Journal scan: A review of 42 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Major Extremity Trauma Research Consortium (METRC), et al. Aspirin or Low-Molecular-Weight Heparin for Thromboprophylaxis after a Fracture. N Engl J Med. 2023;388:203-213.
Background
Clinical guidelines recommend low-molecular-weight heparin for thromboprophylaxis in patients with fractures, but trials of its effectiveness as compared with aspirin are lacking.
Methods
In this pragmatic, multicenter, randomized, noninferiority trial, we enrolled patients 18 years of age or older who had a fracture of an extremity (anywhere from hip to midfoot or shoulder to wrist) that had been treated operatively or who had any pelvic or acetabular fracture. Patients were randomly assigned to receive low-molecular-weight heparin (enoxaparin) at a dose of 30 mg twice daily or aspirin at a dose of 81 mg twice daily while they were in the hospital. After hospital discharge, the patients continued to receive thromboprophylaxis according to the clinical protocols of each hospital. The primary outcome was death from any cause at 90 days. Secondary outcomes were nonfatal pulmonary embolism, deep-vein thrombosis, and bleeding complications.
Results
A total of 12,211 patients were randomly assigned to receive aspirin (6101 patients) or low-molecular-weight heparin (6110 patients). Patients had a mean (±SD) age of 44.6±17.8 years, 0.7% had a history of venous thromboembolism, and 2.5% had a history of cancer. Patients received a mean of 8.8±10.6 in-hospital thromboprophylaxis doses and were prescribed a median 21-day supply of thromboprophylaxis at discharge. Death occurred in 47 patients (0.78%) in the aspirin group and in 45 patients (0.73%) in the low-molecular-weight-heparin group (difference, 0.05 percentage points; 96.2% confidence interval, -0.27 to 0.38; P<0.001 for a noninferiority margin of 0.75 percentage points). Deep-vein thrombosis occurred in 2.51% of patients in the aspirin group and 1.71% in the low-molecular-weight-heparin group (difference, 0.80 percentage points; 95% CI, 0.28 to 1.31). The incidence of pulmonary embolism (1.49% in each group), bleeding complications, and other serious adverse events were similar in the two groups.
Conclusions
In patients with extremity fractures that had been treated operatively or with any pelvic or acetabular fracture, thromboprophylaxis with aspirin was noninferior to low-molecular-weight heparin in preventing death and was associated with low incidences of deep-vein thrombosis and pulmonary embolism and low 90-day mortality. (Funded by the Patient-Centered Outcomes Research Institute; PREVENT CLOT ClinicalTrials
(2). Le Ma, et al. Beverage consumption and mortality among adults with type 2 diabetes: prospective cohort study. BMJ 2023;381:e073406.
Objective:
To investigate the intake of specific types of beverages in relation to mortality and cardiovascular disease (CVD) outcomes among adults with type 2 diabetes.
Design:
Prospective cohort study.
Setting:
Health professionals in the United States.
Participants:
15486 men and women with a diagnosis of type 2 diabetes at baseline and during follow-up (Nurses’ Health Study: 1980-2018; and Health Professionals Follow-Up Study: 1986-2018). Beverage consumption was assessed using a validated food frequency questionnaire and updated every two to four years.
Main outcome measures:
The main outcome was all cause mortality. Secondary outcomes were CVD incidence and mortality.
Results:
During an average of 18.5 years of follow-up, 3447 (22.3%) participants with incident CVD and 7638 (49.3%) deaths were documented. After multivariable adjustment, when comparing the categories of lowest intake of beverages with the highest intake, the pooled hazard ratios for all cause mortality were 1.20 (95% confidence interval 1.04 to 1.37) for sugar sweetened beverages (SSBs), 0.96 (0.86 to 1.07) for artificially sweetened beverages (ASBs), 0.98 (0.90 to 1.06) for fruit juice, 0.74 (0.63 to 0.86) for coffee, 0.79 (0.71 to 0.89) for tea, 0.77 (0.70 to 0.85) for plain water, 0.88 (0.80 to 0.96) for low fat milk, and 1.20 (0.99 to 1.44) for full fat milk. Similar associations were observed between the individual beverages and CVD incidence and mortality. In particular, SSB intake was associated with a higher risk of incident CVD (hazard ratio 1.25, 95% confidence interval 1.03 to 1.51) and CVD mortality (1.29, 1.02 to 1.63), whereas significant inverse associations were observed between intake of coffee and low fat milk and CVD incidence. Additionally, compared with those who did not change their consumption of coffee in the period after a diabetes diagnosis, a lower all cause mortality was observed in those who increased their consumption of coffee. A similar pattern of association with all cause mortality was also observed for tea, and low fat milk. Replacing SSBs with ABSs was significantly associated with lower all cause mortality and CVD mortality, and replacing SSBs, ASBs, fruit juice, or full fat milk with coffee, tea, or plain water was consistently associated with lower all cause mortality.
Conclusions:
Individual beverages showed divergent associations with all cause mortality and CVD outcomes among adults with type 2 diabetes. Higher intake of SSBs was associated with higher all cause mortality and CVD incidence and mortality, whereas intakes of coffee, tea, plain water, and low fat milk were inversely associated with all cause mortality. These findings emphasize the potential role of healthy choices of beverages in managing the risk of CVD and premature death overall in adults with type 2 diabetes.
(3). David A Warrell et al. Clinical aspects of snakebite envenoming and its treatment in low-resource settings. Lancet 2023;401(10385):P1382-1398.
Summary
There is increasing recognition of the public health importance of snakebite envenoming. Worldwide annual incidence is likely to be 5 million bites, with mortality exceeding 150000 deaths, and the resulting physical and psychological morbidity leads to substantial social and economic repercussions. Prevention through community education by trained health workers is the most effective and economically viable strategy for reducing risk of bites and envenoming. Clinical challenges to effective treatment are most substantial in rural areas of low-resource settings, where snakebites are most common. Classic skills of history taking, physical examination, and use of affordable point-of-care tests should be followed by monitoring of evolving local and systemic envenoming. Despite the profusion of new ideas for interventions, hyperimmune equine or ovine plasma-derived antivenoms remain the only specific treatment for snakebite envenoming. The enormous interspecies and intraspecies complexity and diversity of snake venoms, revealed by modern venomics, demands a radical redesign of many current antivenoms.
(4). Ornella Verrastro, et al. Bariatric-metabolic surgery versus lifestyle intervention plus best medical care in non-alcoholic steatohepatitis (BRAVES): a multicentre, open-label, randomised trial. Lancet. 2023;S0140.
Background
Observational studies suggest that bariatric-metabolic surgery might greatly improve non-alcoholic steatohepatitis (NASH). However, the efficacy of surgery on NASH has not yet been compared with the effects of lifestyle interventions and medical therapy in a randomised trial.
Methods
We did a multicentre, open-label, randomised trial at three major hospitals in Rome, Italy. We included participants aged 25-70 years with obesity (BMI 30-55 kg/m2), with or without type 2 diabetes, with histologically confirmed NASH. We randomly assigned (1:1:1) participants to lifestyle modification plus best medical care, Roux-en-Y gastric bypass, or sleeve gastrectomy. The primary endpoint of the study was histological resolution of NASH without worsening of fibrosis at 1-year follow-up. This study is registered at ClinicalTrials.gov, NCT03524365.
Findings
Between April 15, 2019, and June 21, 2021, we biopsy screened 431 participants; of these, 103 (24%) did not have histological NASH and 40 (9%) declined to participate. We randomly assigned 288 (67%) participants with biopsy-proven NASH to lifestyle modification plus best medical care (n=96 [33%]), Roux-en-Y gastric bypass (n=96 [33%]), or sleeve gastrectomy (n=96 [33%]). In the intention-to-treat analysis, the percentage of participants who met the primary endpoint was significantly higher in the Roux-en-Y gastric bypass group (54 [56%]) and sleeve gastrectomy group (55 [57%]) compared with lifestyle modification (15 [16%]; p<0.0001). The calculated probability of NASH resolution was 3.60 times greater (95% CI 2.19-5.92; p<0.0001) in the Roux-en-Y gastric bypass group and 3.67 times greater (2.23-6.02; p<0.0001) in the sleeve gastrectomy group compared with in the lifestyle modification group. In the per protocol analysis (236 [82%] participants who completed the trial), the primary endpoint was met in 54 (70%) of 77 participants in the Roux-en-Y gastric bypass group and 55 (70%) of 79 participants in the sleeve gastrectomy group, compared with 15 (19%) of 80 in the lifestyle modification group (p<0.0001). No deaths or life-threatening complications were reported in this study. Severe adverse events occurred in ten (6%) participants who had bariatric-metabolic surgery, but these participants did not require re-operations and severe adverse events were resolved with medical or endoscopic management.
Interpretation
Bariatric-metabolic surgery is more effective than lifestyle interventions and optimised medical therapy in the treatment of NASH.
(5). Joanna M Wardlaw et al. Even more benefit with endovascular treatment for patients with acute ischaemic stroke: MR CLEAN-LATE. Lancet. 2023;401(10385):1317-1319.
Since 2015 endovascular treatment has been an established treatment for intracranial large artery occlusion up to 6 h after symptom onset or when the patient was last known well. The effect of endovascular treatment within 6 h is strong; however, the timepoint when recanalisation therapy becomes ineffective varies between individuals, and some patients might benefit after 6 h. The DEFUSE-3 and DAWN trials tested endovascular treatment up to 16 h or 24 h after symptom onset in patients selected using clinical criteria and perfusion imaging (to identify ischaemic core and tissue-at-risk volumes within strict limits), and showed benefit within these strict criteria. On this basis, endovascular treatment was extended for clinical use beyond 6 h after stroke for patients meeting the DEFUSE-3 and DAWN clinical and perfusion imaging criteria. However, the large treatment benefit in these late-treatment-window trials, despite strict selection criteria, suggested that more patients might benefit from endovascular treatment in the late window. Because perfusion imaging is not universally available and definitions of infarct core and tissue-at-risk are inconsistent and not easy to use in emergency settings, identification of more pragmatic easy-to-interpret widely available imaging selection methods could make endovascular treatment accessible to many more late-presenting patients worldwide.
Background
Endovascular treatment for anterior circulation ischaemic stroke is effective and safe within a 6 h window. MR CLEAN-LATE aimed to assess efficacy and safety of endovascular treatment for patients treated in the late window (6-24 h from symptom onset or last seen well) selected on the basis of the presence of collateral flow on CT angiography (CTA).
Methods
MR CLEAN-LATE was a multicentre, open-label, blinded-endpoint, randomised, controlled, phase 3 trial done in 18 stroke intervention centres in the Netherlands. Patients aged 18 years or older with ischaemic stroke, presenting in the late window with an anterior circulation large-vessel occlusion and collateral flow on CTA, and a neurological deficit score of at least 2 on the National Institutes of Health Stroke Scale were included. Patients who were eligible for late-window endovascular treatment were treated according to national guidelines (based on clinical and perfusion imaging criteria derived from the DAWN and DEFUSE-3 trials) and excluded from MR CLEAN-LATE enrolment. Patients were randomly assigned (1:1) to receive endovascular treatment or no endovascular treatment (control), in addition to best medical treatment. Randomisation was web based, with block sizes ranging from eight to 20, and stratified by centre. The primary outcome was the modified Rankin Scale (mRS) score at 90 days after randomisation. Safety outcomes included all-cause mortality at 90 days after randomisation and symptomatic intracranial haemorrhage. All randomly assigned patients who provided deferred consent or died before consent could be obtained comprised the modified intention-to-treat population, in which the primary and safety outcomes were assessed. Analyses were adjusted for predefined confounders. Treatment effect was estimated with ordinal logistic regression and reported as an adjusted common odds ratio (OR) with a 95% CI. This trial was registered with the ISRCTN, ISRCTN19922220.
Findings
Between Feb 2, 2018, and Jan 27, 2022, 535 patients were randomly assigned, and 502 (94%) patients provided deferred consent or died before consent was obtained (255 in the endovascular treatment group and 247 in the control group; 261 [52%] females). The median mRS score at 90 days was lower in the endovascular treatment group than in the control group (3 [IQR 2-5] vs 4 [2-6]), and we observed a shift towards better outcomes on the mRS for the endovascular treatment group (adjusted common OR 1.67 [95% CI 1.20-2.32]). All-cause mortality did not differ significantly between groups (62 [24%] of 255 patients vs 74 [30%] of 247 patients; adjusted OR 0.72 [95% CI 0.44-1.18]). Symptomatic intracranial haemorrhage occurred more often in the endovascular treatment group than in the control group (17 [7%] vs four [2%]; adjusted OR 4.59 [95% CI 1.49-14.10]).
