Journal scan: A review of 30 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Ruben Jauregui et al. Idiopathic Intracranial Hypertension. N Engl J Med 2023;389:2467
A 25-year-old woman with severe obesity presented to the emergency department with a 1-week history of blurred vision, transient visual obscurations, daily headaches, and intermittent whooshing sounds.
Her body-mass index (the weight in kilograms divided by the square of the height in meters) was 57.
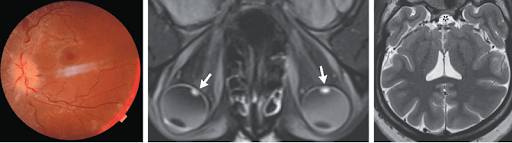
On neurologic examination, optic-disk swelling and retinal hemorrhages were present in both eyes (Panel A, left eye).
The results of visual-field and cranial-nerve testing were normal. Magnetic resonance imaging and venography of the head revealed flattened posterior globes with marked elevation of the optic-nerve heads (Panel B, arrows), an empty sella (Panel C, asterisk), and stenoses of the transverse sinuses without obstruction or thromboses all of which were suggestive of elevated cerebrospinal fluid pressure.
A lumbar puncture was notable for an elevated opening pressure of 55 cm of water (reference range, 10 to 20); the results of the cerebrospinal fluid analysis were normal.
A diagnosis of idiopathic intracranial hypertension was made.
Idiopathic intracranial hypertension is a disorder associated with obesity that manifests with symptoms resulting from increased intracranial pressure, including headaches, diplopia, visual field defects, and pulsatile tinnitus.
Treatment with high-dose acetazolamide was started, and counseling on weight loss was provided.
At a 1-month follow-up visit, the patient’s papilledema had decreased, and treatment with acetazolamide had been continued.
(2). Ying Gao et al, or the INSPIRES Investigators. Dual Antiplatelet Treatment up to 72 Hours after Ischemic Stroke. ,N Engl J Med 2023; 389:2413-2424
Abstract
Background
Dual antiplatelet treatment has been shown to lower the risk of recurrent stroke as compared with aspirin alone when treatment is initiated early (-24 hours) after an acute mild stroke. The effect of clopidogrel plus aspirin as compared with aspirin alone administered within 72 hours after the onset of acute cerebral ischemia from atherosclerosis has not been well studied.
Methods
In 222 hospitals in China, we conducted a double-blind, randomized, placebo-controlled, two-by-two factorial trial involving patients with mild ischemic stroke or high-risk transient ischemic attack (TIA) of presumed atherosclerotic cause who had not undergone thrombolysis or thrombectomy. Patients were randomly assigned, in a 1:1 ratio, within 72 hours after symptom onset to receive clopidogrel (300 mg on day 1 and 75 mg daily on days 2 to 90) plus aspirin (100 to 300 mg on day 1 and 100 mg daily on days 2 to 21) or matching clopidogrel placebo plus aspirin (100 to 300 mg on day 1 and 100 mg daily on days 2 to 90). There was no interaction between this component of the factorial trial design and a second part that compared immediate with delayed statin treatment (not reported here). The primary efficacy outcome was new stroke, and the primary safety outcome was moderate-to-severe bleeding both assessed within 90 days.
Results
A total of 6100 patients were enrolled, with 3050 assigned to each trial group. TIA was the qualifying event for enrollment in 13.1% of the patients. A total of 12.8% of the patients were assigned to a treatment group no more than 24 hours after stroke onset, and 87.2% were assigned after 24 hours and no more than 72 hours after stroke onset. A new stroke occurred in 222 patients (7.3%) in the clopidogrel aspirin group and in 279 (9.2%) in the aspirin group (hazard ratio, 0.79; 95% confidence interval [CI], 0.66 to 0.94; P=0.008). Moderate-to-severe bleeding occurred in 27 patients (0.9%) in the clopidogrel aspirin group and in 13 (0.4%) in the aspirin group (hazard ratio, 2.08; 95% CI, 1.07 to 4.04; P=0.03).
Conclusions
Among patients with mild ischemic stroke or high-risk TIA of presumed atherosclerotic cause, combined clopidogrel aspirin therapy initiated within 72 hours after stroke onset led to a lower risk of new stroke at 90 days than aspirin therapy alone but was associated with a low but higher risk of moderate-to-severe bleeding. (Funded by the National Natural Science Foundation of China)
(3). Rheault MN, Alpers CE, Barratt J, Bieler S, Canetta P, Chae DW, et al,. DUPRO Steering Committee and DUPLEX Investigators. Sparsentan versus Irbesartan in Focal Segmental Glomerulosclerosis. N Engl J Med. 2023 Dec 28;389(26):2436-2445
Abstract
Background
An unmet need exists for focal segmental glomerulosclerosis (FSGS) treatment. In an 8-week, phase 2 trial, sparsentan, a dual endothelin angiotensin receptor antagonist, reduced proteinuria in patients with FSGS. The efficacy and safety of longer-term treatment with sparsentan for FSGS are unknown.
Methods
In this phase 3 trial, we enrolled patients with FSGS (without known secondary causes) who were 8 to 75 years of age; patients were randomly assigned to receive sparsentan or irbesartan (active control) for 108 weeks. The surrogate efficacy end point assessed at the prespecified interim analysis at 36 weeks was the FSGS partial remission of proteinuria end point (defined as a urinary protein-to-creatinine ratio of -1.5 [with protein and creatinine both measured in grams] and a >40% reduction in the ratio from baseline). The primary efficacy end point was the estimated glomerular filtration rate (eGFR) slope at the time of the final analysis. The change in eGFR from baseline to 4 weeks after the end of treatment (week 112) was a secondary end point. Safety was also evaluated.
Results
A total of 371 patients underwent randomization: 184 were assigned to receive sparsentan and 187 to receive irbesartan. At 36 weeks, the percentage of patients with partial remission of proteinuria was 42.0% in the sparsentan group and 26.0% in the irbesartan group (P=0.009), a response that was sustained through 108 weeks. At the time of the final analysis at week 108, there were no significant between-group differences in the eGFR slope; the between-group difference in total slope (day 1 to week 108) was 0.3 ml per minute per 1.73 m2 of body-surface area per year (95% confidence interval [CI], &1.7 to 2.4), and the between-group difference in the slope from week 6 to week 108 (i.e., chronic slope) was 0.9 ml per minute per 1.73 m2 per year (95% CI, &1.3 to 3.0). The mean change in eGFR from baseline to week 112 was &10.4 ml per minute per 1.73 m2 with sparsentan and &12.1 ml per minute per 1.73 m2 with irbesartan (difference, 1.8 ml per minute per 1.73 m2; 95% CI, &1.4 to 4.9). Sparsentan and irbesartan had similar safety profiles, and the frequency of adverse events was similar in the two groups.
Conclusions
Among patients with FSGS, there were no significant between-group differences in eGFR slope at 108 weeks, despite a greater reduction in proteinuria with sparsentan than with irbesartan. (Funded by Travere Therapeutics)
(4). Alexei Buruian et al. Stepladder Dislocation of the Finger. December 30, 2023, DOI: 10.1056/NEJMicm2302974

A 54-year-old woman presented to the emergency department with a crooked, painful finger after she had fallen backward onto her outstretched hand 1 hour earlier. On physical examination, dorsal displacement of the right fifth ( pinky ) finger was noted at the proximal and distal interphalangeal joints. The patient was unable to move the finger. There were no signs of neurovascular compromise. Radiographs of the right hand showed dorsal dislocation of the proximal and distal interphalangeal joints of the fifth finger, which created a stepladder shape (Panel A, lateral view; Panel B, posteroanterior view). A diagnosis of simultaneous dislocation of the proximal and distal interphalangeal joints of the fifth finger was made. Although dislocation of an interphalangeal joint is commonly seen, simultaneous dislocations within the same finger are rare. Treatment with closed reduction and splinting of the finger was provided. Three weeks after reduction, the splint was removed and the patient was counseled to resume an active range of motion with the finger without weight-bearing for 4 additional weeks. At the 6-month follow-up, the patient had full function of the finger.
(5). Simon B. Drysdale et al. Nirsevimab for Prevention of Hospitalizations Due to RSV in Infants. , N Engl J Med 2023; 389:2425-2435,
Abstract
Background
The safety of the monoclonal antibody nirsevimab and the effect of nirsevimab on hospitalizations for respiratory syncytial virus (RSV) associated lower respiratory tract infection when administered in healthy infants are unclear.
Methods
In a pragmatic trial, we randomly assigned, in a 1:1 ratio, infants who were 12 months of age or younger, had been born at a gestational age of at least 29 weeks, and were entering their first RSV season in France, Germany, or the United Kingdom to receive either a single intramuscular injection of nirsevimab or standard care (no intervention) before or during the RSV season. The primary end point was hospitalization for RSV-associated lower respiratory tract infection, defined as hospital admission and an RSV-positive test result. A key secondary end point was very severe RSV-associated lower respiratory tract infection, defined as hospitalization for RSV-associated lower respiratory tract infection with an oxygen saturation of less than 90% and the need for supplemental oxygen.
Results
A total of 8058 infants were randomly assigned to receive nirsevimab (4037 infants) or standard care (4021 infants). Eleven infants (0.3%) in the nirsevimab group and 60 (1.5%) in the standard-care group were hospitalized for RSV-associated lower respiratory tract infection, which corresponded to a nirsevimab efficacy of 83.2% (95% confidence interval [CI], 67.8 to 92.0; P<0.001). Very severe RSV-associated lower respiratory tract infection occurred in 5 infants (0.1%) in the nirsevimab group and in 19 (0.5%) in the standard-care group, which represented a nirsevimab efficacy of 75.7% (95% CI, 32.8 to 92.9; P=0.004). The efficacy of nirsevimab against hospitalization for RSV-associated lower respiratory tract infection was 89.6% (adjusted 95% CI, 58.8 to 98.7; multiplicity-adjusted P<0.001) in France, 74.2% (adjusted 95% CI, 27.9 to 92.5; multiplicity-adjusted P=0.006) in Germany, and 83.4% (adjusted 95% CI, 34.3 to 97.6; multiplicity-adjusted P=0.003) in the United Kingdom. Treatment-related adverse events occurred in 86 infants (2.1%) in the nirsevimab group.
Conclusions
Nirsevimab protected infants against hospitalization for RSV-associated lower respiratory tract infection and against very severe RSV-associated lower respiratory tract infection in conditions that approximated real-world settings. (Funded by Sanofi and AstraZeneca)
(6). Shirong Cai et al, Clonorchis sinensis Liver Flukes. N Engl J Med 2023; 389:e57.
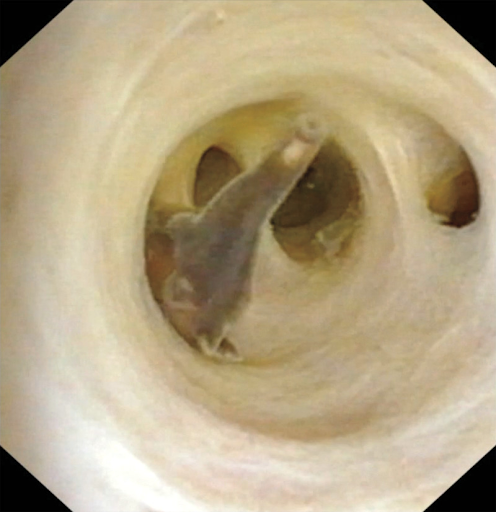
A 70-year-old man undergoing cholangioscopy was found to have flatworms in his biliary tract. One week before the procedure, the patient had received a diagnosis of localized sigmoid adenocarcinoma. After computed tomography of the abdomen revealed choledocholithiasis, dilatation of the common bile duct, and no distant metastases, plans had been made for laparoscopic tumor resection, cholecystectomy, and cholangioscopy. During the cholangioscopy, five large flatworms were seen wriggling in the biliary tract (see video). Two worms were extracted and identified as Clonorchis sinensis a type of liver fluke. C. sinensis is endemic in East Asia. Infection occurs as a result of eating raw or undercooked freshwater fish or shrimp. After larvae are ingested, they emerge from cysts in the duodenum, ascend the biliary tree, and mature into adult worms in the biliary tract, gallbladder, or liver. Most acute infections are asymptomatic. Chronic infection may be complicated by cholangiocarcinoma, a condition that was not present in this patient. The infection is typically diagnosed by identification of parasite eggs in a stool sample, although this patient’s stool tested negative. After the flatworms were removed, treatment with praziquantel was administered, and adjuvant chemotherapy for sigmoid adenocarcinoma was initiated.
