Journal scan: A review of 15 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Margarida Lucas Rocha, Published April 3, 2024, N Engl J Med 2024; 390:1218.
Secondary Hypertrophic Osteoarthropathy

A 55-year-old woman with a 29-pack-year history of smoking presented with a 1.5-year history of pain in her fingers, wrists, hips, knees, and ankles. On physical examination, clubbing and slight thickening of the skin of the fingers and toes were noted (Panel A, right foot). There was mild tenderness on palpation of all her affected joints but no erythema or swelling. A cardiopulmonary examination was normal. Radiographs of the forearms, hands, femurs, tibia, and feet showed symmetric periostitis of the tubular bones (Panel B, right foot, arrows; Panel C, right ulna and radius, arrows). The combination of painful arthropathy, periostitis, and clubbing prompted consideration of hypertrophic osteoarthropathy. Hypertrophic osteoarthropathy is a syndrome that is characterized by thickening of the skin and expansion of the bone of the distal arms and legs and is often associated with lung cancer. A chest radiograph showed a large mass on the left side (Panel D), which was further characterized as an anterior mediastinal mass on subsequent computed tomography. A biopsy of the mass revealed poorly differentiated non–small-cell carcinoma. A final diagnosis of secondary hypertrophic osteoarthropathy due to non–small-cell lung cancer was made. Systemic chemotherapy was initiated, but the patient died of pneumonia 2 months later.
(2). Hsue VB, Patel V. A Coin in the Airway. N Engl J Med. 2024;390(13):e33. doi:10.1056/NEJMicm2312266
A Coin in the Airway
A healthy 14-year-old boy presented to the emergency department with a 6-hour history of hoarseness and difficulty swallowing after having accidentally swallowed a coin. On physical examination, the patient was breathing comfortably without stridor or drooling. Radiographs of the chest (Panel A, posteroanterior view) and neck (Panel B, lateral view) showed a rounded, radiopaque foreign object situated vertically within the subglottis (the region between the vocal cords and the trachea).

A diagnosis of foreign-body aspiration was made. Accidentally ingested foreign bodies usually end up in the esophagus. When aspirated into the airway by older children, foreign bodies typically lodge more distally than in this case (in the trachea or a mainstem bronchus), owing to gravity and the larger airway size. Airway foreign bodies — especially those in the trachea and larynx — necessitate immediate removal to reduce the risk of respiratory compromise. Rigid bronchoscopy was performed while the patient was under general anesthesia, and a U.S. quarter was visualized within the subglottis and removed with optical forceps (Panel C and Video 1). On reinspection of the airway, mild subglottic mucosal ulceration due to the mass effect of the coin was seen (Panel D, asterisks, and Video 2). After the procedure, the patient’s symptoms abated and he was discharged home.
(3). Marina Morgan et al, Group A beta-haemolytic streptococcal infection in childrenBMJ 2024; 385 doi: https://doi.org/10.1136/bmj-2023-077561 (Published 02 April 2024),BMJ 2024;385:e077561
What we need to know
Group A beta-haemolytic streptococcal (GAS) infections, including pharyngitis and more complex invasive infections, can be difficult to diagnose clinically
In December 2022, rates of invasive infection in the UK increased substantially, with a high number of children presenting with empyema
Suspect invasive infection, including necrotising fasciitis and streptococcal toxic shock-like syndrome, in any child who is unwell and presents with severe or disproportionate pain in the setting of recent varicella zoster virus or GAS infection.
Group A beta-haemolytic streptococci (GAS) are Gram positive bacteria resembling chains (“streptos”) of berries (“kokkus”) that colonise mucus membranes and damaged skin. They are spread by skin contact and respiratory droplets. People of all ages are susceptible, but especially children, pregnant women, and older adults. Invasive GAS (iGAS) refers to when GAS moves from “colonising” skin or mucosal surfaces, reaching normally sterile sites such as blood, cerebrospinal, synovial, or pleural fluids, or deep tissues.
(4). Prof Ole Haagen Nielsen, John Mark Gubatan, Kaija-Leena Kolho, Sarah Elizabeth Streett, Prof Cynthia Maxwell. Updates on the management of inflammatory bowel disease from periconception to pregnancy and lactation. The Lancet. 2024; 403(10433):1291-1303.