Interpretation
In this study, endovascular treatment was efficacious and safe for patients with ischaemic stroke caused by an anterior circulation large-vessel occlusion who presented 6-24 h from onset or last seen well, and who were selected on the basis of the presence of collateral flow on CTA. Selection of patients for endovascular treatment in the late window could be primarily based on the presence of collateral flow.
(6). Freddie C. Hamdy, et al. Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N Engl J Med. 2023;388:1547-1558.
Background
Between 1999 and 2009 in the United Kingdom, 82,429 men between 50 and 69 years of age received a prostate-specific antigen (PSA) test. Localized prostate cancer was diagnosed in 2664 men. Of these men, 1643 were enrolled in a trial to evaluate the effectiveness of treatments, with 545 randomly assigned to receive active monitoring, 553 to undergo prostatectomy, and 545 to undergo radiotherapy.
Methods
At a median follow-up of 15 years (range, 11 to 21), we compared the results in this population with respect to death from prostate cancer (the primary outcome) and death from any cause, metastases, disease progression, and initiation of long-term androgen-deprivation therapy (secondary outcomes).
Results
Follow-up was complete for 1610 patients (98%). A risk-stratification analysis showed that more than one third of the men had intermediate or high-risk disease at diagnosis. Death from prostate cancer occurred in 45 men (2.7%): 17 (3.1%) in the active-monitoring group, 12 (2.2%) in the prostatectomy group, and 16 (2.9%) in the radiotherapy group (P=0.53 for the overall comparison). Death from any cause occurred in 356 men (21.7%), with similar numbers in all three groups. Metastases developed in 51 men (9.4%) in the active-monitoring group, in 26 (4.7%) in the prostatectomy group, and in 27 (5.0%) in the radiotherapy group. Long-term androgen-deprivation therapy was initiated in 69 men (12.7%), 40 (7.2%), and 42 (7.7%), respectively; clinical progression occurred in 141 men (25.9%), 58 (10.5%), and 60 (11.0%), respectively. In the active-monitoring group, 133 men (24.4%) were alive without any prostate cancer treatment at the end of follow-up. No differential effects on cancer-specific mortality were noted in relation to the baseline PSA level, tumor stage or grade, or risk-stratification score. No treatment complications were reported after the 10-year analysis.
Conclusions
After 15 years of follow-up, prostate cancer-specific mortality was low regardless of the treatment assigned. Thus, the choice of therapy involves weighing trade-offs between benefits and harms associated with treatments for localized prostate cancer. (Funded by the National Institute for Health and Care Research;
(7). Inge M. van der Sluis, et al Blinatumomab Added to Chemotherapy in Infant Lymphoblastic Leukemia. N Engl J Med. 2023;388:1572-1581.
Background
KMT2A-rearranged acute lymphoblastic leukaemia (ALL) in infants is an aggressive disease with 3-year event-free survival below 40%. Most relapses occur during treatment, with two thirds occurring within 1 year and 90% within 2 years after diagnosis. Outcomes have not improved in recent decades despite intensification of chemotherapy.
Methods
We studied the safety and efficacy of blinatumomab, a bispecific T-cell engager molecule targeting CD19, in infants with KMT2A-rearranged ALL. Thirty patients younger than 1 year of age with newly diagnosed KMT2A-rearranged ALL were given the chemotherapy used in the Interfant-06 trial with the addition of one postinduction course of blinatumomab (15 μg per square meter of body-surface area per day; 28-day continuous infusion). The primary end point was clinically relevant toxic effects, defined as any toxic effect that was possibly or definitely attributable to blinatumomab and resulted in permanent discontinuation of blinatumomab or death. Minimal residual disease (MRD) was measured by polymerase chain reaction. Data on adverse events were collected. Outcome data were compared with historical control data from the Interfant-06 trial.
Results
The median follow-up was 26.3 months (range, 3.9 to 48.2). All 30 patients received the full course of blinatumomab. No toxic effects meeting the definition of the primary end point occurred. Ten serious adverse events were reported (fever [4 events], infection [4], hypertension [1], and vomiting [1]). The toxic-effects profile was consistent with that reported in older patients. A total of 28 patients (93%) either were MRD-negative (16 patients) or had low levels of MRD (<5×10-4 [i.e., <5 leukemic cells per 10,000 normal cells], 12 patients) after the blinatumomab infusion. All the patients who continued chemotherapy became MRD-negative during further treatment. Two-year disease-free survival was 81.6% in our study (95% confidence interval [CI], 60.8 to 92.0), as compared with 49.4% (95% CI, 42.5 to 56.0) in the Interfant-06 trial; the corresponding values for overall survival were 93.3% (95% CI, 75.9 to 98.3) and 65.8% (95% CI, 58.9 to 71.8).
Conclusions
Blinatumomab added to Interfant-06 chemotherapy appeared to be safe and had a high level of efficacy in infants with newly diagnosed KMT2A-rearranged ALL as compared with historical controls from the Interfant-06 trial. (Funded by the Princess Máxima Center Foundation and others
(8). Peter J. Hutchinson, et al. Decompressive Craniectomy versus Craniotomy for Acute Subdural Hematoma. 2023
Background
Traumatic acute subdural hematomas frequently warrant surgical evacuation by means of a craniotomy (bone flap replaced) or decompressive craniectomy (bone flap not replaced). Craniectomy may prevent intracranial hypertension, but whether it is associated with better outcomes is unclear.
Methods
We conducted a trial in which patients undergoing surgery for traumatic acute subdural hematoma were randomly assigned to undergo craniotomy or decompressive craniectomy. An inclusion criterion was a bone flap with an anteroposterior diameter of 11 cm or more. The primary outcome was the rating on the Extended Glasgow Outcome Scale (GOSE) (an 8-point scale, ranging from death to “upper good recovery” [no injury-related problems]) at 12 months. Secondary outcomes included the GOSE rating at 6 months and quality of life as assessed by the EuroQol Group 5-Dimension 5-Level questionnaire (EQ-5D-5L).
Results
A total of 228 patients were assigned to the craniotomy group and 222 to the decompressive craniectomy group. The median diameter of the bone flap was 13 cm (interquartile range, 12 to 14) in both groups. The common odds ratio for the differences across GOSE ratings at 12 months was 0.85 (95% confidence interval, 0.60 to 1.18; P=0.32). Results were similar at 6 months. At 12 months, death had occurred in 30.2% of the patients in the craniotomy group and in 32.2% of those in the craniectomy group; a vegetative state occurred in 2.3% and 2.8%, respectively, and a lower or upper good recovery occurred in 25.6% and 19.9%. EQ-5D-5L scores were similar in the two groups at 12 months. Additional cranial surgery within 2 weeks after randomization was performed in 14.6% of the craniotomy group and in 6.9% of the craniectomy group. Wound complications occurred in 3.9% of the craniotomy group and in 12.2% of the craniectomy group.
Conclusions
Among patients with traumatic acute subdural hematoma who underwent craniotomy or decompressive craniectomy, disability and quality-of-life outcomes were similar with the two approaches. Additional surgery was performed in a higher proportion of the craniotomy group, but more wound complications occurred in the craniectomy group. (Funded by the National Institute for Health and Care Research)
(9). Ting-Han Tai, et al. Isolated Ulnar Shaft Fracture. N Engl J Med. 2023;388:e59.

A 60-year-old left-handed woman presented to the emergency department with pain in her left forearm after having been struck by a baseball bat by her partner. On physical examination, the left forearm was swollen and tender, especially with passive pronation and supination. The overlying skin was intact, and the results of neurovascular examination were normal. No other traumatic injuries were present. Radiographs of the left forearm showed an isolated ulnar shaft fracture (upper image, anteroposterior view; lower image, lateral view). Isolated ulnar shaft fractures, also called “nightstick fractures,” result from blunt force trauma to the forearm. The injury classically occurs when the upper arm is raised in self-defense against an attack to the head or torso, such as in intimate-partner violence, as occurred in this case. Comprehensive assessments of the safety and mental health of the patient were performed, and social services were offered. The patient underwent open reduction and internal fixation of the fracture, followed by splinting, although this type of injury may be managed nonoperatively in some cases. At follow-up 10 weeks later, the patient had regained full function of her arm; she had obtained a restraining order for protection and was receiving assistance from a social worker.
(10). Ayisha A Ashmore, et al. Recognition and initial management of ovarian torsion. BMJ 2023;381:e074514.
What you need to know
Ovarian torsion is a gynaecological emergency: a delay in diagnosis and referral can lead to a reduction in fertility. Ovarian masses are the most common cause of ovarian torsion, but torsion can occur in their absence, including in pregnancy and postpartum. Ovarian torsion can present without severe pain but instead with more vague symptoms such as isolated nausea and vomiting. The presence of ovarian blood flow on Doppler sonography cannot exclude ovarian torsion and so should not be used to dismiss the diagnosis of torsion in the presence of a suggestive history and clinical examination: seek a senior gynaecological opinion to determine the need for a diagnostic laparoscopy
What is ovarian torsion?
Ovarian torsion is a gynaecological emergency characterised by the ovary twisting or torting on the ligaments that suspend it within the pelvis. While the exact incidence is unknown, it accounts for 2-3% of all acute gynaecological emergencies. In torsion, the ovary typically twists around the infundibulo-pelvic ligament, also known as the suspensory ligament of the ovary, leading to compression of the ovarian vessels. If this compression continues, the ovary becomes oedematous and ischaemic. If left untreated over several hours, the ovary can become necrotic and haemorrhagic, leading to long term reduction in fertility. There is limited evidence for the diagnosis and management of ovarian torsion, meaning uncertainties in the management of affected patients.
(11). Chang Liu et al. Surgical versus non-surgical treatment for sciatica: systematic review and meta-analysis of randomised controlled trials. BMJ 2023;381:e070730.
Objective
To investigate the effectiveness and safety of surgery compared with non-surgical treatment for sciatica.
Design
Systematic review and meta-analysis.
Data sources
Medline, Embase, CINAHL, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, and the World Health Organisation International Clinical Trials Registry Platform from database inception to June 2022.
Eligibility criteria for selecting studies
Randomised controlled trials comparing any surgical treatment with non-surgical treatment, epidural steroid injections, or placebo or sham surgery, in people with sciatica of any duration due to lumbar disc herniation (diagnosed by radiological imaging).
Data extraction and synthesis
Two independent reviewers extracted data. Leg pain and disability were the primary outcomes. Adverse events, back pain, quality of life, and satisfaction with treatment were the secondary outcomes. Pain and disability scores were converted to a scale of 0 (no pain or disability) to 100 (worst pain or disability). Data were pooled using a random effects model. Risk of bias was assessed with the Cochrane Collaboration’s tool and certainty of evidence with the grading of recommendations assessment, development, and evaluation (GRADE) framework. Follow-up times were into immediate term (≤six weeks), short term (>six weeks and ≤three months), medium term (>three and <12 months), and long term (at 12 months).
Results
24 trials were included, half of these investigated the effectiveness of discectomy compared with non-surgical treatment or epidural steroid injections (1711 participants). Very low to low certainty evidence showed that discectomy, compared with non-surgical treatment, reduced leg pain: the effect size was moderate at immediate term (mean difference -12.1 (95% confidence interval -23.6 to -0.5)) and short term (-11.7 (-18.6 to -4.7)), and small at medium term (-6.5 (-11.0 to -2.1)). Negligible effects were noted at long term (-2.3 (-4.5 to -0.2)). For disability, small, negligible, or no effects were found. A similar effect on leg pain was found when comparing discectomy with epidural steroid injections. For disability, a moderate effect was found at short term, but no effect was observed at medium and long term. The risk of any adverse events was similar between discectomy and non-surgical treatment (risk ratio 1.34 (95% confidence interval 0.91 to 1.98)).
Conclusion
Very low to low certainty evidence suggests that discectomy was superior to non-surgical treatment or epidural steroid injections in reducing leg pain and disability in people with sciatica with a surgical indication, but the benefits declined over time. Discectomy might be an option for people with sciatica who feel that the rapid relief offered by discectomy outweighs the risks and costs associated with surgery.
(12). Mary Shaniqua. What Your Patient is Thinking. BMJ 2023;381:p475
Mary shares her experience of living with sickle cell disease and the importance of empathy
I received a diagnosis of sickle cell disease when I was around 18 months old. I have since experienced very challenging symptoms and diagnoses, including avascular necrosis, iron overload, and pulmonary embolism. Changes in my body caused by sickle cell have also significantly affected my mobility and my social life.