(7). Julio Rosenstock et al. Weekly Icodec versus Daily Glargine U100 in Type 2 Diabetes without Previous Insulin. ,N Engl J Med 2023; 389:297-308
Abstract
Background
Insulin icodec is an investigational once-weekly basal insulin analogue for diabetes management.
Methods
We conducted a 78-week randomized, open-label, treat-to-target phase 3a trial (including a 52-week main phase and a 26-week extension phase, plus a 5-week follow-up period) involving adults with type 2 diabetes (glycated hemoglobin level, 7 to 11%) who had not previously received insulin. Participants were randomly assigned in a 1:1 ratio to receive once-weekly insulin icodec or once-daily insulin glargine U100. The primary end point was the change in the glycated hemoglobin level from baseline to week 52; the confirmatory secondary end point was the percentage of time spent in the glycemic range of 70 to 180 mg per deciliter (3.9 to 10.0 mmol per liter) in weeks 48 to 52. Hypoglycemic episodes (from baseline to weeks 52 and 83) were recorded.
Results
Each group included 492 participants. Baseline characteristics were similar in the two groups. The mean reduction in the glycated hemoglobin level at 52 weeks was greater with icodec than with glargine U100 (from 8.50% to 6.93% with icodec [mean change, &1.55 percentage points] and from 8.44% to 7.12% with glargine U100 [mean change, &1.35 percentage points]); the estimated between-group difference (&0.19 percentage points; 95% confidence interval [CI], &0.36 to &0.03) confirmed the noninferiority (P<0.001) and superiority (P=0.02) of icodec. The percentage of time spent in the glycemic range of 70 to 180 mg per deciliter was significantly higher with icodec than with glargine U100 (71.9% vs. 66.9%; estimated between-group difference, 4.27 percentage points [95% CI, 1.92 to 6.62]; P<0.001), which confirmed superiority. Rates of combined clinically significant or severe hypoglycemia were 0.30 events per person-year of exposure with icodec and 0.16 events per person-year of exposure with glargine U100 at week 52 (estimated rate ratio, 1.64; 95% CI, 0.98 to 2.75) and 0.30 and 0.16 events per person-year of exposure, respectively, at week 83 (estimated rate ratio, 1.63; 95% CI, 1.02 to 2.61). No new safety signals were identified, and incidences of adverse events were similar in the two groups.
Conclusions
Glycemic control was significantly better with once-weekly insulin icodec than with once-daily insulin glargine U100. (Funded by Novo Nordisk)
(8). Ming Juan Liu et al. Necrobiosis Lipoidica. DOI: 10.1056/NEJMicm2304653, NEJM 04 Jan 24
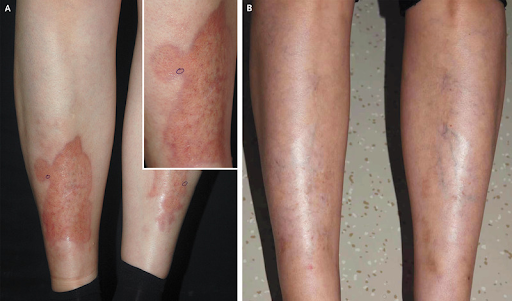
A 43-year-old woman presented to the dermatology clinic with an 8-year history of yellow-brown spots on her shins. The lesions had been asymptomatic, and she had not sought care for them until they had grown in size. She had no history of diabetes mellitus, hypertension, or thyroid disease.
On physical examination, atrophic yellow-brown plaques with telangiectasias and irregular violaceous borders were observed on both shins (Panel A and inset). A skin biopsy of the right shin was performed. Histopathological analysis showed several layers of necrobiosis within the dermis, perivascular inflammatory-cell infiltrates, collagen degeneration, and findings consistent with granulomatous dermatitis. A diagnosis of necrobiosis lipoidica was made. Necrobiosis lipoidica is a chronic granulomatous skin disorder that is frequently associated with diabetes and may precede the development of impaired glucose control. However, the condition is also seen in persons without diabetes, as occurred in this patient, who had normal results on glycemic testing. There are no evidence-based guidelines for treatment, and the lesions often abate on their own. In this case, topical glucocorticoids were administered, but the patient discontinued treatment after 1 month owing to minimal improvement and concerns about side effects. At follow-up performed 13 years after the patient’s initial visit, the plaques had resolved (Panel B) and her glycemic control remained normal.
(9). Mehmet A. Elbey et al. Foreign-Body Aspiration in an Older Patient. https://doi.org/10.7326/aimcc.2023.0186
We present a case of a 68-year-old man with a history of heavy smoking and HIV infection, who displayed concerning symptoms. Initial imaging suggested a possible malignancy. This unique presentation underscores the significance of thorough patient history-taking in reaching accurate diagnoses, especially in complex cases that initially mimic more common conditions.
Case
A 68-year-old man with a history of heavy smoking was admitted for nonproductive cough, anorexia, and nearly 50 lbs of weight loss in the last 3 months. His past medical history was significant for HIV while undergoing antiretroviral therapy maintaining a normal CD4 count. Additionally, he has been diagnosed with chronic obstructive pulmonary disease, and unprovoked pulmonary embolism. Upon examination, the patient’s oxygen saturation level was 96% on room air, while the right chest exhibited reduced air entry. Radiograph of the chest showed dense consolidation in the middle of the right lung (Figure 1A). Computed tomography (CT) of the chest revealed a large consolidation of the right lobe with an abrupt cutoff with a suspected mass concerning malignancy (Figure 1B). A completely obstructing endobronchial lesion was found proximally at the orifice of the right main bronchus in the bronchoscopy (Figure 1C). Biopsy demonstrated predominantly foreign structures, histologically most consistent with the vegetable matter with no evidence of malignancy. When the patient was asked retrospectively, he reported an aspiration episode while eating due to poor dentures, and his symptoms slowly started afterward. However, he did not seek medical attention following the aspiration episode. A 6-month follow-up by CT showed near-complete healing of the right lung (Figure 1D). The patient reported resolution of all symptoms in a 2-year follow-up.
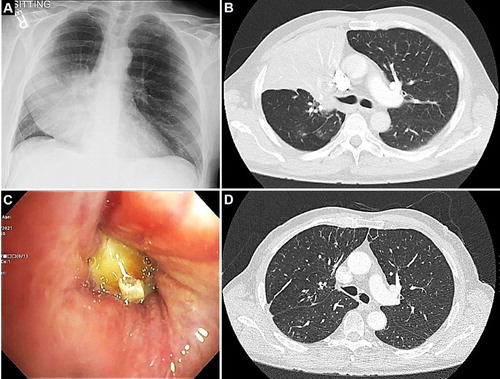
Figure 1. (A) The chest radiograph shows dense consolidation in the middle and upper lobes of the right lung. (B) Computed tomography of the chest with contrast shows a large consolidation of the right lobe consolidation, abrupt cutoff, and a suspected malignant mass. (C) Bronchoscopy reveals a fully obstructing endobronchial lesion near the orifice of the right main bronchus. (D) Follow-up computed tomography at 6 months demonstrates significant near-complete healing of the right lung.
This case highlights a rare and atypical presentation that initially raised strong suspicion of an underlying malignancy, considering the patient’s long-standing HIV infection, history of heavy smoking, and imaging findings. However, findings ultimately demonstrated that the obstructive lesion was secondary to poorly chewed food material, emphasizing the importance of comprehensive and detailed patient history-taking.
(10). The Lancet. Treating obesity and diabetes: drugs alone are not enough. Lancet. 2024 Jan 6;403(10421):1
Pharmacological agents capable of causing loss of up to a quarter of bodyweight are likely to be available soon.
There is cautious optimism for patients.
The costs of these drugs is a live question.
Weight loss is only maintained while taking the drugs; once treatment stops, weight can be regained, and so the costs of chronic treatment, for both individuals and health systems, could be substantial.
Obesity is a product of not only an individual’s circumstances and behaviour, but also society at large, shaped by global food markets and trade agreements. Multidimensional approaches are needed to curb the effects of the obesogenic environment, particularly against an international industry that promotes overproduction of cheap food and drinks. Physical activity needs to increase; walking and cycling for journeys to work or school should be normalised and made easier and safer. Sugar taxes and curbs on marketing of high-energy, high-fat, ultra-processed foods need to be implemented.
Prevention must be the foundation upon which everything else follows.
(11). Jetanat Chantrapitak et al. Papular Purpuric Gloves and Socks Syndrome in Parvovirus B19 Infection. N Engl J Med 2024; 390:165.
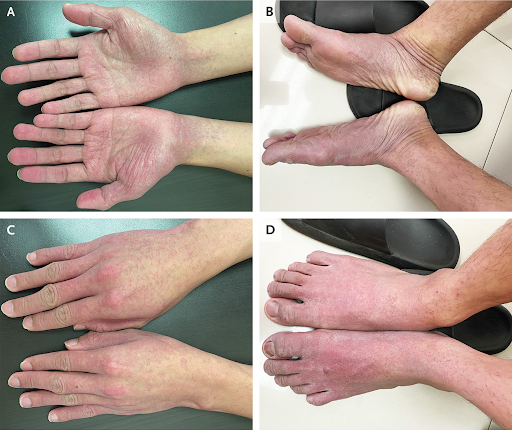
A 26-year-old man presented to the dermatology clinic with a 1-week history of an asymptomatic rash on his hands and feet. He also reported having had a fever which had resolved 6 days before presentation but no joint pains or oral lesions. Physical examination was notable for scattered, partially blanchable macules around the wrists and ankles that merged into erythematous patches on the ventral (Panels A and B) and dorsal (Panels C and D) surfaces of the hands and feet. No skin changes were observed on the cheeks or elsewhere. A serum B19 IgM antibody test and a polymerase-chain-reaction assay were positive for parvovirus. A diagnosis of papular purpuric gloves and socks syndrome in the context of parvovirus B19 infection was made. The classic rash associated with parvovirus B19 infection is a slapped cheek pattern on the face, but other distributions of rashes may be seen. The acral rash seen in papular purpuric gloves and socks syndrome most commonly manifests in adolescents and adults. Despite the name of the syndrome, the skin lesions may be petechial or macular. The patient was reassured about the self-limited nature of the viral infection. One week later, the rash had abated.
