventions. The collected data were divided into two variables based on intervention. The Occupational therapy interventions plan based Activity Configuration Approach. Further, Research data were analyzed by calculating mean value, t value and p value.
Paediatric occupational therapy management on children with mitochondrial leukodystrophy-Session schedule
Intervention
Single subject will be taken in this study. The subjects will be selected from the age between 2.6 years with Mitochondrial leukodystrophy. The therapy was planned for 6 weeks. It will be at 45 min group session with the frequency of five days a week. Total of 08 treatment sessions (each session of 5 days/6 month) is planned for children.
Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking
Session schedule
| Week 1 | Warm-up | Main activities |
|---|---|---|
| Session 1: | Arm wake-up Chair-swing | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with Roll-over |
| Session 2: | Arm wake-up bed mobility activity | Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking |
| Session 3: | Arm wake-up T-swing | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation withNeck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with Roll-over |
| Week 2 | Warm-up | Main activities |
| Session 1: | Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking | |
| Session 2: | Football carrying stretch | Oro Motor Muscular Facilitation, Tactile Spinal Facilitation |
| Session 3: | Football carrying stretch | Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking |
| Week 3 | Warm-up | Main activities |
| Session 1: | Arm wake-up aerobics -jumping | Oro Motor Muscular Facilitation, Tactile Spinal Facilitation |
| Session 2: | Arm wake-up aerobics -jumping | Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking |
| Session 3: | Arm wake-up aerobics -jumping | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity -stair calming, kneeling, rollover |
| Week 4 | Warm-up | Main activities |
| Session 1: | Football carrying stretch | Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking |
| Session 2: | Football carrying stretch | Oro Motor Muscular Facilitation, Tactile Spinal Facilitation |
| Session 3: | Football carrying stretch | Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking |
| Week 5 | Warm-up | Main activities |
| Session 1: | Arm wake-up Pencil aerobics | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity -stair calming, kneeling, rollover |
| Session 2: | Arm wake-up aerobics -jumping | Partial Flexor head control, initiation of extensor, supine to prone, full extension of upper and lower extremity, elevation of neck, prone on hand, pulls to sit, Tetrad position, static standing, Dynamic walking |
| Session 3: | Arm wake-up aerobics -jumping | Oro Motor Muscular Facilitation, Tactile Spinal Facilitation |
| Week 6-8 | Main activities | |
| Session 1: | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity -stair calming, kneeling, rollover |
| Session 2: | Football carrying stretch | Neck rotation-disc swing, neck rotation visual stimulation, transfer activities, Feel the pressure multisensory stimulation with beg board activities, proprioception activity -stair calming, kneeling, rollover |
| Session 3: | Football carrying stretch | Oro Motor Muscular Facilitation, Tactile Spinal Facilitation |
Data collection or statistical analysis
This study used were collected the data of pre- and post-intervention. The entire statistical test was performed using statistical package for graph pad instate software version 3.1 respectively.
Table 1: Characteristic of data pre and post evaluation- Activity based configurational developmental profile (ABCD-Profile)
| Characteristic of data paired t-test | ABCD-Profile (pre-test performance) | ABCD-Profile (post-test performance) |
|---|---|---|
| Mean | 1.67 | 11.67 |
| standard deviation | 2.89 | 15.95 |
| Sample size components | 3 | 3 |
| The standard error (SE) means | 1.67 | 9.21 |
| 95% confidence interval | -35.98 | 15.98 |
Table 1 shows of pre-post-evaluation (ABCD-Profile)- of subject, mean values are 1.67 and 11.67, respectively standard deviation 2.89 and 15.95respectively mono sample size components 03, standard error of mean 1.67 and 9.21, 95% confidence interval -35.98 and 15.98, respectively.
Table 2. Characteristic of data pre and post evaluation- Activity based configurational developmental profile (ABCD-Profile)
| S. No. | Variable 1 | Variable 2 | P-value | t-value | Level of significance |
|---|---|---|---|---|---|
| 1 | Pre-test evaluation | Post-test evaluation | 0.3454 | 1.0687 | Not statistically 1 Pre-test evaluation Post-test evaluation 0.3454 1.0687 Not statistically Significant |
Table 2 shows that comparison between the pre-post-evaluation- ABCD-Profile of subject,‘t’ value is 1.0687 ‘p’ value is 0.3454, This difference is considered to be not statistically significant.

Fig. 2. Characteristic of data pre and post evaluation- Activity based configurational developmental profile (ABCD-Profile).