Experiencing a crisis is awful. The pain is excruciating. It feels like someone armed with knives in their hands and spikes on their feet jumping, stabbing, and stamping to their own rhythm inside a selected part of my body. The knives feel like they are deep within the epicentre of my bones and stabbing outwards, at every angle, in an attempt to escape; creating a piercing radiating pain. When I present to you in crisis, I am in agony. But you can help me through these difficult, traumatic-yet recurring-vulnerable periods in my life.
Empathy is crucial
When I am experiencing a sickle cell crisis, empathy is crucial. Empathy means recognising that I am suffering, listening to me, and engaging me in decisions about my treatment. It can be as simple as reassuring me that resolving my pain is your priority, even if it means we must take some steps back to move forward. I remember an admission to hospital when my pain was so excruciating I was frozen to the bed in a seemingly awkward position. I was trying, but failing, to distract myself with a book. The doctor doing the ward round came in and saw my position, and immediately recognised I was in a lot of pain and that we needed to change strategy.
He shifted the conversation briefly to the book, which helped calm me a bit. He then asked me about myself, what I do, and what I was looking forward to on discharge. We found common ground and spoke about our shared interests. This helped me understand that he truly saw me as a person, and cared about making me better. He suggested going back to a higher dosage of pain relief, which was an apparent step back, but it worked in making me more comfortable.
So much more than my disease
Sickle cell has a huge impact on my life, but I am so much more than a sickle cell patient. There are many components to me that are often lost when I enter a hospital.
My life away from the hospital is beautiful, and I desperately want to get back to that life. Days spent in hospital have wider impacts on my family, career, and social life, and can have adverse consequences for me financially. This is why resolving the sickle cell crisis, as quickly as possible, is my top priority. My plea to doctors is to show empathy, release any negative preconceptions about how people manage pain, and prioritise resolving the pain so that I can get home as soon as it is safe to do so.
What you need to know
Patients bring their own knowledge, instincts, and experience. Hearing these can help you work together
Finding shared interests or common ground can help patients relax and cultivate a more trusting relationship
Patients have whole lives outside their health. Ask them about this to gain greater insight into their plight
Education into practice
What could you do to help someone navigate the pain they are experiencing?
How can you ensure you are taking a patient’s experience into consideration when managing pain?
When might you consider asking a patient about their life beyond their health condition
(13). Hirofumi Hirakawa, et al. A strange smell and visions in a 45-year-old man with focal epilepsy. Lancet 2023;401(10386):P1458.
A 45-year-old man with a 5-year history of episodes of smelling a strange odour followed by seeing images of scenes from his childhood, attended our psychiatry department. The patient said that after experiencing the smell and the images, he felt shivery, had piloerection, and was short of breath; each episode lasted about 1 min, with no impairment of consciousness or abnormal movements. The problem tended to occur when he was tired, or sleep deprived. Previously, the episodes occurred once every 3 months, but recently-as his work had become more demanding-they happened more frequently; in the previous month, prior to presenting, they had occurred weekly. The patient reported no accompanying headache and had no history of medical or psychiatric illness.
On examination he was generally fit and well; a neurological examination showed no abnormalities; he was left-handed.
Laboratory investigations-including a complete blood count, liver and kidney function tests, serum electrolytes, and thyroid function tests-were within normal limits.
MRI of the patient’s brain showed a hypointense lesion in the right posterior parahippocampal gyrus on T2 star-weighted imaging, fluid-attenuated inversion recovery, diffusion-weighted imaging, and apparent diffusion coefficient (figure). Hippocampal signal abnormalities were not detected on T1-weighted and T2-weighted imaging. Magnetic resonance angiography showed no abnormalities
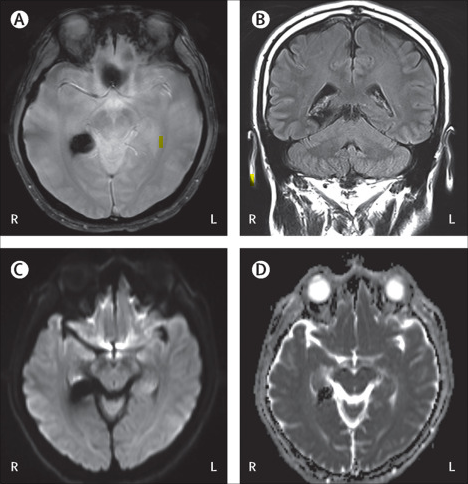
The MRI finding indicated an old intracerebral haemorrhage-insufficient to explain the patient’s primary complaints. An electroencephalogram (EEG) showed generalised 5 Hz spike and sharp wave complexes with an electrographic maximum in the right anterior temporal scalp electrodes, predominantly in the right hemisphere (appendix). Considering the findings in the round, we made a diagnosis of temporal lobe epilepsy (TLE) with focal seizures secondary to the old intracerebral haemorrhage in the right posterior parahippocampal gyrus. Two weeks after starting carbamazepine, the patient’s symptoms had fully resolved.
The differential diagnosis of hallucinations in any modality is extensive. Epilepsy is polymorphic and may mimic a multitude of disorders. An abnormal EEG is most helpful to determine the likely epilepsy type-focal or generalised. TLE is the most common form of localisation-related epilepsy, most frequently appearing in adolescence; hippocampal sclerosis is the most common cause-although it may be caused by structural lesions such as intracerebral haemorrhage or stroke occurring after middle age. Symptoms of focal temporal seizures are characterised by déjí vu, hallucinations, emotional symptoms, epigastric sensations, autonomic features, impairment of awareness or consciousness, and motor manifestations. Olfactory hallucinations are caused by lesions in medial temporal lobe structures-including the anterior parahippocampal gyrus; visual hallucinations occur with right temporal lobe seizures. The right anterior hippocampus relates to topographical hallucinations and the right parahippocampal place area relates to topographical hallucinations along with déjí vu. The semiology of epileptic seizures-as in our case-indicates activation, or dysfunction, of the areas of brain affected.
(14). Flora Peyvandi, et al. Fitusiran in haemophilia: a breakthrough drug with many unknowns. Lancet 2023;401(10386):P1400-1401.
Haemophilia A, defined by factor VIII (FVIII) deficiency, and haemophilia B, defined by factor IX (FIX) deficiency, are X chromosome linked diseases characterised by reduced thrombin generation and bleeding symptoms. 1Prophylaxis with replacement FVIII and FIX is considered the gold standard in haemophilia treatment. Over the past two decades, the treatment landscape in haemophilia has changed substantially with the introduction of extended half-life products, FVIII-activity mimicking agents, and innovative drugs, which aim to rebalance the anticoagulant potential through the inhibition of natural anticoagulants. One of the rebalancing drugs, fitusiran, an investigational small interfering RNA agent, reduces antithrombin synthesis in the hepatocytes, ultimately rebalancing haemostasis.
(15). Colin McCord. A rare brand of a Heart Surgeon. Lancet 2023;401(10386):P1420.
He lived to 94 and died of of congestive heart failure
Did some of the first surgical replacements of diseased heart valves with prosthetic valves. Worked in heart valve replacement with Albert StarrWorked across Asia and Africa to improve public health by implementing interventions such as oral rehydration therapy “A very successful cardiac surgeon who became politicised and decided doing coronary artery bypass grafting was not really the way to improve population health,” In Africa ( Mozambique) he started “developing this new cadre, which they called surgical technicians, who were people trained to do caesarean sections, hernia repairs”. “That meant that in rural settings…women wouldn’t die in childbirth just because they don’t have access to operative deliveries.” He helped to usher in a ban on smoking in most public places and the elimination of trans fats from NYC food services and also to establish an office in the Bronx, where “he worked hard on the idea of reducing teen pregnancy, which worked”. “He just had this clarity about what can be done to make the biggest difference”
(16). Hugo Rodriguez Zanella. Double-orifice mitral valve (DOMV). 2023.
Double-orifice mitral valve (DOMV) is a rare congenital cardiac defect (1% of all types of congenital heart disease). Three varieties have been described: complete bridge, incomplete bridge, and an eccentric type. Patients with DOMV, mitral regurgitation can be found in up to 43% and stenosis in 13%. However, patients rarely need surgical treatment in the absence of associated defects.
A bicuspid aortic valve can coexist as it is the most common congenital valvular heart disease associated with coarctation of the aorta.
Differential diagnoses from imaging modalities include transcathether edge-to-edge mitral valve repair and surgical Alfieri stitch. Both are associated with a similar opening of the mitral valve.
Three years after presentation, the patient was asymptomatic without progression of mitral regurgitation and had normal blood pressure. This case provides an example of a rare congenital pathology.
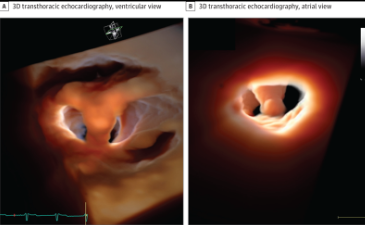
3-Dimensional (3D) transthoracic echocardiographic images. Acquisition with zoom 3D and postprocess with 3D transillumination (FlexiLight [GE]). Transillumination allows for light-source positioning in front or behind the mitral valve thereby improving the anatomic definition and diagnostic accuracy. Both the ventricular (A) and atrial (B) views show a double-orifice mitral valve with a single fibrous annulus and a complete bridge.
(17). Sanjay H Chotirmall. Bronchiectasis: a global disease necessitating global solutions. Lancet Respir Med. 2023
René Laennec’s description of bronchiectasis, almost 200 years ago, serves as a timely reminder that if one does not look for something, we shall never find it. The European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC) provides the most comprehensive analysis of bronchiectasis clinical care available to date. With 16963 individuals enrolled across 27 European countries and Israel, consistent quality-controlled methodology, including longitudinal follow up, it serves as a reminder of the substantial unmet need in bronchiectasis clinical care and research. This snapshot of real-world practice will guide recalibration of clinical practice guidelines, clarify the educational needs of patients and physicians, and provide fresh directions for research.
Of note, the study’s findings of idiopathic and post-infection as the commonest causes are a sobering reminder of how little is still known about this disease and the key geographical and global challenges faced. Remarkable differences in microbiology further attest to geographic influences where higher frequencies of
Pseudomonas aeruginosa
occur in southern Europe, whereas Haemophilus influenzae predominates in northern Europe and the UK. Significant burden on patients and health-care systems is exemplified by the reported median of two exacerbations annually, with more than 25% necessitating hospitalisation, most pronounced in central or eastern Europe where disease severity is highest. Such geographic heterogeneity extends to treatment and adherence to established guidelines, further complicating care delivery, clinical trials, and research.
Shared challenges emerge from this work: global challenges necessitating global solutions. First, inherent disease heterogeneity impacts clinical trial design, conduct, and success with further challenges posed in drafting generalisable clinical guidelines. Such heterogeneity is even more profound when considered globally: bronchiectasis in India is most prevalent in young men with more than 33% of cases having a post-tuberculosis cause. In contrast, almost two thirds of people with bronchiectasis in the US Registry are older women with non-tuberculous mycobacterial (NTM) disease. Second, geographic variation, even across a single continent, contributes substantially to disease endophenotypes, treatment variation, and exacerbation differences. Although Pseudomonas is universally recognised, differences in bronchiectasis microbiology exist. Enterobacteriacae occurs in one in ten individuals in India and portends toward increased mortality, whereas H influenzae and Moraxella catarrhalis are relatively infrequent outside Europe. Disease severity is significant in Australia whereas exacerbations and hospitalisations, although high in Europe, remain greatest in India. Third, meaningful deviations from recommended clinical guidelines is a real, worldwide issue even in developed locations, and one that compounds inequity between patients, health-care systems, and countries. Differences in diagnostic pathways, monitoring, treatment access, and care delivery all remain fundamental challenges to the global bronchiectasis family. Finally, the high disease burden, compounded by an ageing global population, is becoming increasingly evident and no longer can or should the disease be viewed as rare or orphan. Of note, high disease burden exists outside Europe, in countries where tuberculosis is endemic, presenting important challenges to patients, physicians, and health-care systems, including access to specialist microbiology, trained physiotherapists, and treatments such as inhaled antibiotics. As bronchiectasis represents a final outcome from several different diseases, education and training of physicians beyond the respiratory field is required. The success of EMBARC further provides an opportunity to evaluate race and ethnicity in bronchiectasis as inequality in care and clinical outcomes are shown in other respiratory diseases and were forefront during the COVID-19 pandemic. The US Bronchiectasis and NTM Research Registry comprises of predominantly White participants (89.5%), followed by Hispanic (4.3%), Asian (3.7%), and African Americans (2 5%), respectively, showing discordance between registry ascertainment and representativeness of its overall population. Although there are increasing calls to avoid race and ethnic constructs, this is arguably important in assessing the generalisability of data and other potential contributors such as socioeconomic or cultural aspects to bronchiectasis clinical care and outcomes.