(12). Yang Kee Chan. Vocal-Cord Polyp Causing Airway Obstruction. N Engl J Med 2024; 390:e4,DOI: 10.1056/NEJMicm2307437
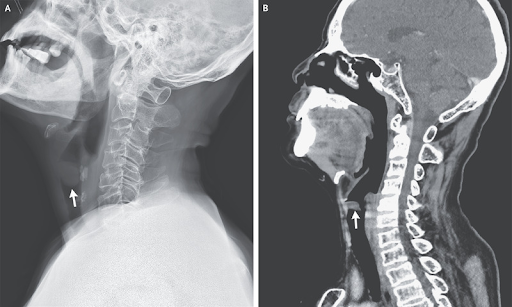
A 69-year-old man presented to the emergency department with a 2-week history of progressive, intermittent dyspnea that worsened when he was lying down. He also reported a 2-year history of hoarseness and a 30-pack-year smoking history. He worked in a noisy factory and frequently yelled to communicate with coworkers. On physical examination, there were normal inspiratory breath sounds and loud expiratory wheezes that were heard best over the neck. Owing to concern for upper-airway obstruction, radiography and computed tomography of the neck were performed, both of which showed a mass causing partial obstruction of the upper airway (Panels A and B, respectively, arrows). Bronchoscopy was subsequently performed, during which a large vocal-cord polyp was found to be causing intermittent airway obstruction in a ball-valve fashion during expiration (see video). Vocal-cord polyps commonly manifest with hoarseness. Such polyps result from chronic irritation of the vocal cords, such as from smoking, reflux, or vocal strain. Immediately after bronchoscopic polypectomy, the patient’s dyspnea resolved. Histopathological analysis confirmed the lesion to be a benign vocal-cord polyp. At the 1-month follow-up, his voice had returned to normal. Counseling on smoking cessation and vocal-strain avoidance was given.
(13). Alves L. Brazil to start widespread dengue vaccinations. Lancet. 2024 Jan 13;403(10422):133.
Brazil becomes the first country to include Qdenga in its public health system
Brazil plans to vaccinate millions of people against dengue after becoming the first country to incorporate Qdenga, manufactured by Japan’s Takeda Pharma
Infection by dengue virus, transmitted by Aedes aegypti mosquitos, has surged in recent years, with many blaming higher temperatures and prolonged rainy seasons.
Brazil’s Health Ministry has approved vaccination following the authorisation of Qdenga for people aged 4 60 years. Our hope is that this arbovirus becomes a vaccine-preventable disease , says Ethel Maciel, Secretary of Health for Brazil’s Ministry of Health.
Brazil has been fighting the dengue virus for at least four decades. It’s been four decades of a war, in which the virus has been winning ,
Not only are we losing this war, but the number of deaths is increasing, which shows the ineffectiveness of the conventional strategies we are using, which is combating the vector
The clinical trials of Qdenga vaccine have produced very encouraging results. The vaccine reduced asymptomatic dengue and mild dengue by around 70% and mitigated the risk of severe dengue, which requires hospitalisation, and even death, by 80 90%.
And as for the risk of side-effects, as seen with the other vaccine on the market, Dengvaxia, it is low.
When widely used in the Philippines, Dengvaxia was found to increase the risk of severe dengue in people who had never previously been infected, meaning that testing for past infection is now required before immunisation.
Such testing is not needed for Qdenga. For this vaccine, it is not necessary to test individuals to find out if they have had dengue before, because the technology is different .
The Qdenga vaccine covers the four serotypes of the disease, but clinical trials of the vaccine were conducted in locations where serotypes 3 and 4 are not common. It is important to remember that we do not know very much about protection and security in relation to dengue serotype 4 ,
The health department will track those taking the vaccine for possible side-effects and efficiency. We will monitor those taking the vaccine in a phase 4 clinical study, as should be done in incorporations for pharmacovigilance analysis .
Takeda will only be able to deliver five million doses of Qdenga this year, starting in February. Considering that it is a two-dose vaccine, health agents will be able to immunise approximately 2.5 million people in 2024. Brazil, however, has a population of more than 160 million people eligible to receive the vaccine. According to Maciel, the priority groups for vaccination will be defined by the National Immunization Program
We are considering taking 1 or 2 years at most. For example 6 7 years old or 11 12 years old. If we only take the WHO recommendation, vaccinating everyone between 6 16 years old, this population in Brazil represents 58 million individuals. At the moment that is undoable ,
The city of Dourados, in Mato Grosso do Sul state, has already become the first in the world to start mass vaccination with Qdenga,
Dengue control has so far largely relied on vector control, using insecticides and larvicides. Dengue numbers clearly show that our main tool, vector control, is not effective in reducing the number of cases in urban regions with high density, as is the case in poor communities ,.
Health experts agree that no one strategy is 100% effective and that a combination of all strategies is our best chance to reduce dengue contamination and transmission. What we are trying today is precisely the combination of several strategies. We’re talking about control, not eradication. We are trying to maintain a lower density [of mosquitos carrying dengue virus] ,
The dengue battle is multifactorial. There will not be a single tool that will truly reduce the problem of the disease. We need to continue carrying out vector control, eventually with more effective tools associated with vaccination .
(14). Antonio Landi et al. Coronary embolisation of native aortic valve debris during transcatheter aortic valve replacement: mechanical embolectomy and histopathological analysis. The Lancet. 2024;403(10422):117-218.
An 86-year-old woman with severe symptomatic aortic stenosis reporting progressive dyspnoea, rated as Class II on the New York Heart Association Functional Classification, for the previous few months had a transcatheter aortic valve replacement (TAVR) in our unit. The patient’s valve was replaced with an aortic valve bio prosthesis (Evolut PRO/PRO+ 29 mm [Medtronic Evolutâ„¢]).
Immediately after the valve had been replaced, continuous electrocardiogram monitoring showed ST-segment elevation in all antero-septal leads. A coronary angiogram showed complete occlusion of the distal part of the left anterior descending artery.
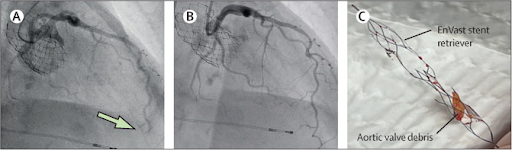
We then did a mechanical embolectomy using a stent retriever (enVast 4.5  37 mm [enVast™]) combined with vacuum-assisted aspiration which resulted in the immediate restoration of blood flow in the blocked artery; no residual material was seen in the vessel on repeat angiography (figure 1).
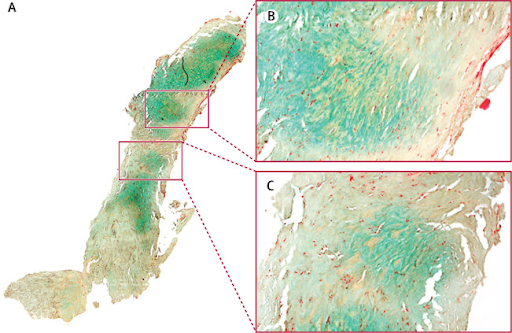
The extracted material was amber-coloured, calcified, and 2 mm in size; histopathological examination showed that it was mostly composed of collagen, proteoglycans, and extracellular matrix compatible with a fragment of a leaflet from the patient’s original aortic valve (figure 2). Additionally, substrates appeared non-birefringent under polarised light, confirming the absence of polymer-coated device fragments.
The patient’s chest pain promptly resolved; concentration of high-sensitivity troponin peaked at 24 h (202 ng/L; normal value <14). The patient remained asymptomatic for 1 day after the operation.
On day 2 postoperatively, she developed severe abdominal pain; an abdominal CT scan showed patency of both the superior and inferior mesenteric arteries with radiological signs of intestinal ischaemia. The patient had abdominal surgery which was complicated by multiple-organ failure; she died 4 days after the index TAVR.
Embolisation of aortic valve debris is a feared complication during TAVR, typically resulting in cerebrovascular accidents, and mesenteric or peripheral ischaemia. Histological analysis of captured material from cerebral protective devices has previously been done.
To the best of our knowledge, this is the first report showing that embolisation of aortic valve debris confirmed by histological examination into coronary circulation can be extracted with a stent retriever. Coronary embolisation during TAVR is unpredictable and no effective preventive measures exist; conventional angioplasty is often unsuccessful because of the presence of the calcified, non-friable material inside the vessel.
(15). John L. Sapp et al, for the RAFT Long-Term Study Team. Long-Term Outcomes of Resynchronization Defibrillation for Heart Failure. , N Engl J Med 2024; 390:212-220
Abstract
Background
The Resynchronization Defibrillation for Ambulatory Heart Failure Trial (RAFT) showed a greater benefit with respect to mortality at 5 years among patients who received cardiac-resynchronization therapy (CRT) than among those who received implantable cardioverter defibrillators (ICDs). However, the effect of CRT on long-term survival is not known.
Methods
We randomly assigned patients with New York Heart Association (NYHA) class II or III heart failure, a left ventricular ejection fraction of 30% or less, and an intrinsic QRS duration of 120 msec or more (or a paced QRS duration of 200 msec or more) to receive either an ICD alone or a CRT defibrillator (CRT-D). We assessed long-term outcomes among patients at the eight highest-enrolling participating sites. The primary outcome was death from any cause; the secondary outcome was a composite of death from any cause, heart transplantation, or implantation of a ventricular assist device.
Results
The trial enrolled 1798 patients, of whom 1050 were included in the long-term survival trial; the median duration of follow-up for the 1050 patients was 7.7 years (interquartile range, 3.9 to 12.8), and the median duration of follow-up for those who survived was 13.9 years (interquartile range, 12.8 to 15.7). Death occurred in 405 of 530 patients (76.4%) assigned to the ICD group and in 370 of 520 patients (71.2%) assigned to the CRT-D group. The time until death appeared to be longer for those assigned to receive a CRT-D than for those assigned to receive an ICD (acceleration factor, 0.80; 95% confidence interval, 0.69 to 0.92; P=0.002). A secondary-outcome event occurred in 412 patients (77.7%) in the ICD group and in 392 (75.4%) in the CRT-D group.
Conclusions
Among patients with a reduced ejection fraction, a widened QRS complex, and NYHA class II or III heart failure, the survival benefit associated with receipt of a CRT-D as compared with ICD appeared to be sustained during a median of nearly 14 years of follow-up.
(16). Yu-Kun Zhao et al. Pubic Lice. N Engl J Med 2024; 390:e6,
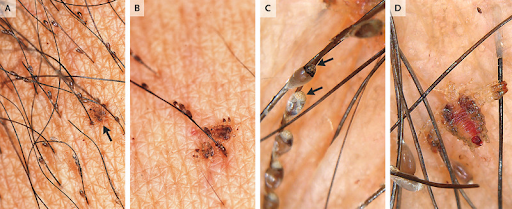
A 59-year-old man presented to the dermatology department with a 4-week history of severe itching in his pubic region. Sixteen weeks before presentation, he had had sexual contact with a new partner.
On physical examination, small, brown nits (Panel A) and mobile, crab-shaped lice (Panel A [arrow] and Panel B) were seen attached to the shafts and bases, respectively, of pubic hairs. No lice were seen elsewhere on the body. Dermoscopic examination showed nits that had a cap, or operculum, at one end (Panel C, arrow) and six-legged lice ingesting blood (Panel D and video). A diagnosis of pubic lice was made.
Pubic lice (Phthirus pubis) are parasites that are most commonly transmitted through sexual contact. The life cycle of the organism involves stages as a nit (or egg), nymph, and adult louse. An adult louse will die within 48 hours without a blood feeding. Treatment with topical lindane the only lice-killing medication available locally was given. Testing for syphilis, human immunodeficiency virus infection, and gonorrhea was negative.
The patient was also advised to wash his clothing and bedsheets in hot water and to avoid sexual contact until treatment was successful. One week after treatment was completed, his itching had abated.
(17). Nisha Desai et al. Early Diagnosis to Prevent Carbon Monoxide Poisoning Complications. 16 January 2024. https://doi.org/10.7326/aimcc.2023.0360,
Abstract
Carbon monoxide (CO) is a toxic gas with undetectable features. Every year in the United States, there are approximately 6000 deaths from CO poisoning. Patients usually present with signs of unresponsiveness but may have nonpathognomonic preceding symptoms. Some literature shows benefits of hyperbaric oxygen therapy (HBOT) within the first 24 hours of exposure to reduce the incidence of myocardial injury and neurologic impairment. This case report presents a 67-year-old man with CO poisoning who developed delayed neurologic sequelae (DNS) due to delayed diagnosis and missed therapeutic window for HBOT. Investigation of CO poisoning requires taking a detailed history to avoid delays in diagnosis and treatment.