Table 3. Characteristic of data pre and post evaluation- manual muscle power grade test (MMT)left side
| Characteristic of data paired t-test | MMT left side (pre-test performance) | MMT left side (post-test performance) |
|---|---|---|
| Mean | 0.38 | 2.38 |
| standard deviation | 0.50 | 0.72 |
| Sample size components | 16 | 16 |
| The standard error (SE) means | 0.13 | 0.18 |
| 95% confidence interval | -2.45 | -1.55 |
Table 3 shows of pre-post-evaluation (MMT left side) of subject, mean values are 0.38and 2.38, respectively standard deviation 0.50 and 0.72 respectively sample size 16, standard error of mean 0.13 and 0.18, 95% confidence interval -2.45 and -1.55, respectively.
Table 4. Characteristic of data pre and post evaluation – Manual Muscle Grade Test (MMT) right side
| S. No. | Variable 1 | Variable 2 | P-value | t-value | Level of Significance |
|---|---|---|---|---|---|
| 1 | Pre-test evaluation | Post-test evaluation | 0.0001 | 9.1366 | Extremely statistically significant |
Table 4 shows that comparison between the pre-post-evaluation (MMT) right side of subject, ‘t’ value is 9.1366, ‘p’ value is 0.0001. This difference is considered to be extremely statistically significant.

Fig. 3. Characteristic of data pre and post evaluation (MMT) left side
Table 5. Characteristic of data pre and post evaluation- Manual muscle power grade test (MMT-right side)
| Characteristic of data paired t-test | MMT (pre-test performance) | MMT (post-test performance) |
|---|---|---|
| Mean | 0.44 | 2.00 |
| standard deviation | 0.51 | 0.63 |
| Sample size-components | 16 | 16 |
| The standard error (SE) means | 0.13 | 0.16 |
| 95% confidence interval | 1.98 | 1.15 |
Table 5 shows of pre-post-evaluation Manual muscle power grade test (MMT) of subject, mean values are 0.44 and 2.00, respectively standard deviation 0.51 and 0.63 respectively sample size 16, standard error of mean 0.13 and 0.16, 95% confidence interval -1.98 and -1.15, respectively.
Table 6. Characteristic of data pre and post evaluation- Manual muscle power grade test (MMT-right side)
| S. No. | Variable 1 | Variable 2 | P-value | t-value | Level of significance |
|---|---|---|---|---|---|
| 1 | pre-test evaluation | post-test evaluation | 0.0001 | 7.6787 | Extremely statistically significant |
Table 6: This shows that comparison between the pre-post-evaluation- Manual muscle power grade test (MMT)of subject, ‘t’ value is 7.6787 ‘p-value is 0.0001, This difference is considered to be extremely statistically significant.

Fig. 4. Characteristic of data pre and post evaluation – Manual muscle power grade test (MMT).
Table 7. Characteristic of data pre and post evaluation- Range of motion (ROM)
| Characteristic of data paired t-test | Range of motion (pre-test performance) | Range of motion (post-test performance) |
|---|---|---|
| Mean | 42.50 | 61.25 |
| standard deviation | 32.27 | 18.87 |
| Sample size | 1 | 1 |
| The standard error (SE) means | 16.14 | 9.44 |
| 95% confidence interval | -58.99 | 21.49 |
Table 7 shows of pre-post-evaluation (Range of motion)- of subject, mean values are 88.75 and 39.25, respectively standard deviation 42.50 and 61.25 respectively sample size 01, standard error of mean 16.14 and 9.44, 95% confidence interval -58.99 and 21.49, respectively.
Table 8. Characteristic of data pre and post evaluation – Range of motion
| S. No. | Variable 1 | Variable 2 | P-value | t-value | Level of Significance |
|---|---|---|---|---|---|
| 1 | Control pre-test evaluation | Control post-test evaluation | 02348 | 1.4828 | Not statistically significant |
Table 8 shows that comparison between the pre-post-evaluation- Range of motion of subject,‘t’ value is 4.3795 ‘p-value is 0.0220, This difference is considered to be statistically significant.
Fig. 5. Characteristic of data pre and post evaluation – Range of motion
Discussion
The present case study aimed to explore the effectiveness of an activity-based configurational developmental approach in managing mitochondrial leukodystrophy in children. Mitochondrial leukodystrophies are a rare group of neurodegenerative disorders that often present with significant developmental delays, motor dysfunction, and a broad range of neurological deficits. These disorders have a profound impact on the quality of life of affected children and their families, as treatment options are limited and focus primarily on symptom management.