Although this work highlights challenges, it also offers opportunities. The disease heterogeneity partially explains variable geographic responses seen in the RESPIRE and ORBIT clinical trials. Whether microbiological variation relates to environmental influence is another novel area for research. Discovering almost 6500 patients with idiopathic disease represents a rich source for genome sequencing and understanding pathogenesis at an unprecedented scale, although it raises the question as to whether bronchiectasis could have been prevented if diagnosed and managed early, a now well accepted treatment goal in children. Perhaps the views of researchers and clinicians are evolving to realise that adult bronchiectasis might be reversible and remains a challenge for physicians caring for adults with bronchiectasis.
The EMBARC registry represents a valuable commodity not just for research but for patients to inform clinical care and health policy. It represents a victory of collaboration and teamwork, but importantly that bronchiectasis can no longer be neglected, considered rare, or labelled orphan. Calls to action might not be new but the cries have never been stronger.
(18). Philis-Tsimikas et al. Switching to once-weekly insulin icodec versus once-daily insulin degludec in individuals with basal insulin-treated type 2 diabetes (ONWARDS 2): a phase 3a, randomised, open label, multicentreh3>treat-to-target trial. Lancet Diabetes Endocrinol. 2023
Background
Insulin icodec (icodec) is a once-weekly basal insulin currently under development. ONWARDS 2 aimed to assess the efficacy and safety of once-weekly icodec versus once-daily insulin degludec (degludec) in basal insulin-treated type 2 diabetes.
Methods
This 26-week, randomised, open-label, active-controlled, multicentre, treat-to-target phase 3a trial was conducted in 71 sites in nine countries. Eligible participants with type 2 diabetes inadequately controlled on once-daily or twice-daily basal insulin, with or without non-insulin glucose-lowering agents, were randomly assigned (1:1) to once-weekly icodec or once-daily degludec. The primary outcome was change from baseline to week 26 in HbA1c; the margin used to establish non-inferiority of icodec compared with degludec was 0.3 percentage points. Safety outcomes (hypoglycaemic episodes and adverse events) and patient-reported outcomes were also assessed. The primary outcome was evaluated in all randomly assigned participants; safety outcomes were evaluated descriptively based on all randomly assigned participants who received at least one dose of trial product, with statistical analyses based on all randomly assigned participants. This trial is registered with ClinicalTrials.gov, NCT04770532, and is now complete.
Findings
Between March 5 and July 19, 2021, 635 participants were screened, of whom 109 were ineligible or withdrew, and 526 were randomly assigned to icodec (n = 263) or degludec (n = 263). From a mean baseline of 8.17% (icodec; 65.8 mmol/mol) and 8.10% (degludec; 65.0 mmol/mol), HbA1c was reduced to a greater extent with icodec than degludec (7.20% vs 7.42% [55.2 vs 57.6 mmol/mol], respectively) at week 26. This translates to an estimated treatment difference (ETD) of -0.22 percentage points (95% CI -0.37 to -0.08) or -2.4 mmol/mol (95% CI -4.1 to -0.8), demonstrating non-inferiority (p < 0.0001) and superiority (p = 0.0028). The estimated mean change from baseline to week 26 in bodyweight was +1.40 kg for icodec and -0.30 kg for degludec (ETD 1.70 [95% CI 0.76 to 2.63]). Overall rates of combined level 2 or level 3 hypoglycaemia were less than one event per patient-year of exposure for both groups (0.73 [icodec] vs 0.27 [degludec]; estimated rate ratio 1.93 [95% CI 0.93 to 4.02]). Overall, 161 (61%) of 262 participants receiving icodec and 134 (51%) of 263 participants receiving degludec experienced an adverse event; 22 (8%) and 16 (6%), respectively, experienced a serious adverse event. One serious adverse event (degludec) was assessed as being possibly related to treatment. No new safety issues were identified in relation to icodec compared with degludec in this trial.
Interpretation
Among adults with basal insulin-treated type 2 diabetes, treatment with once-weekly icodec versus once-daily degludec demonstrated non-inferiority and statistical superiority in HbA1c reduction after 26 weeks, associated with modest weight gain. Overall rates of hypoglycaemia were low, with numerically but not statistically significantly higher event rates of level 2 or level 3 hypoglycaemia with icodec versus degludec.
(19). Anura V Kurpad. Good example of a Negative Trial! Efficacy of maternal vitamin B12 supplementation for improving infant outcomes in settings with high deficiency. Lancet 2023;401(10387):P1476-1478.
Maternal vitamin B12 supplementation to improve early neurodevelopment in infants has been proposed for some time now because vitamin B12 is a neurotropic vitamin, and infant neurodevelopment and growth are important dimensions for attained human capital and a healthy and successful adult life. In The Lancet, Ram K Chandyo and colleagues 1 report a community-based, double-blind, randomised controlled trial in a Nepalese region, which is endemic for biochemical vitamin B12 deficiency. Chandyo and colleagues 1 evaluated the effect of daily maternal vitamin B12 supplementation (50 μg per day) from early pregnancy until 6 months post partum on infant growth and neurodevelopment. The authors deserve compliments for their large and rigorous efficacy trial, which included 800 pregnant women, with 400 (50%) women randomly assigned to receive vitamin B12 supplementation and 400 (50%) women randomly assigned to the placebo group (mean age was 27.7 years [SD 4.0]). At baseline, 569 (71%) of the women had plasma vitamin B12 concentrations indicating low or marginal status (<221 pmol/L). The primary outcomes were length-for-age Z-scores (LAZ) at age 12 months, and the cognitive composite score of the Bayley Scales of Infant and Toddler Development, 3rd edition (Bayley-III) at age 6 months and 12 months. In this trial, there was no improvement in infant growth or neurodevelopment associated with vitamin B12 supplementation. The mean LAZ score at age 12 months was -0.57 (SD 1.03) in the vitamin B12 group and -0.55 (1.03) in the placebo group with a mean difference of -0.02 (95% CI -0.16 to 0.13). The mean cognitive composite scores (ie, at age 6 and 12 months) were 97.7 (SD 10.5) in the vitamin B12 group and 97.1 (10.2) in the placebo group, with a mean difference of 0.5 (-0.6 to 1.7). There was also no significant difference in infant haemoglobin concentrations despite a substantial biomarker response and improved vitamin B12 status among mothers and infants.
(20). Viola D’Ambrosio et al. Dementia, Almonds and AKI! Lancet 2023;401(10387):P1530.
Hyperoxaluric acute kidney injury and frontotemporal dementia
A 58-year-old man, who after reporting several days of abdominal pain was found to have acute kidney injury, was transferred to our unit from a regional hospital.
In the preceding 6 months, the patient had been diagnosed with frontotemporal dementia; he had no personal or family history of nephrolithiasis, bowel disease, or weight loss. Notably, the year before this presentation, his kidney function had been found to be normal with the serum creatinine concentration recorded as 71 μmol/L (normal range 60-115).
On examination, the patient was clinically well with a blood pressure of 122/66 mm Hg, heart rate of 95 beats per min, respiratory rate of 18 breaths per min, and oxygen saturation of 95% on room air.
Laboratory investigations confirmed acute kidney injury-his serum creatinine concentration was 703 μmol/L with preserved urinary output; his remaining serum biochemistry was unremarkable. The urinary protein/creatinine ratio was 39 mg/mmol (normal range 0-12.5).
The patient was admitted to the nephrology ward for a kidney biopsy which showed acute tubular injury with abundant intratubular calcium oxalate crystals; the background kidney was healthy, with little scarring, and only 1/14 obsolete glomeruli
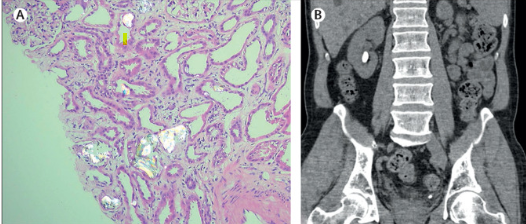
A detailed dietary history found that the patient had been eating 500-1000 g of almonds daily over the last four years-corresponding to approximately 2-4 g of oxalate per day. He had no evidence of malabsorption; his faecal elastase concentration was >500 ug/g (typical range 200 to less than 500).
A CT of the kidney, ureter, and bladder showed a non-obstructing 1.4 cm calculus in the lower pole of the right kidney and a non-obstructing 0.6 cm calculus in the distal left ureter (figure). We concluded the patient had a diet-related secondary hyperoxaluria; frontotemporal dementia is associated with unusual, compulsive eating habits.
As he was asymptomatic, we decided to manage him conservatively; the patient was started on a low-oxalate, high-calcium diet with a high fluid intake and reviewed regularly. At his last appointment, the patient’s laboratory results showed his serum creatinine concentration was improving (478 μmol/L).
Hyperoxaluria causes calcium oxalate stones by raising urinary saturation of calcium oxalate; hyperoxaluria can result from ingestion of oxalate-rich foods, such as rhubarb, spinach, beetroot, almonds-as in our case-and chocolate. Hyperoxaluria is less common than hypercalciuria as a cause of calcium oxalate stones.
Non-obstructive kidney stones of less than 15 mm can be treated conservatively and monitored closely; an increase in the size of the stone or complications, such as infections, may result in a more proactive approach.
(21). Joo Myung Lee et al. Intravascular Imaging-Guided or Angiography-Guided Complex PCI. N Engl J Med. 2023;388:1668-1679.
Background
Data regarding clinical outcomes after intravascular imaging-guided percutaneous coronary intervention (PCI) for complex coronary-artery lesions, as compared with outcomes after angiography-guided PCI, are limited.
Methods
In this prospective, multicenter, open-label trial in South Korea, we randomly assigned patients with complex coronary-artery lesions in a 2:1 ratio to undergo either intravascular imaging-guided PCI or angiography-guided PCI. In the intravascular imaging group, the choice between intravascular ultrasonography and optical coherence tomography was at the operators’ discretion. The primary end point was a composite of death from cardiac causes, target-vessel-related myocardial infarction, or clinically driven target-vessel revascularization. Safety was also assessed.
Results
A total of 1639 patients underwent randomization, with 1092 assigned to undergo intravascular imaging-guided PCI and 547 assigned to undergo angiography-guided PCI. At a median follow-up of 2.1 years (interquartile range, 1.4 to 3.0), a primary end-point event had occurred in 76 patients (cumulative incidence, 7.7%) in the intravascular imaging group and in 60 patients (cumulative incidence, 12.3%) in the angiography group (hazard ratio, 0.64; 95% confidence interval, 0.45 to 0.89; P = 0.008). Death from cardiac causes occurred in 16 patients (cumulative incidence, 1.7%) in the intravascular imaging group and in 17 patients (cumulative incidence, 3.8%) in the angiography group; target-vessel-related myocardial infarction occurred in 38 (cumulative incidence, 3.7%) and 30 (cumulative incidence, 5.6%), respectively; and clinically driven target-vessel revascularization in 32 (cumulative incidence, 3.4%) and 25 (cumulative incidence, 5.5%), respectively. There were no apparent between-group differences in the incidence of procedure-related safety events.
Conclusions
Among patients with complex coronary-artery lesions, intravascular imaging-guided PCI led to a lower risk of a composite of death from cardiac causes, target-vessel-related myocardial infarction, or clinically driven target-vessel revascularization than angiography-guided PCI.
(22). Nan Zhang, et al. Red Flag on Electrocardiogram Findings in a Patient With Lung Cancer. JAMA Intern Med. 2023.
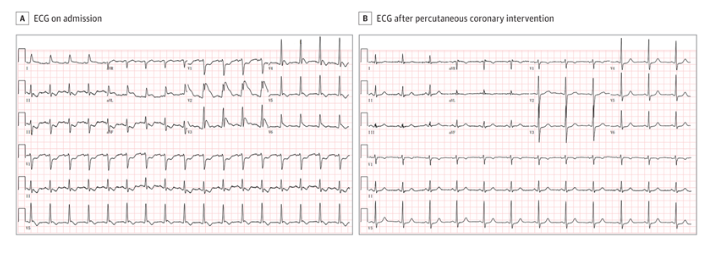
A patient in their early 70s with a history of lung cancer was admitted to the oncology department for routine assessment and next cycle of anticancer therapy. Previously, the patient had undergone a left upper lobectomy followed by 19 doses of pembrolizumab for lung cancer; the 20th dose was to be administered during this visit. The patient had a medical history of well-controlled diabetes and immune-related hypothyroidism associated with pembrolizumab use, and no other comorbidities or noteworthy family medical history.