Background
Carbon monoxide (CO) is a highly toxic gas characterized as tasteless, odorless, colorless, and nonirritating. These indistinguishable characteristics make CO toxicity difficult to identify. Common sources of CO production include motor vehicles, faulty heaters, gas-powered generators, propane stoves, and charcoal grills. Carbon monoxide poisoning is the cause of approximately 40000 emergency department (ED) visits and 6000 deaths per year in the United States. Patients often arrive unresponsive with other general preceding symptoms, including headaches, dizziness, nausea, vomiting, chest pain, and confusion. Some studies have shown that hyperbaric oxygen therapy (HBOT) provides the greatest therapeutic outcome if initiated within the first 24 hours of exposure. Hyperbaric oxygen therapy (HBOT) improves oxygenation by displacing the strongly bound carboxyhemoglobin from heme in the blood.
Objective
A good history and a broad differential diagnosis are crucial to ascertaining the diagnosis of CO poisoning. The condition of CO toxicity is often underdiagnosed and is detected specifically via an elevated carboxyhemoglobin level. Early treatment with HBOT can avoid serious myocardial and neurologic damage.
Case Report
A 67-year-old man with a history of hypercholesterolemia and active smoking presented via emergency medical services (EMS) for unresponsiveness. A history was obtained from his wife who reported the patient went to sleep at his baseline but was unarousable in the morning. She did not report any seizure-like activity, bowel or bladder incontinence, tongue biting, drug use, or alcohol use. On arrival, vital signs were stable and the patient showed no signs of airway compromise. On physical examination, he became more alert, was able to follow simple commands, and was able to answer questions by nodding. Besides the delayed responses and aphasia, the rest of the physical examination was unremarkable. Laboratory results were clinically significant for elevated troponin levels of 2.45 nmol/L (0-0.15 nmol/L) which peaked at 7.29 nmol/L. The remainder of work-up, including urine drug screen, alcohol test, urinalysis, complete blood count (CBC), comprehensive metabolic panel (CMP), arterial blood gas (ABG), lactic acid, and electrocardiogram (ECG), were unremarkable. The computed tomography (CT) of the head, angiogram of the head and neck, and video encephalogram were also unremarkable. On further investigation the next day, the patient’s wife reported the patient was fixing a leak in the heater the day before the episode and had disconnected the carbon monoxide detectors because of their constant beeping. He slept in the same room that night. His wife, who slept in a different room, later recalled experiencing symptoms of headaches and vomiting herself a day before. The detailed history and possibility of CO poisoning with a faulty heater in winter months prompted further investigation. The carboxyhemoglobin (COHb) and methemoglobin (MetHb) profile showed an elevated carboxyhemoglobin level of 5.0% (reference rage, 1.5% to 5.0%), an oxyhemoglobin level of 83% (reference range, 94% to 98%), and an oxygen (O2) saturation level of 87%. Supplemental O2 was administered to the patient. Hyperbaric oxygen therapy (HBOT) was deferred because of the patient’s improved mental status, normal pH level, and carboxyhemoglobin level of less than 25%. Magnetic resonance imaging (MRI) of the brain showed bilateral globus pallidus ischemia associated with CO poisoning. An echocardiogram showed new findings of concentric hypertrophy with mildly reduced ejection fraction of 40% to 45% and grade 1 diastolic dysfunction. The patient at baseline was fully functional and independent with no neurologic deficits. However, after the exposure to CO, he developed residual deficits with delayed cognitive communication, memory, and word-finding. During a 6-month follow-up call, the patient reported he has been receiving outpatient speech therapy and has shown minor improvements but has not yet returned to his baseline.
Discussion
Carbon monoxide is a gas produced by incomplete combustion. Sources include smoke inhalation from fires, faulty furnaces, motor vehicles in poorly ventilated areas, hookah waterpipe use, and underground electrical cable fires (1). Carbon monoxide is rapidly absorbed by the lungs and has a 240-fold affinity to heme than that of oxygen. The high affinity of CO to heme reduces the ability of oxygen to offload to peripheral tissues. Oxidative stress mediates injury to vital organs, primarily the myocardium and the brain (2).
The undetectable characteristics of CO make the diagnosis of toxicity difficult. Therefore, the diagnosis requires taking a detailed history. Signs and symptoms of CO poisoning present nonspecifically as nausea, vomiting, headaches, and dizziness. Patients will commonly arrive unresponsive or in a comatose state during winter months. Carbon monoxide poisoning accounts for 40000 ED visits per year with a mortality rate of 1% to 3% (2). If survived, the effects of the poisoning can lead to permanent cognitive and motor impairments, and myocardial damage. Delayed neurologic sequelae (DNS) is a serious complication caused by acute CO poisoning that can occur within several days to weeks after recovery from acute CO poisoning. It manifests as depression, memory issues, ataxia, behavioral changes, and impaired cognitive function (3). It is important to identify patients at risk for developing DNS associated with acute toxicity because it can affect treatment options.
Making a timely diagnosis is fundamental in the decision to administer high oxygen concentrations. In order to offset the high affinity of CO to heme, oxygenation promotes faster displacement of CO correlating directly to the level of concentration. For example, HBOT can drastically decrease the half-life of CO to 30 minutes compared to 90 minutes with a nonrebreather with high flow nasal cannula (4).
The decision to treat a patient with acute CO poisoning with HBOT is controversial. Several randomized retrospective studies show treatment with HBOT within 24 hours of CO poisoning reduces the incidence and sequelae of cognitive impairment (5 8). Despite inconclusive literature available about the role of HBOT, treatment with HBOT should be considered in such individuals, if no contraindications are present, to avoid cognitive and motor deficits.
Some physicians find it reasonable to treat with HBOT regardless of severity of poisoning because it is difficult to predict which patients will develop DNS (9). Other physicians treat with HBOT based on patient presentation of loss of consciousness on arrival, new neurologic deficits, mental status change, end organ ischemia associated with EKG changes, pH level less than 7.1, or pregnancy (10). Assessing the benefits and risks of HBOT is the driving factor for choice of treatment.
In this case report, we presented a 67-year-old man with a delayed diagnosis of CO poisoning with normal vital signs and initial laboratory findings. The initial presentation led to a broad variation of differential diagnosis. Indistinguishable characteristics of the gas, lack of common laboratory tests hinting the diagnosis of CO toxicity, and poor history taking can all make the diagnosis of CO poisoning difficult. In our patient, after further investigation, the family was able to hint to exposure to CO due to recent furnace work. This crucial information prompted further investigation of CO toxicity. The decision was made to continue with normobaric O2 instead of HBOT because of the delayed diagnosis and improvement in the patient’s symptoms. The increased hypoxemia and lipid peroxidation likely resulted in the bilateral globus pallidus ischemia (Figure 1), which is frequently seen in patients with CO poisoning. In general, the diagnosis of DNS is also difficult to make because it manifests with a lucid interval, which can cause a delay in the treatment with HBOT. Perhaps if the diagnosis of CO toxicity was made earlier, HBOT could have been initiated within 24 hours of exposure and DNS could have been avoided.
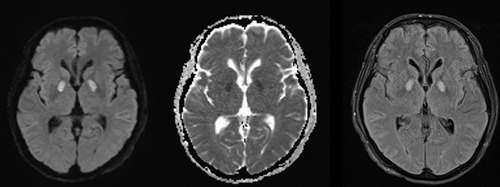
Figure 1. Magnetic resonance imaging of the brain showing bilateral globus pallidus ischemia with surrounding edema often seen in patients with carbon monoxide poisoning.
On initial presentation to the ED in cases of unresponsiveness, it is important to consider CO poisoning in the differential diagnosis, especially in cold weather months and based on a patient’s social history. Hyperbaric oxygen therapy should be considered a gold standard treatment of CO poisoning unless a contraindication is present.
(18). Rebecca C. Olsen, et al. Staphylococcus saprophyticus, an Unusual Cause of Pyelonephritis and Sepsis in Pregnancy. https://doi.org/10.7326/aimcc.2023.0613
Abstract
Maternal sepsis accounts for 13% of U.S. maternal deaths, with an estimated 2.2 deaths per 100000 live births. Early identification and treatment are critical in sepsis. Maternal sepsis is often a polymicrobial condition. Common causative agents include Escherichia coli, Group B Streptococcus, anaerobes, and Staphylococcus aureus. Staphylococcus saprophyticus is a rare cause of pyelonephritis-associated sepsis in immunocompetent patients and is especially uncommon during pregnancy. Only a handful of cases are reported in the literature, with only 2 cases associated with pregnancy. The case being presented describes an adolescent gravid patient who was diagnosed with pyelonephritis-associated sepsis caused by S saprophyticus.
Background
In the United States, maternal sepsis accounts for 13% of maternal deaths, with an estimated 2.2 deaths per 100 000 live births (1). Early identification and treatment are critical in sepsis. During pregnancy, the maternal immune response is compromised to protect the fetus but can predispose pregnant patients to infection (1). Maternal sepsis can occur due to obstetric causes such as chorioamnionitis, after invasive procedures, or from nonobstetric causes such as pyelonephritis or pneumonia (1). In the setting of pregnancy, sepsis is often a polymicrobial condition. Common causative agents include Escherichia coli, Group B Streptococcus, anaerobes, and Staphylococcus aureus (2).
Objective
Staphylococcus saprophyticus is a rare cause of pyelonephritis-associated sepsis, especially uncommon during pregnancy (3). Only a handful of cases are reported in the literature, with only 2 cases associated with pregnancy. Treatment of this bacterial infection during pregnancy can be challenging, as many preferred antibiotics may be deleterious to the fetus. Here, we present a case of an adolescent gravid patient who was diagnosed with pyelonephritis-associated sepsis caused by S saprophyticus and discuss our rationale for treatment.
Case Report
A 17-year-old girl G2P1001 at 20 weeks and 1 day gestation by last menstrual period presented to the emergency department for acute-onset right flank pain that migrated to the right lower quadrant. Her pain was described as severe and worsening. Associated symptoms included nausea. She did not report any hematuria, dysuria, vaginal bleeding, leakage of fluid, or contractions. On examination, vital signs revealed a fever of 103.3 °F, blood pressure 115/73 mm Hg, and tachycardia (heart rate 153 beats/min). She had right midabdominal and flank tenderness on examination, with the presence of a gravid abdomen.
Initial laboratory values (Table 1) revealed leukocytosis with a left shift, high inflammatory markers, and acute kidney injury due to oliguria. Urinalysis findings were suggestive of a urinary tract infection (UTI) based on the presence of leukocytosis and hematuria, but the sample was likely contaminated, as multiple organisms were isolated.
Table 1. Patient Laboratory Values and Reference Ranges
Value Reference Range
Leukocytes 17.1 103/L (H) 4.0 11.0 103/L
Hgb 10.9 g/dL (L) 12.0 16.0 g/dL
Hct 32.1% (L) 36.0 48.0%
Platelet 383 103/L 130 400 103/L
Absolute neutrophil count 15.4 103/mm3 (H) 1.8 8.0 103/mm3
Neutrophil auto % 90.0% (H) 36.0% 66.0%
Creatinine 0.5 mg/dL 0.5 1.0 mg/dL
CRP 77.31 mg/L (H) -3.01 mg/dL
Lactic acid 1.2 mmol/L 0.5 2.2 mmol/L
CRP = C-reactive protein; H = high; Hct = hematocrit; Hgb = hemoglobin; L = low.