Summary
Inflammatory bowel disease (IBD) affects reproductive planning due to psychological effects and mechanical problems related to surgery. Children of people with IBD have an increased risk of about 10% if one parent has IBD and up to 33% if both parents have IBD.
The fertility of people with IBD is similar to the general population, but fertility might be reduced in individuals with active IBD, ileal pouch-anal anastomosis, or perianal Crohn’s disease.
Flaring disease during pregnancy increases complications, such as preterm birth.
Thus, disease management with appropriate medications can optimise outcomes.
As most medications have minimal fetal risks, people with IBD should be informed about the risks of stopping medications and the importance of maintaining remission.
A period of disease remission is advisable before pregnancy and could reduce the risks for both the pregnant person and the fetus.
Flexible endoscopy, intestinal ultrasound, and gadolinium-free magnetic resonance enterography are safe during pregnancy.
We provide state-of-the-art knowledge on the basis of the latest evidence to ensure successful pregnancy outcomes in controlled IBD.
(5). https://www.bbc.com/news/world-us-canada-68730159
May-Thurner syndrome
What is May-Thurner syndrome?
May-Thurner syndrome (MTS) is not necessarily dangerous in itself but can lead to complications and health risks.
It is a condition caused by a problem involving the right iliac artery, which carries blood to the right leg, and the left iliac vein, which returns blood from the left leg towards the heart.
These blood vessels naturally cross over each other in the pelvis. MTS results when the artery squeezes the vein, resulting in reduced blood flow in that vessel.
This may not lead to any symptoms at all, and some people do not know they have the condition, leading the US National Institutes of Health (NIH) to describe it as “clinically silent”.
But reduced blood flow can increase the risk of blood-clot formation. If a clot travels to the heart, lungs or brain it can cause a blockage with potentially fatal consequences.
MTS often presents itself through pain or cramp in a person’s arm or leg, accompanied by swelling or a discolouring of the skin. Veins can appear more pronounced.
Diagnosis may be confirmed following a CT scan, as was the case with Ms Boebert.
What causes it?
Wwomen between the ages of 20 and 45 who have given birth are also more likely to have May-Thurner syndrome.
How is the condition treated?
Many people with MTS do not seek treatment as the condition does not present them any problems that prompt them to do so.
Options available include inserting a stent that makes sure the compressed vein stays open. .
Other surgery may be considered to restore typical blood flow – for example by moving the artery that is compressing the vein, or by creating an entirely new route for the vein.
People with MTS experiencing blood clots may be given anticoagulants medication in an attempt to break those up.
Those with mild symptoms might be advised by their doctor to wear compression socks on their lower legs to improve blood flow.
(6). Yndigegn T, Lindahl B, Mars K, et al. Beta-Blockers after Myocardial Infarction and Preserved Ejection Fraction. N Engl J Med. 2024;390(15):1372-1381.
Abstract
Background
Most trials that have shown a benefit of beta-blocker treatment after myocardial infarction included patients with large myocardial infarctions and were conducted in an era before modern biomarker-based diagnosis of myocardial infarction and treatment with percutaneous coronary intervention, antithrombotic agents, high-intensity statins, and renin–angiotensin–aldosterone system antagonists.
Methods
In a parallel-group, open-label trial performed at 45 centers in Sweden, Estonia, and New Zealand, we randomly assigned patients with an acute myocardial infarction who had undergone coronary angiography and had a left ventricular ejection fraction of at least 50% to receive either long-term treatment with a beta-blocker (metoprolol or bisoprolol) or no beta-blocker treatment. The primary end point was a composite of death from any cause or new myocardial infarction.