On admission, the patient denied any symptoms and had normal vital signs. However, the initial electrocardiogram (ECG) findings showed alarming features that alerted the physicians who ordered additional investigations (Figure, A). The patient’s troponin I level was 0.063 ng/mL (reference, <0.034 ng/mL; for µg/L, multiply by 1); brain-type natriuretic peptide level was 197 pg/mL (reference, <125 pg/mL; for ng/L, multiply by 1); and serum calcium level was 8.72 mg/dL (reference range, 8.5-10.5 mg/dL; for mmol/L, multiply by 0.25). Ten minutes after the initial ECG was performed, the patient complained of sudden-onset squeezing precordial chest pain with back pain and nausea.
A, On admission, ECG findings showed a sinus tachycardia at a rate of 101 beats per minute with prominent notch-type J waves through leads V2 to V6, at least 0.15 mV ST-segment elevation at J point in leads I and aVL, as well as ST-segment depression in inferior leads and lead V1. B, After percutaneous coronary intervention, ECG findings showed resolution of ST-segment changes and J waves.
Questions: Which findings on the admission ECG are concerning? Considering the patient’s long-term history of pembrolizumab use, what are the potential mechanisms of the ECG changes?
Interpretation
The ECG performed on admission showed a sinus tachycardia with prominent notch-type J waves in leads V2 to V6, ST-segment elevation of at least 0.15 mV at J point in leads I and aVL, and ST-segment depression in the inferior leads and lead V1 (Figure, A). Although the patient had experienced no symptoms during the initial ECG examination, the appearance of prominent J waves parallel to the coronary artery distribution and long-term pembrolizumab use was concerning and suggestive of acute coronary syndrome (ACS). Subsequent onset of chest pain and elevated troponin levels further confirmed the initial diagnosis of ACS.
Clinical Course
Considering that the ECG findings on admission were highly suggestive of ACS and that J waves during acute ischemia are highly predictive for ventricular fibrillation, continuous telemetry monitoring was promptly initiated for this patient. After appearance of the subsequent symptoms and the emergency laboratory test results were obtained, the patient received an oral loading dose of aspirin and ticagrelor as well as intravenous heparin. Then the patient was transferred to the catheterization laboratory for emergency coronary angiography testing that revealed a 95% left main coronary ostial stenosis and a subtotal occlusion of the proximal left anterior descending artery. An ECG tracing obtained after successful angioplasty and stent implantation showed resolution of ST-segment changes and disappearance of J waves (Figure, B). Bedside echocardiography revealed hypokinesia of the left ventricular anterior and lateral walls with an ejection fraction of 47%.
Because emerging evidence indicates a potential role of immune checkpoint inhibitor (ICI) in the development and exacerbation of atherosclerosis, pembrolizumab treatment was discontinued, and afatinib use was initiated. The patient made an uneventful recovery and received follow-up care in the cardio-oncology clinic.
Discussion
In recent years, ICI has revolutionized the treatment of advanced malignant neoplasms, although improved cancer survival often comes with increased risk of various immune-related adverse events (irAEs). Much interest has been focused on ICI-related myocarditis, and emerging preclinical and clinical studies have also indicated that ICI may also be associated with the development and exacerbation of atherosclerosis. Immune checkpoint pathways play a substantially protective role in atherogenesis and progression to advanced plaque phenotype; however, inhibition of these pathways has been associated with proinflammatory changes,increased atherosclerotic lesion size, lesion macrophage content, and enhanced plaque T-cell activation, which may develop into more advanced atherosclerosis. In the largest study to our knowledge, Drobni and colleagues observed a 7-fold increased risk of myocardial infarction in patients receiving ICI than among those without more than 2 years of follow-up, and a 3-fold increased rate of atherosclerotic plaque progression compared with the rate before ICI treatment.
In the present case report, the patient had well-controlled diabetes and had no history of smoking or other cardiovascular risk factors. Additionally, it is notable that this patient developed other irAEs, including hypothyroidism. This lends further support to our hypothesis that long-term ICI therapy may have been the culprit of severe atherosclerosis, especially given that among patients treated with ICI, the group of patients who experienced irAEs had a significantly higher risk of atherosclerosis exacerbation compared with the group that did not experience any irAEs.
The J wave, which is also known as the Osborn wave
, was defined as positive when it was 0.1 mV or higher than the isoelectric line in 2 or more contiguous leads. This may be observed in several pathologic conditions, such as hypercalcemia, hypothermia, brain injury, Brugada syndrome, early repolarization, and idiopathic ventricular fibrillation.In addition, vasospastic angina and acute myocardial infarction have also been considered as important causes of J waves, namely the ischemia-induced J waves seen in this patient. The ischemia-induced J waves are registered in ECG leads facing the ischemic territory and are usually followed by ST-segment elevation in persistent ischemia, which could facilitate localizing the infarct-related artery. The ischemia-induced J waves represent an initial and transient response to acute myocardial ischemia, whereas the electrophysiological basis is not fully understood. Recent studies have suggested that the ischemia-induced J waves may be associated with both a conduction delay in the ischemic myocardium and accentuation of the transient outward potassium current (Ito)-mediated action potential notch during early ventricular repolarization in the epicardium but not in the endocardium, which creates a transmural voltage gradient. A voltage gradient during early acute myocardial ischemia can induce phase 2 reentry and associated ventricular fibrillation. Therefore, prominent J waves with ST-segment elevation have been considered to be a warning sign for the development of ventricular fibrillation in myocardial ischemia.
In this case report, we describe a rare case of ACS featured by prominent J waves as a possible irAE in a patient with cancer being treated with long-term ICI. This patient’s experience highlights the need to treat ICI therapy as a modifier of atherosclerotic cardiovascular risk and suggests that candidates for ICI therapy undergo a comprehensive cardiovascular risk evaluation, optimization of preventive medical therapy, and close cardiac monitoring.
(23). Tadarro L. Richardson, et al. Primary Occurrence of Cardiovascular Events After Adding Sodium-Glucose Cotransporter-2 Inhibitors or Glucagon-like Peptide-1 Receptor Agonists Compared With Dipeptidyl Peptidase-h3>Inhibitors: A Cohort Study in Veterans With Diabetes. Ann Intern Med. 2023
Background
The effectiveness of glucagon-like peptide-1 receptor agonists (GLP1RA) and sodium-glucose cotransporter-2 inhibitors (SGLT2i) in preventing major adverse cardiac events (MACE) is uncertain for those without preexisting cardiovascular disease.
Objective
To test the hypothesis that MACE incidence was lower with the addition of GLP1RA or SGLT2i compared with dipeptidyl peptidase-4 inhibitors (DPP4i) for primary cardiovascular prevention.
Design
Retrospective cohort study of U.S. veterans from 2001 to 2019.
Setting
Veterans aged 18years or older receiving care from the Veterans Health Administration, with data linkage to Medicare, Medicaid, and the National Death Index.
Patients
Veterans adding GLP1RA, SGLT2i, or DPP4i onto metformin, sulfonylurea, or insulin treatment alone or in combination. Episodes were stratified by history of cardiovascular disease.
Measurements
Study outcomes were MACE (acute myocardial infarction, stroke, or cardiovascular death) and heart failure (HF) hospitalization. Cox models compared the outcome between medication groups using pairwise comparisons in a weighted cohort adjusted for covariates.
Results
The cohort included 28759 GLP1RA versus 28628 DPP4i weighted pairs and 21200 SGLT2i versus 21170 DPP4i weighted pairs. Median age was 67years, and diabetes duration was 8.5years. Glucagon-like peptide-1 receptor agonists were associated with lower MACE and HF versus DPP4i (adjusted hazard ratio [aHR], 0.82 [95% CI, 0.72 to 0.94]), yielding an adjusted risk difference (aRD) of 3.2 events (CI, 1.1 to 5.0) per 1000 person-years. Sodium-glucose cotransporter-2 inhibitors were not associated with MACE and HF (aHR, 0.91 [CI, 0.78 to 1.08]; aRD, 1.28 [-1.12 to 3.32]) compared with DPP4i.
Limitation
Residual confounding; use of DPP4i, GLP1RA, and SGLT2i as first-line therapies were not examined.
Conclusion
The addition of GLP1RA was associated with primary reductions of MACE and HF hospitalization compared with DPP4i use; SGLT2i addition was not associated with primary MACE prevention.
(23). M Bilal Ahmed, et al. 32-Year-Old Man With Chronic Left Ventricular Dysfunction. JAMA Cardiol. 2020 Jun 1;5(6):726-727.
A 32-year-old man with a diagnosis of dilated cardiomyopathy sought care for angina and dyspnea with exertion. His chest pain and dyspnea were chronic and had recently increased in frequency. His cardiomyopathy followed a diagnosis of myocarditis after repeated putative chest colds and chest pain at age 14 years, at which time the ejection fraction was reported to be 30%. The results of a graded exercise stress test at 22 years were unremarkable.
On examination, he was afebrile. His heart rate was 68 beats per minute, his blood pressure was 114/77 mm Hg, and his examination was notable for an absence of jugular venous distension, peripheral edema, and murmurs or extra heart sounds. His electrocardiogram, shown below , unchanged from his electrocardiogram at age 14 years.
What are the two conduction system anomalies seen here?
(24). David Simmons, et al. Treatment of Gestational Diabetes Mellitus Diagnosed Early in Pregnancy. 2023
Background
Whether treatment of gestational diabetes before 20 weeks’ gestation improves maternal and infant health is unclear.
Methods
We randomly assigned, in a 1:1 ratio, women between 4 weeks’ and 19 weeks 6 days’ gestation who had a risk factor for hyperglycemia and a diagnosis of gestational diabetes (World Health Organization 2013 criteria) to receive immediate treatment for gestational diabetes or deferred or no treatment, depending on the results of a repeat oral glucose-tolerance test [OGTT] at 24 to 28 weeks’ gestation (control). The trial included three primary outcomes: a composite of adverse neonatal outcomes (birth at <37 weeks’ gestation, birth trauma, birth weight of ≥4500 g, respiratory distress, phototherapy, stillbirth or neonatal death, or shoulder dystocia), pregnancy-related hypertension (preeclampsia, eclampsia, or gestational hypertension), and neonatal lean body mass.
Results
A total of 802 women underwent randomization; 406 were assigned to the immediate-treatment group and 396 to the control group; follow-up data were available for 793 women (98.9%). An initial OGTT was performed at a mean (±SD) gestation of 15.6±2.5 weeks. An adverse neonatal outcome event occurred in 94 of 378 women (24.9%) in the immediate-treatment group and in 113 of 370 women (30.5%) in the control group (adjusted risk difference, -5.6 percentage points; 95% confidence interval ci, -10.1 to -1.2). Pregnancy-related hypertension occurred in 40 of 378 women (10.6%) in the immediate-treatment group and in 37 of 372 women (9.9%) in the control group (adjusted risk difference, 0.7 percentage points; 95% CI, -1.6 to 2.9). The mean neonatal lean body mass was 2.86 g in the immediate-treatment group and 2.91 g in the control group (adjusted mean difference, -0.04 g; 95% CI, -0.09 to 0.02). No between-group differences were observed with respect to serious adverse events associated with screening and treatment.
Conclusions
Immediate treatment of gestational diabetes before 20 weeks’ gestation led to a modestly lower incidence of a composite of adverse neonatal outcomes than no immediate treatment; no material differences were observed for pregnancy-related hypertension or neonatal lean body mass. (Funded by the National Health and Medical Research Council and others; TOBOGM Australian New Zealand Clinical Trials
(25). Ioannis Gallos, et al. Randomized Trial of Early Detection and Treatment of Postpartum Hemorrhage. 2023.
Background
Delays in the detection or treatment of postpartum hemorrhage can result in complications or death. A blood-collection drape can help provide objective, accurate, and early diagnosis of postpartum hemorrhage, and delayed or inconsistent use of effective interventions may be able to be addressed by a treatment bundle.
Methods
We conducted an international, cluster-randomized trial to assess a multicomponent clinical intervention for postpartum hemorrhage in patients having vaginal delivery. The intervention included a calibrated blood-collection drape for early detection of postpartum hemorrhage and a bundle of first-response treatments (uterine massage, oxytocic drugs, tranexamic acid, intravenous fluids, examination, and escalation), supported by an implementation strategy (intervention group). Hospitals in the control group provided usual care. The primary outcome was a composite of severe postpartum hemorrhage (blood loss, ≥1000 ml), laparotomy for bleeding, or maternal death from bleeding. Key secondary implementation outcomes were the detection of postpartum hemorrhage and adherence to the treatment bundle.