Abdominal ultrasound revealed the presence of right hydroureteronephrosis, a common physiologic finding in pregnancy. Magnetic resonance imaging was performed, as to avoid use of computed tomography, to better visualize the urinary tract for any mechanical blockages that may have required emergency drainage (4) and to rule out appendicitis, given the patient’s presenting symptoms. Magnetic resonance imaging results confirmed the finding and indicated that the hydroureteronephrosis terminated at the level of the gravid uterus. Obstetrician-gynecologist specialists evaluated the patient and determined that the pregnancy was viable; the fetal heart rate was 163 beats/min without evidence of decelerations.
The patient was given ceftriaxone in the emergency department and admitted to the pediatric intensive care unit for sepsis due to presumed pyelonephritis. Antibiotics were broadened to include piperacillin/tazobactam and vancomycin, due to concerns for early sepsis and after early growth of gram-positive cocci in blood and urine cultures. A unilateral percutaneous nephrostomy tube was placed for hydronephrosis decompression. Final blood and urine culture from nephrostomy placement results were positive for S saprophyticus. Infectious disease specialists were consulted due to limited agents available for treatment without deleterious fetal effects. Infectious disease discontinued vancomycin and restarted ceftriaxone, 2 g intravenously, every 24 hours, based on antibiotic sensitivity results (Table 2). The patient was treated for 2 weeks with intravenous ceftriaxone through home infusion with a peripherally inserted central catheter line and fully recovered.
Table 2. Antimicrobial Sensitivity
Drug Staphylococcus saprophyticus
Interpretation Minimum Inhibitory Concentration Dilution (MDIL)
Gentamicin Sensitive -0.5
Oxacillin Sensitive 0.5
Rifampin Sensitive -0.5
Vancomycin Sensitive -0.5
Discussion
S saprophyticus is an extremely rare cause of bacteremia-related pyelonephritis in immunocompetent patients. Only a handful of cases have been reported in the literature, with only 2 cases associated with pregnancy (both cases were published in the 1980s). S saprophyticus is a gram-positive, novobiocin-resistant, coagulase-negative cocci. It is the second leading cause of acute uncomplicated UTIs in young, sexually active women (5), with Escherichia coli being most common (6). The bacteria are commonly part of normal flora within the female genital tract, urethra, and rectum (6) and have virulence factors, such as hemagglutinin, that facilitate attachment to the urogenital epithelium (5). During urinary tract obstruction, virulence factors enable the bacteria to ascend to the kidney, where it can cause pyelonephritis. (5) The virulence factor catalase deactivates hydrogen peroxide, protecting it from bactericidal activities of reactive oxygen metabolites. Notably, the bacteria have low virulence and pathogenicity in blood because they lack coagulase and ATPase, which allow for growth in low potassium environments such as blood (5).
For uncomplicated UTIs, nitrofurantoin or trimethoprim sulfamethoxazole (TMP-SMX) may be used. TMP-SMX should be avoided in the first trimester of pregnancy, as it can cross the placenta and potentially affect cleft palate development and cause neural tube or cardiac defects due to trimethoprim’s activity as a folate antagonist (7). Sulfamethoxazole is not recommended after 32 weeks of gestation due to concerns of causing kernicterus (7). As S saprophyticus is an uncommon cause of bacteremia originating from the urinary tract, the treatment of this condition is not well established, especially during pregnancy. One case of S saprophyticus bacteremia in a healthy, young woman was successfully treated with a course of vancomycin and daptomycin (5). In general, S saprophyticus is reported to be sensitive to vancomycin, daptomycin, and linezolid (8), although some strains can form biofilms, which can exacerbate antibiotic resistance (6). However, increasing resistance to ampicillin, ceftriaxone, cephalexin, ciprofloxacin, and even possible resistance against vancomycin has been reported (6). In patients infected with resistant S saprophyticus strains, the recommended treatment is linezolid (6). Previously reported cases of S saprophyticus bacteremia associated pyelonephritis in the literature were treated with various antibiotic regimens with duration of therapy ranging from 7 to 21 days. It is recommended that treatment be guided by antimicrobial sensitivity within the local area (5). All reports in the literature achieved full recovery without complications (5).
The 2 cases of S saprophyticus bacteremia occurring during pregnancy reported in the literature received different antibiotic treatments. One case that occurred at 26 weeks of gestation originated from a UTI and was successfully treated with 3 days of intravenous cefazolin followed by oral cephalexin, 500 mg every 6 hours, for an unspecified length of time (9). The second report was in a woman at 15 weeks of gestation that originated from pyelonephritis with a predisposing factor of ureteric calculus and was successfully treated with a 12-day course of amoxicillin (10). It is important to identify the bacteria causing sepsis primarily for appropriate treatment of the mother. If the uterus is the source of infection, delivery of the fetus is indicated; otherwise, it is generally recommended that pregnancies continue without intervention (11).
S saprophyticus is an unusual cause of pyelonephritis-associated sepsis, especially in gravid patients. Treatment of this bacterial infection during pregnancy can be challenging, as many preferred antibiotics such as TMP-SMX can be deleterious to the fetus. Duration of treatment is not well defined, and antibiotic selection should be guided by local antimicrobial sensitivity data. In the present case, the patient was treated with intravenous ceftriaxone both in the hospital and for 2 weeks after discharge, but linezolid is recommended if the clinical isolate demonstrates broad antibiotic resistance.
(19). Marion Larue et al. Pericardial Abscess in an Immunocompromised Patient. https://doi.org/10.7326/aimcc.2023.0300
A 44-year-old woman treated with corticosteroids and methotrexate for mixed connective tissue disease was hospitalized for lower limb edema and chest pain. Imaging studies revealed a large pericardial abscess with spondylodiscitis. Blood cultures were positive for methicillin-sensitive Staphylococcus aureus (MSSA). Pairwise genomes comparison done on both the responsible strain and an MSSA strain isolated 3 months earlier in a context of catheter-related infraclinical blood stream infection revealed identical patterns, highlighting the probable silent evolution of an incompletely treated infection in a patient receiving corticosteroids.
Case Report
A 44-year-old woman was hospitalized for lower limb edema and progressive chest pain. Three months earlier, she presented with inflammatory myositis, discoid lupus, pericarditis, and pleural effusion. Mixed connective tissue disease was diagnosed. Treatment with corticosteroids and methotrexate resulted in a complete disappearance of symptoms. At admission, she had no fever, and clinical examination was unremarkable except for lower limb edema. Computed tomography (CT) scan showed a limited pericardial collection (Figure 1A and B), and T5-T6 spondylodiscitis (Figure 1C) confirmed on spine magnetic resonance imaging (MRI) (Figure 1D). Blood cultures were positive to MSSA. Repeated transthoracic and transesophageal echocardiograms confirmed the pericardial abscess without further involvement and excluded cardiac dysfunction and infective endocarditis. Corticosteroid dosages were tapered and methotrexate was withdrawn. The patient improved after 6 weeks of intravenous cefazolin and drainage of the pericardial abscess. She has remained well for 6 months without relapse.
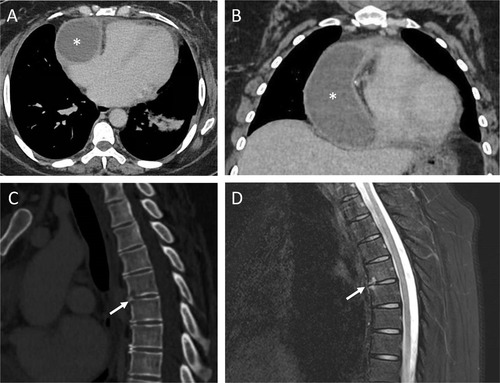
Figure 1. Thoracic CT scan (A and B) showed a limited pericardial collection (70 67 110 mm 18 Hounsfield unit) (asterisk). Thoracoabdominal CT scan (C) and magnetic resonance imaging (D) of the thoracic spine showed erosions of T5 and T6, suggestive of spondylodiscitis (arrow). CT = computed tomography.
The genomes of both the responsible MSSA strain and another strain isolated 3 months earlier during a catheter-related blood stream infection were compared, revealing identical patterns and suggesting a silent dissemination of an incompletely treated infection in a patient receiving corticosteroids.
Methicillin-sensitive Staphylococcus aureus has been reported to colonize approximately 30% of the human population (1). It causes various symptoms with a mortality rate between 15% and 30% for bloodstream infections (1, 2). While immunosuppressive agents were not associated with higher mortality (3), methotrexate and corticosteroids were probably responsible for the silent bacterial dissemination in our patient. Reduction of immunosuppression was proposed to favor infection control and limit postoperative complications.
(20). Caitlin Trottier et al. Maggots: Antimicrobial Stewards and Life Savers. https://doi.org/10.7326/aimcc.2023.0693.
Abstract
Maggots have been used in wound care for centuries.
Their larvae secrete digestive enzymes and antimicrobial compounds that reduce the bacterial load within a wound and promote the growth of new, healthy tissue.
We will discuss a series of patients with complex, nonhealing and life-threatening sacral wounds who developed multidrug-resistant sacral osteomyelitis.
These wounds had failed to respond to standard and advanced strategies.
Medicinal maggots were offered as a last-ditch effort in each case. In addition to saving the patients’ lives, these maggots demonstrated their underappreciated and underused role as antimicrobial stewards.
Background
Medicinal maggots can be used as potential adjunctive therapy and in certain situations as the main therapy for the management of decubitus ulcers and sacral osteomyelitis. They demonstrate promising antimicrobial properties and assist in the recovery of complex wounds that are nonresponsive to standard-of-care therapies, as discussed in this narrative.
Objective
Amidst the challenges of nonhealing, life-threatening sacral wounds, the unconventional use of medicinal maggots has unveiled a surprising and life-saving salvage therapy. This narrative explores this avenue in further detail.
Case Reports
Case 1
A 66-year-old man with a medical history significant for morbid obesity, chronic bilateral lower-extremity edema, seizure disorder, and alcohol dependence disorder was transferred to our hospital after a mechanical fall, with head injury and prolonged downtime complicated by rhabdomyolysis. On admission, he was noted on physical examination to have multiple traumatic injuries including a large 15 30-cm-deep tissue injury on his buttock, sacrum, and coccyx that evolved into a stage 4 pressure injury with exposed bone, tendon, and muscle (Figure 1). Magnetic resonance imaging of the sacrum and pelvis demonstrated associated bony erosion consistent with osteomyelitis. Initial tissue cultures grew an extended-spectrum beta lactamase producing Enterobacter cloacae. Despite the infusion of intravenous ertapenem, the wound deteriorated to 15 21 4 cm in the setting of fecal incontinence and poor nutrition. He had a diverting colostomy and additional debridement with repeat deep tissue cultures including culture from the exposed necrotic bone, which now was growing multidrug-resistant (MDR) Escherichia coli, for which he was started on ceftazidime avibactam. Despite fecal diversion, aggressive wound care with Dakin’s packing 3 times a day, followed by negative-pressure wound therapy, systemic antibiotics, and complete offloading with the Envella sand bed (Hill-Rom Holdings), the wound continued to worsen, with ongoing necrosis of the deep tissues.
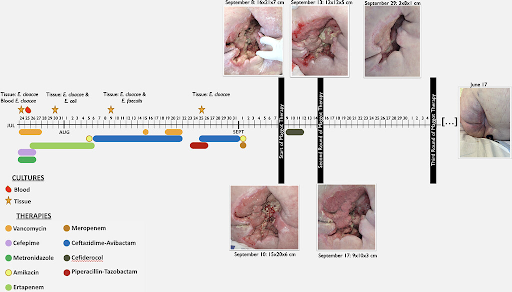
Figure 1. Timeline of evolution of sacral wound with treatment modalities used. Before and after use of maggot therapy showing dramatic recovery and complete resolution of the wound.