Results
From September 2017 through May 2023, a total of 5020 patients were enrolled (95.4% of whom were from Sweden). The median follow-up was 3.5 years (interquartile range, 2.2 to 4.7). A primary end-point event occurred in 199 of 2508 patients (7.9%) in the beta-blocker group and in 208 of 2512 patients (8.3%) in the no–beta-blocker group (hazard ratio, 0.96; 95% confidence interval, 0.79 to 1.16; P=0.64). Beta-blocker treatment did not appear to lead to a lower cumulative incidence of the secondary end points (death from any cause, 3.9% in the beta-blocker group and 4.1% in the no–beta-blocker group; death from cardiovascular causes, 1.5% and 1.3%, respectively; myocardial infarction, 4.5% and 4.7%; hospitalization for atrial fibrillation, 1.1% and 1.4%; and hospitalization for heart failure, 0.8% and 0.9%). With regard to safety end points, hospitalization for bradycardia, second- or third-degree atrioventricular block, hypotension, syncope, or implantation of a pacemaker occurred in 3.4% of the patients in the beta-blocker group and in 3.2% of those in the no–beta-blocker group; hospitalization for asthma or chronic obstructive pulmonary disease in 0.6% and 0.6%, respectively; and hospitalization for stroke in 1.4% and 1.8%.
Conclusions
Among patients with acute myocardial infarction who underwent early coronary angiography and had a preserved left ventricular ejection fraction (≥50%), long-term beta-blocker treatment did not lead to a lower risk of the composite primary end point of death from any cause or new myocardial infarction than no beta-blocker use. (Funded by the Swedish Research Council and others;
(7). Antonelli J, Verhoye JP, Martins RP. Transient Monocular Blindness in a Man in His 30s. JAMA Cardiol. 2024;9(4):405
.Apatient in his 30s presented to the emergency department with transient monocular blindness but no cardiovascular symptoms. Cerebral magnetic resonance imaging was normal, and a transient ischemic attack (TIA) was diagnosed. Transthoracic echocardiography revealed a gigantic, dilated structure (Figure, A) corresponding to the ascending aorta, with severe stenotic type 0 bicuspid aortic valve. Computed tomography confirmed a massive, 122-mm ascending aortic dilation (3-dimensional reconstruction in Figure, B) with signs of prerupture, confined between the sternum and the spinal cord, compressing the left atrium. An urgent bioprosthetic Bentall surgery was performed.

Giant ascending aortic aneurysms, defined as exceeding 10 cm in diameter, are rare entities, especially in recent years due to the widespread use of echocardiography.1 Aortic dilatation may be asymptomatic for years and manifest at the time of a complication, such as a TIA. Transthoracic echocardiography should always be performed to rule out cardiac origin.
(8). Das P, Singh G. Central Cyanosis in Acquired Methemoglobinemia. N Engl J Med. 2024;390(14):1311

A 35-year-old man presented to the dermatology clinic with 4-day history of anxiety, insomnia, and resting tremor of the hands and feet. One month before presentation, the patient had begun taking multidrug therapy for leprosy, which included dapsone after he tested negative for glucose-6-phosphate dehydrogenase deficiency. On physical examination, bluish discoloration of the lips and tongue (Panel A) — a finding known as central cyanosis — was observed. Cyanosis is best detected in areas of the body where the epidermis is thin and blood supply is abundant, such as the ears, nose, lips, and oral mucus membranes. Central cyanosis should arouse concern for decreased arterial oxygen saturation or hemoglobin abnormalities. Assessment of arterial blood gas showed a partial pressure of oxygen (Pao2) of 96 mm Hg (reference range, 75 to 100) and an oxygen saturation of 84%. Owing to the discrepancy between the Pao2 and oxygen-saturation values (a finding known as a “saturation gap”), acquired methemoglobinemia from dapsone was suspected. Dapsone therapy was stopped, and supportive care was given. The methemoglobin level as assessed by an outside laboratory was 14% (reference range, 0 to 3). Two days after the initial presentation and discontinuation of dapsone therapy, the patient’s symptoms and cyanosis had resolved (Panel B).
(9). Yin H, Lu L. Evolution of Pyoderma Gangrenosum. N Engl J Med. 2024;390(14):e36.