Results
A total of 80 secondary-level hospitals across Kenya, Nigeria, South Africa, and Tanzania, in which 210,132 patients underwent vaginal delivery, were randomly assigned to the intervention group or the usual-care group. Among hospitals and patients with data, a primary-outcome event occurred in 1.6% of the patients in the intervention group, as compared with 4.3% of those in the usual-care group (risk ratio, 0.40; 95% confidence interval [CI], 0.32 to 0.50; P<0.001). Postpartum hemorrhage was detected in 93.1% of the patients in the intervention group and in 51.1% of those in the usual-care group (rate ratio, 1.58; 95% CI, 1.41 to 1.76), and the treatment bundle was used in 91.2% and 19.4%, respectively (rate ratio, 4.94; 95% CI, 3.88 to 6.28).
Conclusions
Early detection of postpartum hemorrhage and use of bundled treatment led to a lower risk of the primary outcome, a composite of severe postpartum hemorrhage, laparotomy for bleeding, or death from bleeding, than usual care among patients having vaginal delivery. (Funded by the Bill and Melinda Gates Foundation)
(26). Katharina S. Shaw et al. Eosinophilic Fasciitis. N Engl J Med. 2023;388:e65.
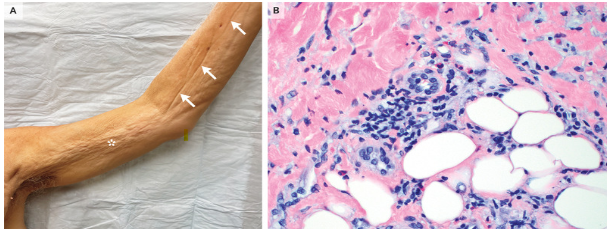
A 66-year-old man presented to the dermatology clinic with an 8-month history of progressively worsening, painful skin tightening and swelling of his arms and legs. He had received treatment for possible scleroderma with oral glucocorticoids and methotrexate, but the symptoms had progressed. On physical examination, there was symmetric, woody induration of the trunk, arms, and legs, sparing the hands and feet. The involved skin had a dimpled appearance (peau d’orange changes) (Panel A, asterisk). Elevation of the arms resulted in visible indentations along the course of superficial veins, a finding known as the “groove sign” (Panel A, arrows). Elbow contractures were also noted. Laboratory studies were notable for an absolute eosinophil count of 2040 cells per cubic millimeter (reference range, 15 to 500) and a normal antinuclear antibody level. A skin biopsy of the left arm was performed. Histopathological examination showed a perivascular and interstitial inflammatory infiltrate of lymphocytes and eosinophils in the deep reticular dermis and subcutis (Panel B, hematoxylin and eosin stain). A diagnosis of eosinophilic fasciitis was made. Owing to the severity of the patient’s symptoms and the lack of a previous response to oral glucocorticoids and methotrexate, treatment with intravenous methylprednisolone, oral mycophenolate mofetil, and intravenous immune globulin was initiated. At 4 months of follow-up, his symptoms had markedly abated.
(27). Rohit Kothari et al. Dietary Zinc Deficiency-Associated Dermatitis in a Child. N Engl J Med. 2023;388:1799.

A 2-year-old boy was referred to the dermatology clinic with an 8-month history of rash, hair loss, and watery diarrhea. The child had been exclusively breast-fed until 6 months of age, at which time a vegetarian solid-food diet of produce and natural grains had been introduced. When the child was weaned from breast milk to cow’s milk at 16 months of age, the symptoms had started. On examination, the child was irritable; he had angular cheilitis, alopecia, and erosions with crusted borders across the face and scalp and around the mouth, eyes, and ears (Panels A and B). The rash also involved the perianal region, trunk, and all four limbs (Panel C). Laboratory testing showed a serum zinc level of 0.32 μg per milliliter (reference range, 0.65 to 1.10) and a low alkaline phosphatase level. Zinc is a cofactor for alkaline phosphatase activity, and therefore a low alkaline phosphatase level may be seen in a patient with zinc deficiency. A diagnosis of dietary zinc deficiency-associated dermatitis was made. Oral zinc supplementation and dietary changes were recommended. At a 3-week follow-up visit, the alopecia and dermatitis had abated (Panel D). When zinc supplementation was stopped 3 months later, the symptoms did not recur.
(28). Abi Rimmer. Antidepressants lack evidence for treating chronic pain, says Cochrane. BMJ 2023;381:p1056.
Most antidepressants used for chronic pain are being prescribed with insufficient evidence of their effectiveness, a Cochrane review has found.1
Of the most commonly used antidepressants studied-including amitriptyline, fluoxetine, citalopram, paroxetine, sertraline, and duloxetine-researchers found that only the latter showed some evidence for pain relief. But the evidence for long term efficacy was lacking as the average length of the studies was 10 weeks.
Lead author Tamar Pincus, from the University of Southampton, said, “Our review found no reliable evidence for the long-term efficacy of any antidepressant, and no reliable evidence for their safety for chronic pain at any point. Although we found that duloxetine provided short term pain”
(29). Mario Gaudino et al. Current concepts in coronary artery revascularisation. Lancet. 2023 May 13;401(10388):1611-1628.
Coronary artery revascularisation can be performed surgically or percutaneously. Surgery is associated with higher procedural risk and longer recovery than percutaneous interventions, but with long-term reduction of recurrent cardiac events. For many patients with obstructive coronary artery disease in need of revascularisation, surgical or percutaneous intervention is indicated on the basis of clinical and anatomical reasons or personal preferences. Medical therapy is a crucial accompaniment to coronary revascularisation, and data suggest that, in some subsets of patients, medical therapy alone might achieve similar results to coronary revascularisation. Most revascularisation data are based on prevalently White, non-elderly, male populations in high-income countries; robust data in women, older adults, and racial and other minorities, and from low-income and middle-income countries, are urgently needed.
The summary is brilliant!
(30). Sigrid Lundberg, et al. We can go further in non-immunosuppressive treatment of IgA nephropathy. Lancet. 2023 May 13;401(10388):1548-1550.
More than 50 years after the description of IgA nephropathy as Berger’s disease, 20-40% of affected individuals still progress to end-stage kidney disease within 10-20 years of diagnosis, which negatively affects life expectancy. 1 Glucocorticoids can halt progression in some patients but rarely prevent the final development of end-stage kidney disease, and side-effects limit the intensity and duration of treatment. 2 , 3 A challenge for the assessment of treatment effects in IgA nephropathy is the usual long time-course to traditional outcomes of doubling of serum creatinine, end-stage kidney disease, or death. A breakthrough has been the Kidney Health Initiative (KHI) project that, on the basis of published trials, evaluated and confirmed the predictive value of proteinuria reduction on this combined outcome. This resulted in the KHI recommendation of proteinuria reduction as a surrogate efficacy endpoint for accelerated approval of new therapies for IgA nephropathy by the US Food and Drug Administration (FDA). 4 Since then, an increasing number of new therapies are under investigation for IgA nephropathy. Recently, targeted-release budesonide for a course of 9 months has been approved as the first specific immunosuppressive treatment in IgA nephropathy. 5 Sustained proteinuria reduction is essential for the prognosis of IgA nephropathy, 6 which highlights the need for additional non-toxic treatments that can be given in the long term and at different disease stages.
(31). Antonia W Shand, et al. Anaemia in pregnancy: a major global health problem. Lancet. 2023;401(10388):1550-1551.
Anaemia, most commonly due to iron deficiency, is a common problem in pregnant women worldwide, affecting nearly 50% of pregnancies globally.1 Anaemia is associated with maternal morbidity, including impaired quality of life, a need for blood transfusions, post-partum haemorrhage, and maternal mortality.1 In addition, anaemia is associated with adverse fetal outcomes such as preterm birth, small for gestational age, and perinatal death.1 Impaired neurodevelopmental outcomes of the child have also been reported in some studies.
Oral iron is the main therapy for prevention and treatment of iron deficiency and iron deficiency anaemia. Oral iron is cheap and readily available but might exacerbate or cause common gastrointestinal symptoms of pregnancy such as nausea, vomiting, and constipation, which can lead to poor tolerance and adherence to treatment. Numerous meta-analyses show possible greater haematological benefit of intravenous iron compared with oral iron, and use of more expensive intravenous iron is increasing.
Guidelines have been developed to improve care of pregnant women with iron deficiency and iron deficiency anaemia.5 However, these guidelines are not based on high-quality evidence. There is little evidence on the role of universal oral iron supplementation and, for oral iron, the optimal iron salt, dose, timing of the dose (ie, morning vs evening), and frequency of dosing (ie, twice daily, daily, or alternate daily) is not known. For intravenous iron, the optimal preparation, dose, and gestation are unknown.
Sant-Rayn Pasricha and colleagues present a large open-label randomised controlled trial including pregnant women with predominantly moderate to severe anaemia (haemoglobin 7-10 g/dL) in Malawi.6 430 women were randomly assigned to receive intravenous iron (ferrous carboxymaltose up to 1000 mg) and 432 to receive oral iron (ferrous sulphate 60 mg twice daily). Mean age was 22.4 years and women were at a median of 22 weeks’ gestation. 366 (43%) of 844 women had baseline iron deficiency and all women had malaria excluded. The primary maternal outcome was anaemia at 36 weeks’ gestation. The primary neonatal outcome was birthweight. There was no significant reduction in anaemia prevalence at 36 weeks’ gestation in women randomly assigned to ferrous carboxymaltose compared with those assigned to oral iron (ferrous carboxymaltose 179 [52%] of 341 vs oral iron 189 [57%] of 333; prevalence ratio [PR] 0.92 [95% CI 0.81 to 1.06]). There was no significant change in birthweight (mean difference -3.1 g [95% CI -75 to 69]). The only significant reduction in anaemia in women randomly assigned to ferrous carboxymaltose was at 4 weeks’ post-treatment (ferrous carboxymaltose 306 [77%] of 399 vs oral iron 329 [84%] of 390; PR 0.91 [95% CI 0.85 to 0.97]). There was no change in any infection (ferrous carboxymaltose 103 [24%] of 430 vs oral iron 87 [20%] of 432; risk ratio [RR] 1.19 [95% CI 0.92 to 1.52]). There was no difference in the composite adverse birth outcome (ferrous carboxymaltose 158 [40%] of 398 vs oral iron 155 [38%] of 407; RR 1.04 [95% CI 0.88 to 1.24]), nor any of its components, including pregnancy loss or stillbirth. Women who received intravenous iron were less likely to have iron deficiency anaemia at delivery than those who received oral iron (ferrous carboxymaltose 29 [9%] of 324 vs oral iron 93 [29%] of 321; PR 0.30 [95% CI 0.20 to 0.44]).
The strength of the study is the pragmatic randomised trial design including women with moderate to severe anaemia. A weakness of the study is that the cause of anaemia was not determined. There was high prevalence of recently treated malaria (61%), and most participants (57%) did not have iron deficiency. 55% (368/674) of women remained anaemic at 36 weeks’ gestation, rising to 75% (37/50) for women who had severe baseline anaemia. Another limitation was that the trial was open label; however, blinding to brown intravenous iron might be difficult. Adherence was also unable to be measured, partly due to COVID-19 pandemic disruption. Pasricha and colleagues used standard doses and preparations of iron, although studies suggest other preparations might be more effective than ferrous sulphate.7 Once daily or alternate day dosing with 60 mg might be just as effective;8 however, these regimens have not been tested in randomised trials in pregnant women. Despite being a negative trial in terms of anaemia, fetal growth, and perinatal death outcomes, this trial gives important information about the relative safety of intravenous iron treatment of anaemia predominantly in the second trimester, in a setting with high prevalence of infections including malaria and HIV. Improvements in testing for iron deficiency (eg, point-of-care ferritin testing) are required, so that women with anaemia in low-resource settings can receive targeted therapy. In addition, it is to be hoped long-term infant outcomes will be reported.
Further high-quality studies in pregnant women with iron deficiency and iron deficiency anaemia in various settings are urgently needed. Short-term maternal and fetal outcomes, patient-reported outcomes, long-term childhood outcomes, and cost effectiveness need to be measured.
(32). Roger Chou et al. Major Update: Masks for Prevention of SARS-CoV-2 in Health Care and Community Settings-Final Update of a Living, Rapid Review. Ann Intern Med. 2023
Background:
Optimal use of masks for preventing COVID-19 is unclear.
Purpose:
To update an evidence synthesis on N95, surgical, and cloth mask effectiveness in community and health care settings for preventing SARS-CoV-2 infection.
Data Sources:
MEDLINE, EMBASE, medRxiv (3 June 2022 to 2 January 2023), and reference lists.