Two months into management and after 6 operative debridements, the wound measured 16 21 7 cm, and the surgical teams determined further surgical intervention was futile. With each debridement, the wound only became larger, and it never demonstrated granulation tissue. Palliative care was recommended, given no further operative options, and the MDR organism was only susceptible to nephrotoxic agents, which perpetuated renal failure. The patient was now dialysis-dependent. The medical and surgical teams believed palliative care was the only option, given his extreme deconditioning, comorbid conditions, and perceived unlikelihood that the wound would ever be able to close. The patient did not want to die and asked the wound care team for any other options. After extensive multidisciplinary meetings, it was decided, under the guidance of the wound care team, to attempt salvage therapy with inpatient maggot biodebridement for the first time in decades at our institution. The thought was that the maggots could remove the rapidly reaccumulating necrotic tissue while reducing bacterial bioburden and stimulating granulation tissue and hopefully the start of wound closure. It was his only hope for survival.
He subsequently had 3 rounds of maggot therapy with rapid, sequential decrease in the volume of the wound, increased granulation tissue formation, and clearance of the MDR infection, allowing for cessation of the cytotoxic systemic antimicrobials and hemodialysis. After 20 days, the third and final round of maggots was deployed and at the time of maggot retrieval, the wound measured 8 9 1 cm and the bone was no longer palpable. It was remarkable progress: before initial maggot deployment, the wound volume was that of a gallon of milk. At the end of the third deployment, there was near-complete regranulation of the wound bed.
The maggots exceeded our expectations: they had eradicated this superbug from the necrotic deep tissue, allowing the wound to granulate and rapidly close. Antibiotics and dialysis were no longer needed, nor was additional surgical intervention or flap closure. At 3, 6-, and 12-month follow-up, the wound remained completely healed.
Case 2
A 46-year-old man with familial nonischemic cardiomyopathy and ventricular tachycardia was in cardiogenic shock complicated by Klebsiella pneumoniae ventilator-associated pneumonia at another facility in Puerto Rico, where he developed an unstageable sacral coccyx pressure injury during the acute illness. He was transferred via med flight from Puerto Rico to our institution for consideration of advanced heart therapies. Upon arrival, biventricular assist device placement was required for cardiac stabilization. Heart transplant work-up determined that the sacral wound was his only barrier to transplant listing, and the listing team did not report him for listing.
At this time, the sacral l coccyx wound measured 4.5 3 1 cm, with 3-cm circumferential undermining and copious, malodorous drainage (Figure 2). The wound base was completely necrotic, slough tissue with palpable, and exquisitely painful on palpation coccyx and sacral bone. The clinical diagnosis of sacral coccyx osteomyelitis was confirmed by magnetic resonance imaging. Culture biopsy of involved coccyx and sacral bone grew the same MDR Klebsiella pneumoniae (carbapenem-resistant Enterobacteriaceae) that had grown from the bronchoscopy culture 1 month previously in Puerto Rico. Surgical intervention in the operating room was contraindicated because he had previous life-threatening reactive arrhythmia (ventricular tachycardia) with general anesthesia.
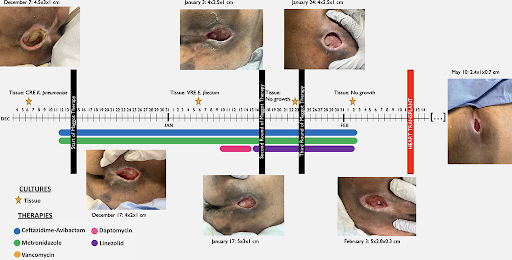
Figure 2. Timeline of evolution of sacral wound with treatment modalities used. Maggot therapy improved significantly in wound healing, avoiding the use of invasive surgical interventions. CRE = carbapenem resistant Enterobacterales; VRE = vancomycin resistant Enterococcus.
He was initiated on ceftazidime avibactam and metronidazole for management of osteomyelitis and had aggressive off-loading on the Envella sand bed support surface. Aggressive local wound care included quarter-strength Dakin’s loosely packed kerlix 3 times a day and with support for urinary or fecal incontinence. Maggot therapy was employed as an alternative to surgical intervention, given the aforementioned contraindications with any procedure requiring pain medication.
At the end of the therapy, he was noted to have significant improvement in the wound with minimal devitalized tissue remaining. The repeat deep tissue cultures demonstrated eradication of the MDR K pneumoniae.
As such, he was cleared for listing for heart transplantation, which he had successfully. At his 2-month outpatient wound center follow-up, he was nearly completely closed and no longer had any pain. He is now back in Puerto Rico with his family and has had no recurrence of his wound despite the level of immunosuppression and severity of his wound at presentation.
Case 3
A 74-year-old man with medical history relevant for ulcerative colitis and total abdominal colectomy with end ileostomy, diabetes mellitus, and chronic lymphocytic leukemia initially was admitted from rehabilitation due to nonhealing and progressive sacral decubitus ulcer, which probed to bone measuring 6 2 1 cm (Figure 3). He initially had surgical debridement down to the coccyx bone, establishing the diagnosis of cortical osteomyelitis. The cultures tested positive for polymicrobial infection with Streptococcus constellatus, Pseudomonas aeruginosa, Corynebacterium straitum, and E coli, for which he was started on intravenous vancomycin, cefepime, and metronidazole. Given the extent of the infection, he was considered to be a candidate for biodebridement with maggots and had his first session of maggot therapy while he finished the 6-week intravenous antibiotic course for osteomyelitis.
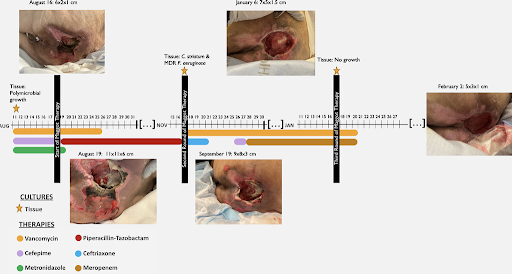
Figure 3. Timeline of evolution of sacral wound with treatment modalities used. Maggot therapy assisting in wound healing and granulation tissue formation in adjunctive to local wound care. MDR = multidrug-resistant.
The wound initially improved, and he continued to have additional minor debridement of the necrotic tissue in outpatient visits. However, he was readmitted 1 month later for deterioration of the wound. His repeat cultures demonstrated C straitum and a MDR P aeruginosa, for which he was started on intravenous vancomycin and meropenem.
Further surgical interventions were not considered as the debridements were only making the wound bigger (similar to the scenario in Case 1) and the medical and surgical services recommended hospice. The family requested wound care for a second opinion on salvage therapy options. He had 2 additional cycles of maggot therapy and was managed with aggressive offloading and wound care with negative-pressure wound therapy. The wound subsequently demonstrated clinical improvement with healthy granulation tissue, as depicted in Figure 3.
Discussion
Pressure injuries are a frequently encountered medical condition in health care settings. They usually occur over bony areas of the body where significant pressure distorts the tissues. According to several studies, the global prevalence of pressure ulcer is reported to be approximately 12.8% with hospital-related incidence of 8.4% (1). Case series and case reports describe the incidence of significant infectious complications such as osteomyelitis (14% 86%) in stage 4 or unstageable pressure injuries in the sacrum (2). The management of these wounds requires complex care with a multidisciplinary approach. Only limited data support the use of prolonged antibiotic therapy for such wounds, with the main goal of achieving closure in cases of sacral osteomyelitis (3). The duration and choice of antibiotics is also cumbersome for health care providers, with isolation of MDR organisms leading to use of expensive novel antimicrobials. Surgical interventions are also often necessary, with the goal of achieving source control. However, as our cases demonstrate, surgical intervention can often make the wounds larger and more difficult to close. Flap closure is rarely a readily available option in these complex patients due to their malnutrition, immobility, inability to offload, and other factors, such as immunosuppression. There is paucity of medical literature available in use of maggot biodebridement therapy for the treatment of such wounds. Here we present a few difficult-to-manage stage 4 sacral pressure injuries and osteomyelitis complicated with MDR organisms and successful treatment with maggot therapy.
Debridement of chronic wounds with maggot therapy was first introduced in the United States in the 1930s but with the introduction of effective antimicrobials, its utility waned until the 1990s, when there was renewed interest for its use as an adjunctive therapy for complex wounds. It uses green bot fly (Lucilia sericata) maggots, which are introduced into the wound and left for a few days (2 4 days) (4). Maggots can separate necrotic tissue from viable tissues, effectively perform wound debridement, and promote wound granulation with healthy tissue formation (5). Literature evidence supports favorable outcomes in the use of maggots in the debridement of such chronic wounds comparable with routine use of advanced wound care techniques and standard surgical interventions. Elimination of pathogenic organisms and faster reduction of wound surface area often with complete healing makes this biotherapy a promising alternative to available standard therapy options (6). A randomized control trial conducted in France showed a statistically significant reduction in slough by day 8 in patients who had maggot therapy as compared with those who had thrice-weekly surgical debridement, indicating that this process was faster at clearing necrotic tissue than conventional methods (7). Although this study did not show a significant difference between the 2 groups at 15 days, the authors did not evaluate longer-term outcomes.
Maggot therapy appears to be efficacious, cost-effective, and a well-tolerated method in wound care described in medical literature (8, 9). Since its approval by the Food and Drug Administration in 2004, it has been used in management of a wide spectrum of wounds, including necrotic ulcers, posttraumatic wound infections, necrotizing fasciitis, and diabetic foot ulcers (8). The use of maggot therapy for sacral decubitus ulcers with osteomyelitis has not been described widely (10). Limited case reports and case series suggest beneficial effects, especially in cases of failure to respond to classical wound care, antimicrobials, surgical debridement, and negative-pressure wound therapy (11, 12). Our cases support the use of maggots in successful eradication of deep-tissue infections (including MDR organisms), promoting healthy granulation tissue and preventing surgical interventions. It is worth mentioning that all our cases had limitations in surgical options due to the complexity of comorbid conditions. In all these cases, maggot biodebridement therapy was successfully used to accelerate the wound closure with the promotion of healthy granulation tissue. This also resulted in timely de-escalation and reduction in the need to continue broad-spectrum antimicrobials (13).
No significant side effects are noted with maggot therapy. The major symptom experienced by some patients is the sensation of tickling or itching. Mild-to-moderate pain may be experienced by a small fraction of patients, which can be managed with analgesics. None of these side effects were reported in our patients. Psychological and esthetic concerns are another aspect of maggot therapy that needs to be discussed with the patients before consideration (5).
Overall, maggot therapy seems to be a well-tolerated, cost-effective, and efficient in management of complicated sacral decubitus ulcers and osteomyelitis, especially where conventional methods were unsuccessful or unavailable.
These findings suggest that further clinical investigations and prospective comparative data are needed to elucidate the exact impact of maggot therapy for treatment of complicated sacral pressure injuries and osteomyelitis.
(21). Louise Smith, senior lecturer in clinical skills. Cultivating curiosity about our patients can make all the difference to their care. BMJ 2024; 384: q129
Asking questions that elicit who a patient is, and not just their diagnosis and symptoms, leads to more compassionate care, says Louise Smith
My mother lay there, day after day, waiting for the time to come. She had cancer and was terminally ill, with only a few days left to live. She was unconscious and cachexic, the toll of the disease evident. At 83 years old, she had grey hair as she could no longer visit the hairdresser. Before this illness, nothing would have got in the way of her weekly hair appointments that she had enjoyed for so many years.
The deterioration in her health had been rapid. Until quite recently, she had been an active woman who had enjoyed cooking, gardening, and looking after her two young grandchildren while their parents went to work. Now she was frail and bedbound.