In this case study, a two-year-old male child with a confirmed diagnosis of mitochondrial leukodystrophy received an occupational therapy intervention based on a developmental approach. The intervention was structured around activity-based configurational play, focusing on improving the child’s range of motion, muscle tone, coordination, and overall functional abilities. Specific strategies included therapeutic play, multisensory activities, and caregiver education to reinforce developmental skills at home.
The child demonstrated modest improvements in motor coordination, balance, and mobility over the course of treatment. Although progress was slower than anticipated, this is consistent with the nature of mitochondrial leukodystrophies, where neurodegeneration can limit the capacity for rapid improvement. The integration of a structured, activity-based approach allowed for an individualized, holistic treatment plan, targeting the child’s unique functional needs while providing a supportive environment for gradual developmental gains.
One of the most significant aspects of this intervention was the involvement of caregivers. Training parents and caregivers to continue therapeutic activities at home ensured that the child received ongoing support outside of formal therapy sessions, reinforcing skills and contributing to functional maintenance. In this context, the Activity-Based Configurational Developmental Approach served as a framework not only for direct child engagement but also for sustainable home-based care.
While the child showed improvements, challenges such as fluctuating energy levels, decreased stamina, and difficulties in maintaining progress during periods of metabolic crises were evident. These limitations highlight the need for an integrated, multidisciplinary care approach that includes medical management, therapeutic interventions, and caregiver support. This collaborative approach can help mitigate some of the physical and neurological complications associated with mitochondrial leukodystrophies.
Conclusion
This case study illustrates the potential benefits of an activity-based configurational developmental approach in managing mitochondrial leukodystrophy in children. While the disorder’s progressive nature poses challenges to treatment, the implementation of a structured, play-based occupational therapy intervention led to improvements in motor function and overall coordination. The emphasis on caregiver involvement and home-based support also played a crucial role in maintaining the child’s functional abilities.
The findings of this case suggest that a personalized, activity-based developmental approach, combined with regular follow-up and multidisciplinary support, can enhance the quality of life for children with mitochondrial leukodystrophy. However, more research is needed to evaluate long-term outcomes and to develop standardized protocols for therapeutic interventions in this population. Future studies should also explore the potential for integrating advanced rehabilitative technologies and pharmacological treatments to further improve outcomes for these children.
Reference
- M. Mahendran et al. Identification of occupational therapy domains for a new conceptual model of activity configuration approach strategies for paediatrics habituation and rehabilitation. 2020
- M. Mahendran. Effectiveness of rood’s approach based paediatric occupational therapy management: on children with congenital muscular torticollis. Kauverian Sci J. 2023;5(11).
- Vanderver A, Prust M, Tonduti D, Mochel F, Hussey HM, Helman G, Garbern J, Eichler F, Labauge P, Aubourg P, Rodriguez D. Case definition and classification of leukodystrophies and leukoencephalopathies. Mol Gen Metabol. 2015;114(4):494-500.
- Van der Knaap MS, Bugiani M. Leukodystrophies: a proposed classification system based on pathological changes and pathogenetic mechanisms. Acta Neuropathol. 2017;134:351-382.
- Kevelam SH, Steenweg ME, Srivastava S, Helman G, Naidu S, Schiffmann R, Blaser S, Vanderver A, Wolf NI, Van Der Knaap MS. Update on leukodystrophies: a historical perspective and adapted definition. Neuropediatrics. 2016;47(06):349-354.
- Vanderver A, Simons C, Helman G, Crawford J, Wolf NI, Bernard G, Pizzino A, Schmidt JL, Takanohashi A, Miller D, Khouzam A. Whole exome sequencing in patients with white matter abnormalities. Ann Neurol. 2016;79(6):1031-1037.
- Montaut S, Tranchant C, Drouot N, Rudolf G, Guissart C, Tarabeux J, Stemmelen T, Velt A, Fourrage C, Nitschké P, Gerard B. Assessment of a targeted gene panel for identification of genes associated with movement disorders. JAMA Neurol. 2018;75(10):1234-1245.
- Gordon-Lipkin E, Fatemi A. Current therapeutic approaches in leukodystrophies: a review. J Child Neurol. 2018;33(13):861-868.
- Bugiani M, van der Knaap MS. Childhood white matter disorders: much more than just diseases of myelin. Acta Neuropathol. 2017;134(3):329-330.