Study Selection:
Randomized trials of interventions to increase mask use and risk for SARS-CoV-2 infection and observational studies of mask use that controlled for potential confounders.
Data Extraction:
Two investigators sequentially abstracted study data and rated quality.
Data Synthesis:
Three randomized trials and 21 observational studies were included. In community settings, mask use may be associated with a small reduced risk for SARS-CoV-2 infection versus no mask use, on the basis of 2 randomized trials and 7 observational studies. In routine patient care settings, surgical masks and N95 respirators may be associated with similar risk for SARS-CoV-2 infection, on the basis of 1 new randomized trial with some imprecision and 4 observational studies. Evidence from observational studies was insufficient to evaluate other mask comparisons due to methodological limitations and inconsistency.
Limitation:
Few randomized trials, studies had methodological limitations and some imprecision, suboptimal adherence and pragmatic aspects of randomized trials potentially attenuated benefits, very limited evidence on harms, uncertain applicability to Omicron variant predominant era, meta-analysis not done due to heterogeneity, unable to formally assess for publication bias, and restricted to English-language articles.
Conclusion:
Updated evidence suggests that masks may be associated with a small reduction in risk for SARS-CoV-2 infection in community settings. Surgical masks and N95 respirators may be associated with similar infection risk in routine patient care settings, but a beneficial effect of N95 respirators cannot be ruled out.
(33). Tara N. Palmore, et al. For Patient Safety, It Is Not Time to Take Off Masks in Health Care Settings. Ann Intern Med. 2023
As the COVID-19 public health emergency is lifted and the pandemic continues to recede, hospitals must decide how to de-escalate mitigation strategies to sustainable states. Decisions about modifying institutional strategies for infection prevention and control are complex and depend on regional and institutional factors. As health care facilities approach this crossroad, we urge their leaders to take stock of what we have learned regarding masking and patient safety.
Masking in the community has been a controversial mitigation strategy during the pandemic, in part because of the dearth of high-quality evidence documenting efficacy and in part because mask wearing has become politicized. Most published studies addressing mask efficacy have methodological flaws, and adherence to mask wearing has been suboptimal in virtually all. Demonstrating that masks work is difficult when they are not worn consistently. Although gold-standard evidence is not available, we argue that, despite the lack of clinical efficacy trials (as with the widely accepted practice of hand hygiene), masking in interactions between patients and health care personnel should continue to receive serious consideration as a patient safety measure.
Laboratory studies have done what clinical research has not and demonstrated that surgical masks-and to a greater extent, filtering facepiece respirators-are effective in limiting the spread of aerosols and droplets from individuals infected with influenza, coronaviruses, and other respiratory viruses (1). Although not 100% effective, they substantially reduce quantities of virus expelled during coughing or talking, thereby mitigating risk (2).
Real-world experience shows the effectiveness of mask wearing in clinical settings. Thanks largely to universal masking and use of other personal protective equipment, health care personnel have been at far greater risk for acquiring COVID-19 from community than occupational exposures (3). Transmission from patient to staff and staff to patient when both are masked does occur but is uncommon (4).
A compelling reason for continuing masking in health care is presenteeism, a behavior that long preceded, and will likely outlast, the pandemic. Health care personnel are notorious for coming to work while ill. In studies conducted during the pandemic, half to two thirds of health care personnel acknowledged working with symptoms of respiratory illness (5). Presenteeism has been well documented in health care-associated respiratory viral outbreaks (6), with various reasons proffered, including an unwillingness to place burdens on colleagues, a belief that some respiratory infections may be trivial, a fear of reprisal for absenteeism, a moral imperative to provide patient care, and, for those in some roles, a lack of paid sick leave. We can find no reason to believe these time-honored behaviors will change if masks come off.
In one of our hospitals, the NIH Clinical Center, we studied presenteeism in detail during the pandemic via contact tracing interviews (NIH Clinical Center. Unpublished data.). Among staff who chose an asymptomatic rather than a symptomatic testing pathway and tested positive, more than 50% subsequently acknowledged having had some symptoms characteristic of COVID-19 at the time of testing. These data underscore the problem of presenteeism and emphasize the appropriateness of masking. Despite the proximity of personnel providing care, no transmission to patients was identified.
Presymptomatic transmission of respiratory viruses, particularly SARS-CoV-2, provides additional grounds for the continued use of masking in clinical contexts (7). Those who are vaccinated against influenza or SARS-CoV-2 may present with mild symptoms that are often minimized or mistaken as noninfectious (6). In addition, up to a third of Omicron infections are asymptomatic (8)-but could nonetheless cause severe or life-threatening disease or prolonged illness if transmitted to immunologically vulnerable patients. Hospitals serving elderly and immunocompromised patients, such as oncology patients and stem-cell and organ transplant recipients, face challenges when deescalating measures that protect these patient populations.
Universal masking may not be the only valid approach. One could envision other reasonable approaches to this issue, based on the clinical setting. Examples include masking only during respiratory virus season, beginning in the fall; masking on wards housing patients at higher risk for serious sequelae of respiratory virus infections; or masking staff and visitors but allowing optional masking for patients (one-way masking). In any event, exposing patients unnecessarily to infections that are preventable by masking seems directly contrary to the principles of patient safety. For all of these reasons, we advocate remaining masked during patient interactions.
Use of masks in the clinical setting should continue to be studied for both benefits and untoward consequences. The most concrete pitfalls of masks, such as impeding communication and negatively affecting empathy, should become fodder for engineers and developers to improve or redesign masks to obviate these issues.
On balance, despite the limitations of existing masks, health care institutions functioned reasonably well during the pandemic. Some have argued that sustaining universal masking is impractical for patient care. During the early HIV/AIDS epidemic, some physicians said they simply could not-for a host of reasons-wear gloves even when situations were associated with likely exposure to blood or bloody body fluids. Health care personnel have adjusted to this requirement, and glove use in such situations has now become the standard of care and is widely accepted as part of standard precautions.
We are struck by the broad efficacy of masks for source control and protection during the pandemic and find this to be one of the major lessons learned with enduring value as a patient safety measure in health care. A striking finding was the remarkable reduction in the health care-associated transmission of virtually all respiratory viruses, not simply SARS-CoV-2, in our institutions and others. Although not all of our colleagues agree with our approach (9), a survey of hospital epidemiologists across the country suggests that, as recently as the fall and winter of 2022, about 97% of surveyed hospital epidemiologists were not eager to eliminate masks in their facilities (10). Perhaps that sentiment has shifted in the past 4 months, but the support of many infection prevention experts for using masks for broad prevention of respiratory virus transmission, and not simply SARS-CoV-2, suggests that many others share this view.
In our enthusiasm to return to the appearance and feeling of normalcy, and as institutions decide which mitigation strategies to discontinue, we strongly advocate not discarding this important lesson learned for the sake of our patients’ safety.
(34). Miriam Santer et al. Effectiveness of spironolactone for women with acne vulgaris (SAFA) in England and Wales: pragmatic, multicentre, phase 3, double blind, randomised controlled trial. BMJ 2023;381:e074349.
Objective:
To assess the effectiveness of oral spironolactone for acne vulgaris in adult women.
Design:
Pragmatic, multicentre, phase 3, double blind, randomised controlled trial.
Setting:
Primary and secondary healthcare, and advertising in the community and on social media in England and Wales.
Participants:
Women (≥18 years) with facial acne for at least six months, judged to warrant oral antibiotics.
Interventions:
Participants were randomly assigned (1:1) to either 50 mg/day spironolactone or matched placebo until week six, increasing to 100 mg/day spironolactone or placebo until week 24. Participants could continue using topical treatment.
Main outcome measures:
Primary outcome was Acne-Specific Quality of Life (Acne-QoL) symptom subscale score at week 12 (range 0-30, where higher scores reflect improved QoL). Secondary outcomes were Acne-QoL at week 24, participant self-assessed improvement; investigator’s global assessment (IGA) for treatment success; and adverse reactions.
Results:
From 5 June 2019 to 31 August 2021, 1267 women were assessed for eligibility, 410 were randomly assigned to the intervention (n=201) or control group (n=209) and 342 were included in the primary analysis (n=176 in the intervention group and n=166 in the control group). Baseline mean age was 29.2 years (standard deviation 7.2), 28 (7%) of 389 were from ethnicities other than white, with 46% mild, 40% moderate, and 13% severe acne. Mean Acne-QoL symptom scores at baseline were 13.2 (standard deviation 4.9) and at week 12 were 19.2 (6.1) for spironolactone and 12.9 (4.5) and 17.8 (5.6) for placebo (difference favouring spironolactone 1.27 (95% confidence interval 0.07 to 2.46), adjusted for baseline variables). Scores at week 24 were 21.2 (5.9) for spironolactone and 17.4 (5.8) for placebo (difference 3.45 (95% confidence interval 2.16 to 4.75), adjusted). More participants in the spironolactone group reported acne improvement than in the placebo group: no significant difference was reported at week 12 (72% v 68%, odds ratio 1.16 (95% confidence interval 0.70 to 1.91)) but significant difference was noted at week 24 (82% v 63%, 2.72 (1.50 to 4.93)). Treatment success (IGA classified) at week 12 was 31 (19%) of 168 given spironolactone and nine (6%) of 160 given placebo (5.18 (2.18 to 12.28)). Adverse reactions were slightly more common in the spironolactone group with more headaches reported (20% v 12%; p=0.02). No serious adverse reactions were reported.
Conclusions:
Spironolactone improved outcomes compared with placebo, with greater differences at week 24 than week 12. Spironolactone is a useful alternative to oral antibiotics for women with acne.
(35). Paul Sorajja, et al. Transcatheter Repair for Patients with Tricuspid Regurgitation. N Engl J Med. 2023;388:1833-1842.
Background
Severe tricuspid regurgitation is a debilitating condition that is associated with substantial morbidity and often with poor quality of life. Decreasing tricuspid regurgitation may reduce symptoms and improve clinical outcomes in patients with this disease.
Methods
We conducted a prospective randomized trial of percutaneous tricuspid transcatheter edge-to-edge repair (TEER) for severe tricuspid regurgitation. Patients with symptomatic severe tricuspid regurgitation were enrolled at 65 centers in the United States, Canada, and Europe and were randomly assigned in a 1:1 ratio to receive either TEER or medical therapy (control). The primary end point was a hierarchical composite that included death from any cause or tricuspid-valve surgery; hospitalization for heart failure; and an improvement in quality of life as measured with the Kansas City Cardiomyopathy Questionnaire (KCCQ), with an improvement defined as an increase of at least 15 points in the KCCQ score (range, 0 to 100, with higher scores indicating better quality of life) at the 1-year follow-up. The severity of tricuspid regurgitation and safety were also assessed.
Results
A total of 350 patients were enrolled; 175 were assigned to each group. The mean age of the patients was 78 years, and 54.9% were women. The results for the primary end point favored the TEER group (win ratio, 1.48; 95% confidence interval, 1.06 to 2.13; P=0.02). The incidence of death or tricuspid-valve surgery and the rate of hospitalization for heart failure did not appear to differ between the groups. The KCCQ quality-of-life score changed by a mean (±SD) of 12.3±1.8 points in the TEER group, as compared with 0.6±1.8 points in the control group (P<0.001). At 30 days, 87.0% of the patients in the TEER group and 4.8% of those in the control group had tricuspid regurgitation of no greater than moderate severity (P<0.001). TEER was found to be safe; 98.3% of the patients who underwent the procedure were free from major adverse events at 30 days.
Conclusions
Tricuspid TEER was safe for patients with severe tricuspid regurgitation, reduced the severity of tricuspid regurgitation, and was associated with an improvement in quality of life.
(36). Le Wang, et al. Single-Dose Rifapentine in Household Contacts of Patients with Leprosy. N Engl J Med. 2023;388:1843-1852.
Background
Previous studies have suggested that a single dose of rifampin has protective effects against leprosy in close contacts of patients with the disease. Rifapentine was shown to have greater bactericidal activity against Mycobacterium leprae than rifampin in murine models of leprosy, but data regarding its effectiveness in preventing leprosy are lacking.
Methods
We conducted a cluster-randomized, controlled trial to investigate whether single-dose rifapentine is effective in preventing leprosy in household contacts of patients with leprosy. The clusters (counties or districts in Southwest China) were assigned to one of three trial groups: single-dose rifapentine, single-dose rifampin, or control (no intervention). The primary outcome was the 4-year cumulative incidence of leprosy among household contacts.