When she was admitted to hospital for the final time, nurses attended to her needs, bringing her food and medication as required. They came and went, chatting to me as they went about their jobs. They all merged into one as my hurting brain took the situation in. Apart from one. Her words will stay with me forever. Did you mum work? she asked, followed by, What did she work as?
This nurse was interested in my mum as a person, not just as a patient. It meant the world to me.
She was not just an old, frail, bedbound, confused, terminally ill patient. She was a retired teacher who was a mum, wife, grandma, and who, until very recently, had lived a full and active life. She was not ready to die yet. Sadly, cancer had other ideas.
It reminded me of doing home visits when I was a GP. Seeing photos of patients with dementia in their younger days (on their wedding day or in a military uniform) was a stark reminder that they hadn’t always been the old and confused person I met. There had been many chapters of their lives before this. They had worked and travelled, married and started families, experienced both world events and life’s everyday joys. They deserved not just my respect, but a recognition of the full richness of their humanity.
I sometimes wonder how people will treat me as I become older. Will they take the time to ask me what I did or what my passions were?
When the Queen died, I thought how lucky she was that her healthcare staff and carers knew who she was and about the accomplishments she’d achieved throughout her life. Most people aren’t so lucky, but it doesn’t have to be that way.
Even short exchanges can help healthcare professionals to find out more about the people they care for so that they can provide more person-centred, compassionate care. And we can all spread the word and encourage our colleagues to do this.
As the lead for hospital visits for students in their first two years of medical school, I want students to find out who the patient lying in the hospital bed really is. We encourage students to not only find out the reason for a patient’s admission but also the effects of their illness on life at home, their family, and their day-to-day activities (including work and hobbies). This helps students to understand firsthand that, by finding out who the person is, they can be more compassionate doctors and care for the patient more fully as an individual. Asking questions such as what family do they have, do or did they work, and what are their favourite things to do are small, simple ways to gain an insight. I’m hoping that one day, if they treat me, my students will remember to find out about me and my life before I became ill.
Unfortunately, the major barrier to this practice continuing into my students’ future careers as doctors is time. A busy shift can be the enemy of curiosity. And, like most of the things that a doctor would like to do more of, the habit of asking questions can be crowded out by a high workload and the time pressures of clinical work. This is a shame as finding out more about patients can diminish doctors’ sense of working in an impersonal system where care has become transactional and increase their fulfilment at work. Healthcare systems should make space for these interactions for both parties’ benefit, and senior healthcare workers should model them. Even if someone just occasionally has the time to do this then, believe me, it makes all the difference.
(22). The Lancet, Published:January 20, 2024. What next in Parkinson’s disease?. DOI:https://doi.org/10.1016/S0140-6736(24)00094.
More than 200 years since the publication of James Parkinson’s An Essay on the Shaking Palsy (1817)’, many uncertainties regarding the progressive neurological disorder now known by his name remain.
This issue of The Lancet carries a Series dedicated to Parkinson’s disease, which includes an exploration of some of the outstanding questions around the epidemiology, causes, and current treatment options for this disabling and currently incurable condition.
Parkinson’s is second only to Alzheimer’s disease in the list of most common neurodegenerative disorders and, with increasing life expectancies and fewer competing causes of death, its prevalence is expected to increase to 12 17 million people by 2040.
Difficulties in the diagnosis of Parkinson’s (especially early disease) also hamper effective care
The pathogenesis of the disease remains largely elusive. The cause of Parkinson’s disease is multifactorial and, although there is consensus among experts that Parkinson’s is an age-related disease, questions regarding the extent to which Parkinson’s can be attributed to external drivers (such as pollutants) do not yet have clear answers.
Ultimately, research needs to aim for treatments that can alter the course of the disease but, despite growing research funding, major breakthroughs have been few and far between.
A move towards biologically based criteria for the classification of Parkinson’s is proving controversial, but the hope is that these new criteria can help detect the disease in its early stages, preferably in the prodromal phase, which might also pave the way for further research on disease-modifying therapies.
Meanwhile, clinical studies of new drugs to better treat dyskinesia and other motor symptoms are under way, as are trials covering several known mechanisms of disease in Parkinson’s. Non-pharmacological approaches such as robotics to help with gait impairments and music-based interventions to help manage various non-motor symptoms also show promise.
Additionally, the potential value of lifestyle interventions to improve control of Parkinson’s symptoms should not be overlooked, particularly regarding physical activity and nutrition, which offer some means to take care out of the clinic and into a patient’s home.
Despite an acute need for better access to specialist care, there is still much to be done in ensuring that essential drugs reach patients.
Informal carers, especially women, remain essential for many patients with Parkinson’s disease, yet their experiences are often overlooked, and there is little support for caregivers globally.
Tackling stigma against the disease (which can lead to higher rates of depression, comorbidities, and mortality in individuals with Parkinson’s) and dispelling the misconception that Parkinson’s disease is a natural consequence of ageing can be achieved through education and advocacy not least among health-care providers, especially to help to improve communication around a diagnosis of Parkinson’s.
A disease-modifying treatment to slow, halt, and reverse progression of Parkinson’s disease must be the goal to strive for. But in the meantime, improvements in basic and specialist care for patients with Parkinson’s disease supporting caregivers, ensuring access to simple medication regimens, and expanding the provision of primary and multidisciplinary care for comorbidities would make tremendous differences to the care and quality of life for millions of patients worldwide.
(23). Nicole Chicoine et al. Severe colonic distention and malnutrition in a 6-week-old infant: a case of Hirschsprung-associated enterocolitis. DOI:https://doi.org/10.1016/S0140-6736(23)02685-5
A 6-week-old infant was seen in our emergency department with his family, who reported him to be lethargic and unwell; his abdomen was distended and he had not passed faeces for 4 days.
The patient had been born at full term weighing 3.3 kg (typical range 2.5 4.0) after an uncomplicated pregnancy. He had passed faeces 48 h after birth with a glycerine suppository; from that point on he had passed daily, watery stools, developed repeated vomiting, and had failed to gain weight.
View related content for this article
On examination, the infant was emaciated weighing 3.5 kg (typical range at 6 weeks 2.3 4.9) with a significantly distended abdomen; he was febrile with a temperature of 38.5°C and tachycardic (heart rate 180 beats per min). The patient had no features of chromosomal abnormalities or suspicion of a neurodevelopmental disorder; he had no family history of gastrointestinal difficulties.
Laboratory investigations showed a leucocytosis of 28.0109 per L (typical range 6.0 17.5), and lactic acidosis with a venous lactate concentration of 3.3 mmol/L (typical range 0.5 2.2). An abdominal x-ray showed significant colonic distension; faeces were seen in the rectum but no air (figure).
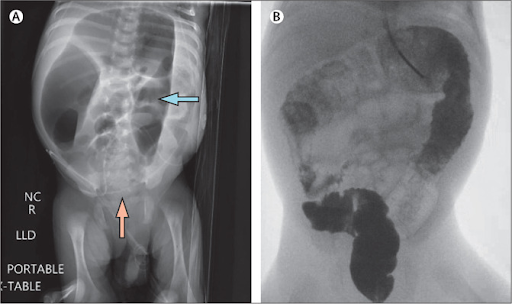
The patient was resuscitated in the neonatal intensive care unit and was given twice daily rectal irrigations with saline; he was also given intravenous antibiotics (ceftriaxone and metronidazole).
Further investigations included a suction rectal biopsy which found aganglionosis an absence of ganglion cells on three sections (section 1 at 1 cm, section 2 at 2 cm, and section 3 at 3 cm). Two transitions from dilated to narrowed colon were seen on contrast enema: one segment in the mid-sigmoid colon and the second in the descending colon (figure).
After a month of inpatient nutritional optimisation initially the patient had total parenteral nutrition, followed by a combination of oral and nasogastric lavage feeds with breastmilk and formula the patient had laparoscopic colonic biopsies taken and an end ileostomy. Histopathological examination of samples of the biopsies obtained during this operation confirmed Hirschsprung disease to the level of the distal splenic flexure. The patient was allowed home 7 weeks after the day of his initial admission.
At 11 months old, the patient had a planned laparotomy with Swenson pull-through of his distal transverse colon; this involved taking additional colonic biopsies to assess the location of the ganglion cells, resection of the aganglionic rectum, sigmoid, and descending colon, mobilisation of the splenic and hepatic flexures with takedown of the ligament for Treitz, and pull-through of the normal distal transverse colon to his anal canal with anastomosis 1 cm proximal to the dentate line.
At the age of 1 year and 1 month, the patient had an ileostomy reversal during a planned re-admission.
At his most recent follow-up, at 3 years of age, the patient had been doing well: he had been passing faeces regularly with no evidence of constipation; he was well-nourished and developing normally.
Hirschsprung-associated enterocolitis (HAEC) is a potentially life-threatening condition that occurs in Hirschsprung disease. HAEC is characterised by abdominal distention, fever, vomiting, and diarrhoea. Other associated symptoms include colicky abdominal pain, lethargy, and passing blood-stained stools. The condition is caused by a large stool burden in an aganglionic segment of bowel leading to bacterial overgrowth and infection. Initial management requires prompt recognition, antibiotics, and rectal irrigations. Delayed diagnosis of Hirschsprung disease can result in life-threatening enterocolitis and severe malnutrition.
(24). Zemplen Pataki et al. Paracoccidioidomycosis. N Engl J Med 2024; 390:357
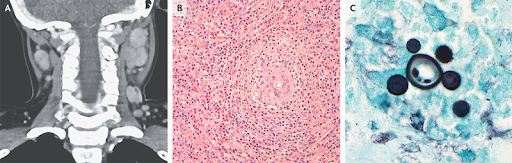
A 9-year-old boy who had recently emigrated from Brazil presented to the emergency department with a 3-week history of neck swelling, fevers, and weight loss. On physical examination, there was fixed, tender lymphadenopathy in the posterior auricular, submandibular, and occipital chains. There was no hepatosplenomegaly or rash. Laboratory testing was notable for an absolute eosinophil count of 12,878 per cubic millimeter (reference range, 0 to 400), anemia, thrombocytosis, hypoalbuminemia, and a negative fourth-generation assay for human immunodeficiency virus. Computed tomography of the neck showed hyperattenuating cervical lymphadenopathy on both sides (Panel A). An excisional biopsy of a lymph node in the deep left cervical region was performed, and histopathological examination of a biopsy specimen showed tissue eosinophilia, granulomatous formations, and conspicuous, round structures (Panel B, hematoxylin and eosin stain) and clusters of yeast forms (Panel C, Grocott Gomori methenamine silver stain). Tests for cryptococcus and histoplasmosis were negative, but a polymerase-chain-reaction assay of lymph node tissue was positive for Paracoccidioides brasiliensis. A diagnosis of paracoccidioidomycosis was made. Treatment with itraconazole was initiated but was later changed to fluconazole owing to adverse side effects. Two months after presentation, the patient’s symptoms had abated. Antifungal therapy was continued for 1 year.
(25). Tao Zhang et al. Hemolacria. N Engl J Med 2024; 390:e8

A 51-year-old man presented to the emergency department with a 1-hour history of bloody tears. Four hours before presentation, the patient had sustained blunt force trauma to the face in a fight. He had subsequently presented to the emergency department with nose pain and epistaxis and had received nasal packing. One hour after discharge from the emergency department, he returned with bloody tears, blurry vision, and eye pain. He had no history of ocular or nasal surgery.
On physical examination, blood oozed from the upper and lower lacrimal puncta of both eyes (arrow; the right eye is shown) and accumulated along the margins of the lower eyelids (see video) a finding known as hemolacria. The rest of the eye examination, including a slit-lamp examination, was normal. Ongoing epistaxis and ecchymosis of the nasal bridge were also noted.
tomography of the head and orbit showed no fractures. A diagnosis of hemolacria resulting from retrograde blood flow through the nasolacrimal system after nasal tamponade for epistaxis was made. To treat the ongoing epistaxis, the nose was repacked and topical epinephrine was applied to the left nasal cavity. A half hour later, the bloody tears had resolved.