A 32-year-old man presented to the rheumatology clinic with a 4-month history of recurrent abscesses and a 3-day history of a skin lesion on his face. The abscesses had developed in his kidney, spleen, liver, lung, and skin. During previous evaluations of the abscesses, cultures had been negative, and antimicrobial therapy had been ineffective. Tests for rheumatologic conditions and immunodeficiency had been negative. At the current presentation, the physical examination was notable for a skin ulcer with a violaceous border on the right lower portion of the face that had started as an umbilicated, tender papule (Panels A, B, and C are photographs from days 1, 2, and 3, respectively, taken by the patient; Panel D is a photograph from day 4, taken during the current presentation). The next day, the ulcer had enlarged (Panel E, day 5). Histopathological analysis of a skin-biopsy specimen obtained from the border of the lesion showed a diffuse neutrophilic infiltrate with no organisms. A colonoscopy showed no evidence of inflammatory bowel disease. A diagnosis of pyoderma gangrenosum associated with aseptic abscess syndrome — an autoinflammatory disorder — was made. Treatment with colchicine and a tapering course of an oral glucocorticoid was initiated. The skin lesion started to subside 1 day after the start of treatment (Panel F, day 6; Panel G, day 8; and Panel H, day 14). At the 3-month follow-up, the ulceration (Panel I) and abscesses had abated
(10). Chen B, Wei M. Aortic Coarctation. N Engl J Med. 2024;390(15):1420.

A 35-year-old man was referred to his primary care physician for evaluation of previously unknown hypertension that had been identified during a medical screening for his rugby team. The patient was asymptomatic. The blood pressure was 146/89 mm Hg in the left arm, 146/99 mm Hg in the right arm, 104/83 mm Hg in the left leg, and 109/90 mm Hg in the right leg. On physical examination, a radial–femoral delay was present. A chest radiograph showed notching of posterior ribs 3 through 8 (Panel A, arrows) and widened paratracheal stripes (Panel A, asterisks). Computed tomographic (CT) angiography of the chest revealed coarctation of the descending aorta, with the isthmus measuring 3 mm in diameter (reference range for the patient’s age and size, 18 to 25) (Panel B, arrow). CT angiography also showed extensive collateral arterial circulation in the soft tissues (Panels C and D, white arrows), along the trachea (which accounted for the paratracheal stripes seen on chest radiography) (Panel C, dashed box), and in the intercostal spaces (which accounted for the notching of the ribs seen on chest radiography) (Panel D, black arrows). A transthoracic echocardiogram showed left ventricular hypertrophy and a pressure gradient of 25 mm Hg across the coarctation. No other cardiac abnormalities were identified. Percutaneous stenting of the aortic coarctation was performed without complications. At a follow-up visit 1 month after the procedure, the patient’s blood pressure had improved. At a 3-month follow-up visit, repeat imaging showed a marked decrease in collateral arterial circulation.
(11). Carazo Casas C, Medina Gonzalez M. Hemotympanum with a Basilar Skull Fracture. N Engl J Med. 2024;390(15):e38.
A 15-year-old boy presented to the emergency department with a 1-hour history of hearing loss and pain in the left ear after he had tripped and fallen on the street, striking his head on the pavement. He reported a headache but no ear drainage, tinnitus, vertigo, nasal discharge, or vomiting. The physical examination was notable for mild swelling behind the left ear, with no bruising. An otoscopic examination of the left ear showed blood behind the tympanic membrane (Panel A). Rinne and Weber testing, as well as pure-tone audiometry, indicated the presence of mild conductive hearing loss in the left ear. The remainder of the neurologic examination was normal. Computed tomography of the head revealed fluid in the middle ear (Panel B, white arrow) and a longitudinal left temporal bone fracture (Panel B, black arrow), as well as separation of the occipitotemporal suture and pneumocephalus (Panel C, asterisk).

A final diagnosis of a basilar skull fracture resulting in hemotympanum was made. The patient was admitted for observation, serial neurologic examinations, and repeat imaging. At a follow-up visit 2 weeks after hospital discharge, his ear pain and hemotympanum had abated and his hearing had returned to normal
(12). Fischer K, Nazir Z, Valencia D. Man in His Sixth Decade of Life With Totally Occluded Abdominal Aorta (Leriche Syndrome). JAMA Cardiol. Published online April 17, 2024.