Results
A total of 207 clusters comprising 7450 household contacts underwent randomization; 68 clusters (2331 household contacts) were assigned to the rifapentine group, 71 (2760) to the rifampin group, and 68 (2359) to the control group. A total of 24 new cases of leprosy occurred over the 4-year follow-up, for a cumulative incidence of 0.09% (95% confidence interval [CI], 0.02 to 0.34) with rifapentine (2 cases), 0.33% (95% CI, 0.17 to 0.63) with rifampin (9 cases), and 0.55% (95% CI, 0.32 to 0.95) with no intervention (13 cases). In an intention-to-treat analysis, the cumulative incidence in the rifapentine group was 84% lower than that in the control group (cumulative incidence ratio, 0.16; multiplicity-adjusted 95% CI, 0.03 to 0.87; P=0.02); the cumulative incidence did not differ significantly between the rifampin group and the control group (cumulative incidence ratio, 0.59; multiplicity-adjusted 95% CI, 0.22 to 1.57; P=0.23). In a per-protocol analysis, the cumulative incidence was 0.05% with rifapentine, 0.19% with rifampin, and 0.63% with no intervention. No severe adverse events were observed.
Conclusions
The incidence of leprosy among household contacts over 4 years was lower with single-dose rifapentine than with no intervention. (Funded by the Ministry of Health of China and the Chinese Academy of Medical Sciences
(37). Emmanuel C. Mrimi, et al. Emodepside for Trichuris trichiura and Hookworm Infection. N Engl J Med. 2023;388:1863-1875.
Background
Current treatments for soil-transmitted helminth infections in humans have low efficacy against Trichuris trichiura. Emodepside – a drug in veterinary use and under development for the treatment of onchocerciasis in humans – is a leading therapeutic candidate for soil-transmitted helminth infection.
Methods
Conducted two phase 2a, dose-ranging, randomized, controlled trials to evaluate the efficacy and safety of emodepside against T. trichiura and hookworm infections. We randomly assigned, in equal numbers, adults 18 to 45 years of age in whom T. trichiura or hookworm eggs had been detected in stool samples to receive emodepside, at a single oral dose of 5, 10, 15, 20, 25, or 30 mg; albendazole, at a single oral dose of 400 mg; or placebo. The primary outcome was the percentage of participants who were cured of T. trichiura or hookworm infection (the cure rate) with emodepside 14 to 21 days after treatment, determined with the use of the Kato-Katz thick-smear technique. Safety was assessed 3, 24, and 48 hours after the receipt of treatment or placebo.
Results
A total of 266 persons were enrolled in the T. trichiura trial and 176 in the hookworm trial. The predicted cure rate against T. trichiura in the 5-mg emodepside group (85% [95% confidence interval {CI}, 69 to 93]; 25 of 30 participants) was higher than the predicted cure rate in the placebo group (10% [95% CI, 3 to 26]; 3 of 31 participants) and the observed cure rate in the albendazole group (17% [95% CI, 6 to 35]; 5 of 30 participants). A dose-dependent relationship was shown in participants with hookworm: the observed cure rate was 32% (95% CI, 13 to 57; 6 of 19 participants) in the 5-mg emodepside group and 95% (95% CI, 74 to 99.9; 18 of 19 participants) in the 30-mg emodepside group; the observed cure rates were 14% (95% CI, 3 to 36; 3 of 21 participants) in the placebo group and 70% (95% CI, 46 to 88; 14 of 20 participants) in the albendazole group. In the emodepside groups, headache, blurred vision, and dizziness were the most commonly reported adverse events 3 and 24 hours after treatment; the incidence of events generally increased in a dose-dependent fashion. Most adverse events were mild in severity and were self-limited; there were few moderate and no serious adverse events.
Conclusions
Emodepside showed activity against T. trichiura and hookworm infections.
(38). Lei Wen, et al. Primary Diffuse Meningeal Melanomatosis. N Engl J Med. 2023;388:1892.
A 27-year-old woman was referred to the neuro-oncology clinic with a 3-month history of headaches, vomiting, confusion, and seizures. The physical examination was notable for meningismus without focal neurologic deficits. Magnetic resonance imaging of the head and whole spine showed diffuse leptomeningeal enhancement on T1-weighted images after administration of contrast material (Panel A, arrows). A lumbar puncture was subsequently performed, and the opening pressure was 330 mm of water (reference range, 80 to 180). Analysis of the cerebrospinal fluid showed a pleocytosis that included abundant large nonhematopoietic cells with a high nuclear-to-cytoplasmic ratio and coarse chromatin (Panel B, Wright-Giemsa stain). Tests for infection were negative. Owing to persistent symptomatic intracranial hypertension, the patient was taken urgently for placement of an external ventricular drain. During the procedure, blackened meninges were seen after the dura mater was opened (Panel C). A biopsy sample of the meninges was consistent with melanoma. No other sites of melanoma were identified on a detailed skin examination, ophthalmologic examination, or whole-body positron-emission tomography-computed tomography. A diagnosis of primary diffuse meningeal melanomatosis – a rare form of primary central nervous system melanoma – was made. Testing for BRAF V600 mutations was negative. Treatment with immunotherapy was initiated, but the patient died 7 months after the diagnosis was made.
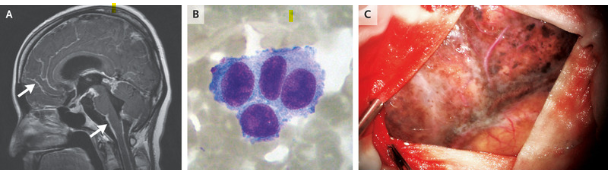
(39). Tal Goldberger et al. Miliaria Crystallina. N Engl J Med. 2023;388(20):e68.
A 55-year-old man who had been admitted to the intensive care unit had a sudden-onset vesicular rash appear across his trunk and arms. Seventeen days earlier, the patient had undergone explorative laparotomy and small-bowel resection to treat small-bowel obstruction. His postoperative course had been complicated by sepsis, respiratory failure, and fevers. On physical examination, the patient was intubated and wrapped tightly in blankets. Clear vesicles resembling water droplets were seen across his chest and upper arms (Panels A and B, respectively). The vesicles did not rupture with light palpation (see video) but broke when more pressure was applied. There was no erythema or umbilication of the lesions. After 24 hours, the rash abated without intervention. A clinical diagnosis of miliaria crystallina was made. A recommendation was given to avoid tight blankets in order to minimize sweating and skin irritation. Miliaria crystallina is a benign, self-resolving skin condition that results from superficial obstruction of sweat ducts in the stratum corneum. It is most commonly seen in neonates but is also observed in adults exposed to high heat and humidity, such as in febrile illnesses or tropical environments. Early recognition of the condition may help avoid unnecessary skin biopsies and empirical treatments in critically ill patients.
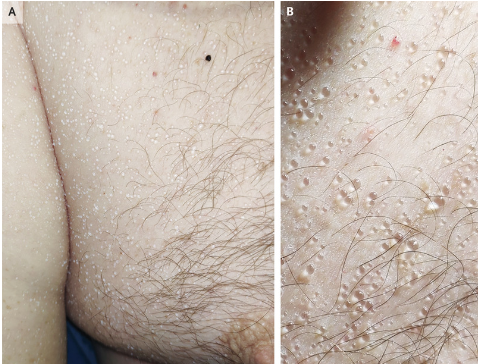
(40). Early detection of prostate cancer create overdiagnosis and inequity with minimal benefit. BMJ 2023;381:e071082.
Screening for prostate cancer with prostate-specific antigen (PSA) remains highly controversial because it is unclear whether the benefits of reduced prostate cancer mortality offset the harms of overdiagnosis and overtreatment. Given this uncertainty, most high income countries have chosen not to implement a national programme of prostate cancer screening, but allow men to obtain a PSA test after a conversation with their physician.
Informed choice approaches lead to high rates of unsystematic PSA testing, especially among those least likely to benefit and most likely to be harmed.
Countries that have adopted screening policies based on shared decision making have seen high rates of PSA testing, particularly among men 70 years or older, who are particularly prone to overdiagnosis1 but do not benefit from screening
We argue that high income countries should either implement a comprehensive risk based approach to PSA testing, one that is designed to reduce overdiagnosis and overtreatment, or discourage PSA testing through a clear recommendation against screening, along with policies that make it hard to obtain a test without defined urological indications.
(41). Marta Karbowiak et al. Management of lateral epicondylitis (tennis elbow). BMJ 2023;381:e072574.
What you need to know
Symptoms of lateral epicondylitis usually resolve within one year with activity modification and watchful waiting
Current evidence suggests that steroid injections do not offer long term benefit
Secondary care management may include percutaneous needle fenestration or injections of autologous blood or platelet rich plasma; however, evidence of moderate certainty shows no benefit from these treatments
Surgical management in refractory cases usually involves open or arthroscopic release of the affected muscle tendon
Lateral epicondylitis (also known as tennis elbow) is a common, often debilitating disorder frequently encountered in primary care across low and high resource settings.12 This article outlines current management strategies, including supportive measures, activity modification, and newer treatments that have emerged over the past 20 years, such as percutaneous needle fenestration and injection of autologous blood and platelet rich plasma.
What is lateral epicondylitis?
Lateral epicondylitis is a type of tendinosis, a degenerative process where repetitive stress causes fibroblast deposition with collagen disorganisation and vascular hyperplasia.3 Pain causes underuse of the affected arm and further weakening in the tendon structure, with possible sequelae of partial or complete rupture of the tendon.4 Cadaveric and electromyographic studies show that symptoms (namely, lateral elbow pain) are often related to excessive loading of the lateral extensor tendons, as well as repetitive wrist extension or supination movements.5 The condition commonly presents as a work related strain injury, and often affects tennis players6 (box 1).
(42). Maí«l Richard. Myocardial calcification: a rare consequence of streptococcal toxic shock. Lancet. 2023;401(10389):1691.
Life can suddenly get very complicated.
Would we expect this kind of evolution to a A 51-year-old woman presented to an emergency room with a 4-day history of fever, chills, abdominal pain, vomiting, and diarrhoea?
A 51-year-old woman presented to our emergency room with a 4-day history of fever, chills, abdominal pain, vomiting, and diarrhoea.
1 week before these problems began, the patient had a nevus removed from her right arm. The dermatologists were concerned it may have been a melanoma; she had a history of primary biliary cholangitis treated with ursodeoxycholic acid.
On examination, we found the patient to be unwell but responsive; her blood pressure was 85/59 mm Hg, her pulse was 107 beats per min, temperature was 39.0degC, respiratory rate 27 breaths per min, and oxygen saturation was 94%.
A CT scan of the patient’s chest showed air space opacities with air bronchogram indicating a pneumonia in the left and right lower lobes (figure); a CT of the abdomen showed circumferential wall thickening of the right colon and surrounding fat stranding, indicating colitis. Blood cultures grew Streptococcus pyogenes.
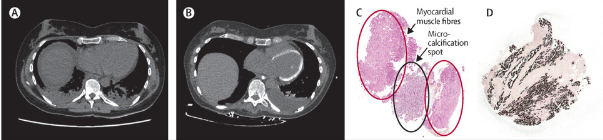
10 h after admission, the patient’s condition deteriorated and she developed septic shock; she was given intravenous antibiotics, crystalloid fluid, and norepinephrine, and transferred to the intensive care unit (ICU). 24 h after admission, she went into cardiogenic shock with a decreased left ventricular ejection fraction (LVEF) of 25% with hypokinesis of the basal and midventricular segments-typical of an inverted takotsubo cardiomyopathy (appendix); on admission her LVEF had been 50%.
Troponin blood concentration was 104 819 ng/L (normal <74). Coronary angiography showed no abnormalities. We made a diagnosis of septic cardiomyopathy, and the patient was treated with dobutamine. After some initial improvement her condition worsened and she was readmitted to the ICU because of pulmonary oedema and a persistent fever (temperature was 38.8degC): LVEF was still decreased at 25%. A whole-body CT scan showed diffuse myocardial calcifications of the left ventricle (figure) but no focus of secondary pulmonary or abdominal infection.
Histopathological examination of a sample obtained at endomyocardial biopsy confirmed myocardial calcifications (figure). Considering the findings in the round, we made a diagnosis of diffuse myocardial calcifications following severe streptococcal sepsis, and high-dose-2 mg/kg-corticosteroids were started. The fever abated and the patient’s clinical status improved; she was allowed home 3 months after admission. Corticosteroids were decreased and stopped at 3 months and the patient was treated with dapagliflozin, ramipril, and a cardioverter-defibrillator was implanted. 10 months after initial presentation, she was asymptomatic and her LVEF was 40%; the microcalcifications were still present (appendix).
Diffuse myocardial calcifications following severe sepsis are uncommon and associated with a poor prognosis. High-dose pulses of corticosteroids are recommended but evidence for effectiveness remains weak in the absence of prospective clinical trials