(26). Matt Morgan. Do we still really need doctors?. BMJ. 2024;384:q155
Patients can now travel through health systems without ever meeting or needing a doctor. If their minor foot infection gets worse despite topical treatment from a pharmacist, they may see a primary care specialist nurse. After being referred to the hospital’s fast track assessment centre they’re seen by a physician assistant, before having an operation carried out by a surgical nurse practitioner helped by an anaesthetic assistant. Their postoperative sepsis is spotted by the critical care outreach team, and an advanced critical care practitioner inserts a central line to treat their septic shock. They survive their critical illness and are followed up in clinic by a consultant psychologist, consultant physiotherapist, and critical care follow-up nurse. All of which begs the question do we still really need doctors?
Acquiring specialist knowledge used to be expensive, guarded, and closely controlled. Budding doctors were invited into this hallowed fold if they were clever enough, rich enough, or connected enough. Today, a smartly edited 10 second clip on TikTok can teach millions of viewers the causes of clubbing. As medical knowledge has become openly accessible, doctors are defined more by their skills in specialist examinations or practical procedures. Today, however, the more experienced a doctor is, the less likely they are to compete with a first-year phlebotomist in taking blood from that tricky patient, owing to a gradual deskilling in practical procedures. So, what’s left? What are doctors for?
Overlapping needs
The taskification of medicine into discrete events, delivered through a multitude of roles, has not just flattened the hierarchy but jumped all over it. With this deconstruction comes protectionism regarding titles and role replacements, mostly motivated by patient safety concerns but with a little nepotism. Many safety concerns are valid, as medicine is much more than a series of discrete tasks.
Health can’t be found only from a blood test, diagnosis, or procedure. Although the art of medicine is an overused phrase, medicine certainly isn’t a factory line, simply producing new knees, improving levels of glycated haemoglobin, or cutting out cancers. There are times when a production line is an efficient and preferred model to learn from: you don’t want a deep dive into your childhood medical history when you need a splinter or cataract removed. But single, simple pathology is rare. The entire population is ageing, with more comorbidity, and our health needs are increasingly overlapping. It’s sometimes easier to say what a patient doesn’t have than what they do have.
So, yes we need roles with well grounded, deep knowledge of the boundaries of human health and science.
Specialists with other titles could assume these roles, but their training, education, experience, and tools would need to achieve an equivalent breadth and depth to a medical degree with postgraduate time.
And so, for now at least, people with this background are called doctors. Not only do we still need these roles but we need them more than ever. A return to the generalist has already started, recognising the modern maelstrom of health needs.
The acute physician, the trauma surgeon, and the intensivist are all essentially generalists in niche circumstances.
The role of the doctor has changed, of course, and long may that continue.
- We’re now conductors of an orchestra with an increasing array of old and new instruments, played by people from many different backgrounds.
- The conductor brings sounds to the front or fades them towards the back at the right times for the right music.
- They need to know the current arrangement in detail while also pulling experience from other orchestras, different music, and instruments they may have played in the past.
- can’t play every instrument in every orchestra, but they know how each one sounds and how loud it can go.
- They appreciate the skills, role, and dedication of each person making up that big orchestra sound.
- Importantly, a conductor knows when to start and stop.
- And when the song ends, whether on a major or a minor note, everyone knows that the music came from the whole orchestra. But without the person holding the baton, everything would be out of time.
(27). Erin E Wes et al. Complement in human disease: approved and up-and-coming therapeutics. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)01524-6/fulltext
Summary
The complement system is recognised as a protector against blood-borne pathogens and a controller of immune system and tissue homoeostasis. However, dysregulated complement activity is associated with unwanted or non-resolving immune responses and inflammation, which induce or exacerbate the pathogenesis of a broad range of inflammatory and autoimmune diseases. Although the merit of targeting complement clinically has long been acknowledged, the overall complement drug approval rate has been modest. However, the success of the humanised anti-C5 antibody eculizumab in effectively treating paroxysmal nocturnal haemoglobinuria and atypical haemolytic syndrome has revitalised efforts to target complement therapeutically. Increased understanding of complement biology has led to the identification of novel targets for drug development that, in combination with advances in drug discovery and development technologies, has resulted in a surge of interest in bringing new complement therapeutics into clinical use. The rising number of approved drugs still almost exclusively target rare diseases, but the substantial pipeline of up-and-coming treatment options will possibly provide opportunities to also expand the clinical targeting of complement to common diseases.
(28). Sir Roy Yorke Calne. The Lancet Obituary. 26 Jan 24. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)00099-0/fulltext
Highlights:
Professor of Surgery at the University of Cambridge, UK
A pioneer in transplantation surgery
Equally important was his role in identifying more effective means of immunosuppression.
Calne was always on the lookout for better immunosuppressants. Radiation was one of the earlier candidates
While working at London’s Royal Free Hospital, UK, he came across a paper about the immunomodulatory 6-mercaptopurine.
He tested it. It was effective, but quite toxic.
A better candidate, Calne later found, was its derivative azathioprine.
The drug that eventually allowed transplantation to become a routine procedure was cyclosporine.
Cyclosporine was developed by Jean-François Borel, an immunologist with the Sandoz company, as a potential anti-fungal agent.
The company was thinking of abandoning on account of its cost. Having shown cyclosporine’s efficacy in animal transplants, Calne began using it in human patients during the late 1970s. Its value was clear.
Prior to cyclosporine, 50% or 60% of kidney transplants from non-identical twins would last a year. after the introduction of cyclosporine in 1978 that figure increased towards 90 95%.
Cyclosporine was a game changer. It was a good immunosuppressant but didn’t put the patients at greater risk of infection.
Most noteworthy of Calne’s contributions to surgery was the development of liver transplantation for which he shared the 2012 Lasker DeBakey Clinical Medical Research Award with Thomas Starzl of Pittsburgh University, USA.
When Calne did his first liver transplant in 1968 it was the first not only in the UK but also in Europe.
Pioneering achievements by Calne included the world’s first heart, lung, and liver transplant in 1986 and the first successful stomach, intestine, pancreas, liver, and kidney transplant in 1994.
Calne as driven and competitive. He had persistence, determination, and a vision.
He had the foresight to dig in when all around him were suggesting it was a bad idea to do liver transplants because results were very poor He was undeterred.
Calne was very patient focused he wanted to solve their problems.
(29). The Lancet Infectious Diseases. A new dawn for malaria prevention. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(24)00012-4/fulltext
The heaviest burden of disease and death from Malaria is in WHO’s African Region where 95% of malaria cases occur and half a million children die from malaria each year. These data make malaria one of the continent’s biggest early childhood killers
Malaria prevention has been so far based mostly on the use of bednets, insect repellants, and antimalarial drugs. However, the absence of an effective malaria vaccine made malaria control difficult until recently.
The effort to develop a malaria vaccine started almost 60 years ago and has been hampered by the complexity of both the lifecycle of Plasmodium falciparum, the most common cause of malaria, and the immune response the parasite induces.
Thanks to the work of many researchers, the situation has changed. In 2021, there was the approval of the first malaria vaccine, RTS,S/AS01, developed and produced by GSK. As of April 2023, RTS,S/AS01 has been given to 1.5 million children living in areas with moderate-to-high malaria transmission and has shown the capacity to reduce malaria mortality by 30%. As the production capacity for RTS,S/AS01 is limited, it is not possible to meet the demand for a vaccine for all those in need.
Thus, the addition of a second vaccine, R21/Matrix-M, developed by the University of Oxford (Oxford, UK) and produced by the Serum Institute of India, to the WHO list of prequalified vaccines on Dec 21, 2023, is particularly welcome. R21/Matrix-M had already received a recommendation by WHO in October 2023.
(30). Walsh MR, Alam MS, Pierce KK, Carmolli M, Alam M, Dickson DM et al,. Safety and durable immunogenicity of the TV005 tetravalent dengue vaccine, across serotypes and age groups, in dengue-endemic Bangladesh: a randomised, controlled trial. Lancet Infect Dis. 2024 Feb;24(2):150-160.
Summary
Background
Morbidity and mortality from dengue virus (DENV) is rapidly growing in the large populations of south Asia. Few formal evaluations of candidate dengue vaccine candidates have been undertaken in India, Pakistan, or Bangladesh. Tetravalent vaccines must be tested for safety and immunogenicity in all age groups and in those previously exposed and naive to DENV infections. TV005 is a live, attenuated tetravalent dengue vaccine. We evaluated the safety and immunogenicity of a single dose of TV005 across age groups in dengue-endemic Bangladesh.
Methods
We performed a randomised, placebo-controlled age de-escalating clinical trial of TV005 at a single clinical site in dengue-endemic Dhaka, Bangladesh, following a technology transfer from the USA. Healthy (as determined by history, clinical examination, and safety laboratory test results) volunteers aged 1 50 years were randomly assigned 3:1 (stratified by four age groups) to receive a single dose of TV005 vaccine or placebo. Participants were followed up for 3 years. The study was double blind and was unmasked at day 180; outcome assessors, clinic staff, and volunteers remained blind throughout. Primary outcomes were safety, evaluated per-protocol as proportion of volunteers with solicited related adverse events of any severity through 28 days post dosing, and post-vaccination seropositivity by day 180 using serotype-specific neutralising antibodies (PRNT50 10). Secondary outcomes included viremia, impact of past dengue exposure, and durability of antibody responses. This study is registered with Clinicaltrials.gov, NCT02678455, and is complete.
Findings
Between March 13, 2016, and Feb 14, 2017, 192 volunteers were enrolled into four age groups (adults [18 50 years; 20 male and 28 female], adolescents [11 17 years; 27 male and 21 female], children [5 10 years; 15 male and 33 female], and young children [1 4 years; 29 male and 19 female]) with 48 participant per group. All participants were Bangladeshi. Vaccination was well tolerated and most adverse events were mild. Rash was the most common vaccine-associated solicited adverse event, in 37 (26%) of 144 vaccine recipients versus six (12%) of 48 placebo recipients; followed by fever in seven (5% of 144) and arthralgias in seven (6% of 108), which were only observed in vaccine recipients. Post-vaccine, volunteers of all ages (n=142) were seropositive to most serotypes with 118 (83%) seropositive to DENV 1, 141 (99%) to DENV 2, 137 (96%) to DENV 3, and 124 (87%) to DENV 4, overall by day 180. Post-vaccination, viraemia was not consistently found and antibody titres were higher (10 15-fold for DENV 1 3 and 1.6-fold for DENV 4) in individuals with past dengue exposure compared with the dengue-naive participants (DENV 1 mean 480 [SD 4.0] vs 32 [2.4], DENV 2 1042 [3.2] vs 105 [3.1], DENV 3 1406 [2.8] vs 129 [4.7], and DENV 4 105 [3.3] vs 65 [3.1], respectively). Antibody titres to all serotypes remained stable in most adults (63 86%) after 3 years of follow-up. However, as expected for individuals without past exposure to dengue, titres for DENV 1, 3, and 4 waned by 3 years in the youngest (1 4 year old) cohort (69% seropositive for DENV 2 and 22 28% seropositive for DENV 1, 3, and 4).
Interpretation
With 3 years of follow-up, the single-dose tetravalent dengue vaccine, TV005, was well tolerated and immunogenic for all four serotypes in young children to adults, including individuals with no previous dengue exposure.
Funding
National Institutes of Health National Institute of Allergy and Infectious Diseases Intramural Research Program and Johns Hopkins University.
The price of health
The Lancet Diabetes & Endocrinology, VOLUME 12, ISSUE 2, P83, FEBRUARY 2024.