Cardiovascular Images
Aman in his sixth decade with a history of peripheral arterial disease, erectile dysfunction, nonischemic cardiomyopathy, and reported sciatica presented for evaluation of a recent right middle cerebral artery cerebrovascular accident with severe carotid stenosis. Cerebral angiography via femoral access was attempted but failed due to bilateral occlusive aortoiliac disease. Abdominal aorta computed tomography angiography (CTA) (Figure) showed total occlusion of the infrarenal abdominal aorta with collaterals from the superior mesenteric artery to the femoral arteries bilaterally, consistent with Leriche syndrome. The patient was a poor surgical candidate due to limited functional status and was treated with medical therapy. Leriche syndrome is a rare obliterative aortoiliac occlusive syndrome with unknown incidence.1 Presenting symptoms include a triad of claudication, erectile dysfunction, and decreased peripheral pulses.1 The patient’s sciatica was likely a gluteal claudication equivalent.
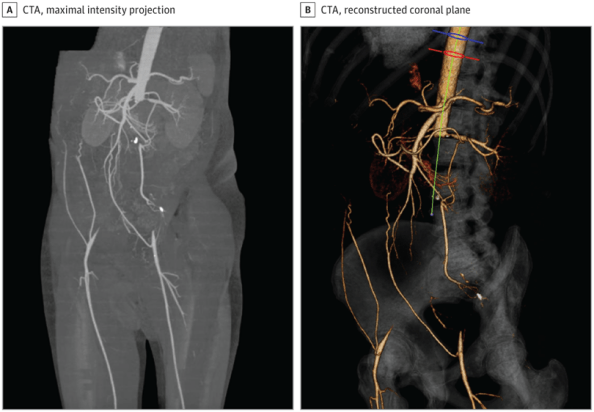
Computed tomography angiography (CTA) of the abdominal aorta with runoff showing Leriche syndrome. A, Maximal intensity projection showing total occlusion of the aorta and bilateral iliac arteries with normal runoff. B, Reconstructed coronal plane images showing total aortic occlusion.
(13). Bayes-Genis A, Gastelurrutia P, Monguió-Tortajada M, et al. Implantation of a double allogeneic human engineered tissue graft on damaged heart: insights from the PERISCOPE phase I clinical trial. EBioMedicine. 2024;102:105060.
Summary
Background
In preclinical studies, the use of double allogeneic grafts has shown promising results in promoting tissue revascularization, reducing infarct size, preventing adverse remodelling and fibrosis, and ultimately enhancing cardiac function. Building upon these findings, the safety of PeriCord, an engineered tissue graft consisting of a decellularised pericardial matrix and umbilical cord Wharton’s jelly mesenchymal stromal cells, was evaluated in the PERISCOPE Phase I clinical trial (NCT03798353), marking its first application in human subjects.
Methods
This was a double-blind, single-centre trial that enrolled patients with non-acute myocardial infarction eligible for surgical revascularization. Seven patients were implanted with PeriCord while five served as controls.
Findings
Patients who received PeriCord showed no adverse effects during post-operative phase and one-year follow-up. No significant changes in secondary outcomes, such as quality of life or cardiac function, were found in patients who received PeriCord. However, PeriCord did modulate the kinetics of circulating monocytes involved in post-infarction myocardial repair towards non-classical inflammation-resolving macrophages, as well as levels of monocyte chemoattractants and the prognostic marker Meteorin-like in plasma following treatment.
Interpretation
In summary, the PeriCord graft has exhibited a safe profile and notable immunomodulatory properties. Nevertheless, further research is required to fully unlock its potential as a platform for managing inflammatory-related pathologies.
(14).Sheth T, Morarji M, Jawaid I. Assessment of diplopia in adults. BMJ. 2024;385:e076413. Published 2024 Apr 23.
What you need to know
For a patient with double vision, differentiating between monocular and binocular diplopia can help guide the urgency of onward management
In an acute setting, for a patient with binocular diplopia and limited eye movements, the main differentials of concern are third, fourth, and six cranial nerve palsies. These should be urgently excluded.
Clinicians must be aware of leg
Double vision, or diplopia, may be the first sign of sight or life threatening pathology. A thorough, accurate first assessment is important for determining the clinical urgency of related pathology and ensuring timely management.
Monocular or binocular diplopia?
Whether diplopia is monocular or binocular will help identify aetiology and determine the urgency of management. Ensure double vision is distinguished from blurred vision (when a patient sees a single image that appears unclear), which has many other distinct causes. In diplopia, the second image may appear fainter as a “ghost” image.
Monocular diplopia refers to double vision originating solely from one eye. This will persist when the patient is asked to cover the other, unaffected eye and suggests an intraocular pathology. Differentials for monocular diplopia include refractive error, dry eye syndrome, corneal pathology, cataract, and non-urgent retinal pathology. In such cases, a routine optometrist or ophthalmology referral is appropriate for further evaluation.
Binocular diplopia is double vision present with both eyes open that resolves on covering either eye, and is more commonly encountered. This symptom is usually more serious as it indicates misalignment of the eyes, secondary either to ocular muscle pathology or a central neurological cause. Patients presenting acutely with this symptom should therefore be referred urgently for ophthalmic assessment and worked up appropriately.
(15). Fisher J, Matanhire-Zihanzu C, Buse K. A new approach to oral health can lead to healthier societies. BMJ. 2024;385:q925. Published 2024 Apr 23.
New definitions of oral health provide an opportunity to change mindsets and promote innovation to tackle high levels of unmet needs, but this will only be realised with a radical change in practice, argue Julian Fisher and colleagues
More than 3.5 billion people globally suffer from the main oral diseases. These conditions combined have an estimated global prevalence of 45%—higher than any other non-communicable disease. A major barrier to improving this situation is our approach to oral health.
The prevailing mindset is that oral health is synonymous with dentistry and that poor oral health has little impact on personal and societal health and wellbeing.
We need to shift away from the idea that the prevention and control of certain oral diseases equates to overall oral health and instead move to a broader and more inclusive understanding.
Expanded definitions of oral health from the World Health Organization and FDI World Dental Federation are transformational and can help realise a model for sustainable oral health put forward by the US National Academy of Medicine.
The academy proposes that oral health is influenced by a wide range of biological, psychosocial, and spiritual perspectives and external social, economic, and environmental factors.
This new narrative takes our understanding of oral health beyond the confines of disease and positions it in terms of personal confidence, wellbeing, and arising from and contributing to healthy societies more broadly. This narrative can herald a sea change for action in practice.
WHO recognises that oral health enables people to perform essential functions. Orofacial structures are central to breathing and speaking. Oral health is linked to diet quality and adequate fluid intake which influences a person’s microbiome and their gut health. This is also important to our understanding of the gut-brain axis and the implications for mental health. Smiling and conveying a range of emotions through facial expressions is central to wellbeing and the ability to socialise and work. The mouth is central to our senses of smell, taste, and touch, which allows us to connect to our environment. The craniofacial complex is an integral part of the musculoskeletal system with implications for balance, gait, and mobility. In short, good oral health equates with wellbeing on a personal level.
Oral health is everyone’s job. Improving it will require an expanded oral health workforce that should include physicians, nurses, midwives, pharmacists, social workers, dietitians, community health workers, speech language pathologists, and other health providers, as well as non-traditional providers such as civic and religious leaders and teachers. Oral health is already embedded in the universal health coverage agenda. Strengthening and scaling up oral health education and training as part of universal health coverage would enable an enlarged oral health workforce to integrate new knowledge, skills, and attitudes for oral health into their practice and daily routines. In this way oral health could be monitored and maintained over the life course with a focus on patient centred concerns and outcomes.This pivot would increase “oral health touch points” with children and families at all income levels, for example, for early detection of oral cancers and tobacco and alcohol interventions for patients at high risk.
Taking action on the social determinants of oral health inequity is at the heart of radical action to end the neglect of oral health. Poor oral health disproportionately affects low income and other marginalised members of societies. Hierarchies of power, money, and resource distribution for oral health services continue to reinforce inequities, including through the continued biomedical dental approach, which both directly and indirectly influence oral health outcomes, particularly for disadvantaged people. Ensuring oral health for all requires an approach involving the whole of government and society, including fixing broken food systems whose marketing, advertising, and sale of products contribute to poor oral health.Actions could include implementing health taxes, particularly taxation of food and beverages with high free sugars content, and avoiding sponsorship by related companies for public and sports events. Done right, oral health can play a major role in creating healthy societies.

