Journal scan: A review of 44 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Lorenzo DAntiga, et al. Gene Therapy in Patients with the Crigler-Najjar Syndrome. N Engl J Med 2023;389:620-631.
Background
Patients with the Crigler-Najjar syndrome lack the enzyme uridine diphosphoglucuronate glucuronosyltransferase 1A1 (UGT1A1), the absence of which leads to severe unconjugated hyperbilirubinemia that can cause irreversible neurologic injury and death. Prolonged, daily phototherapy partially controls the jaundice, but the only definitive cure is liver transplantation.
Methods
We report the results of the dose-escalation portion of a phase 1-2 study evaluating the safety and efficacy of a single intravenous infusion of an adeno-associated virus serotype 8 vector encoding UGT1A1 in patients with the Crigler-Najjar syndrome that was being treated with phototherapy. Five patients received a single infusion of the gene construct (GNT0003): two received 21012 vector genomes (vg) per kilogram of body weight, and three received 51012 vg per kilogram. The primary end points were measures of safety and efficacy; efficacy was defined as a serum bilirubin level of 300 mol per liter or lower measured at 17 weeks, 1 week after discontinuation of phototherapy.
Results
No serious adverse events were reported. The most common adverse events were headache and alterations in liver-enzyme levels. Alanine aminotransferase increased to levels above the upper limit of the normal range in four patients, a finding potentially related to an immune response against the infused vector; these patients were treated with a course of glucocorticoids. By week 16, serum bilirubin levels in patients who received the lower dose of GNT0003 exceeded 300 mol per liter. The patients who received the higher dose had bilirubin levels below 300 mol per liter in the absence of phototherapy at the end of follow-up (mean [SD] baseline bilirubin level, 35156 mol per liter; mean level at the final follow-up visit [week 78 in two patients and week 80 in the other], 14933 mol per liter).
Conclusions
No serious adverse events were reported in patients treated with the gene-therapy vector GNT0003 in this small study. Patients who received the higher dose had a decrease in bilirubin levels and were not receiving phototherapy at least 78 weeks after vector administration. (Funded by Genethon and others;
(2). Preventing HIVs Collateral Cardiovascular Damage. N Engl J Med 2023;389:e11.
People living with HIV have increased risk for cardiovascular disease (and other diseases of aging) earlier in life than those without HIV. In this episode of Intention to Treat, researcher Steven Grinspoon describes a new strategy for preventing collateral damage.
Rachel Gotbaum: Welcome to Intention to Treat from the New England Journal of Medicine. Im Rachel Gotbaum.
Today, were going to talk about patients living with HIV long term and why theyre more likely to develop the diseases of aging faster, specifically cardiovascular disease.
Alicia Diggs: I honestly didnt put it together that because Im living with HIV, Im at greater risk for other comorbidities, that I was twice as likely to develop heart disease because of HIV.
Steven Grinspoon: People living with HIV have cardiovascular disease, even when theyre young. And that cardiovascular disease can be prevented.
Rachel Gotbaum: Today on Intention to Treat, a new strategy that will help millions of patients living with HIV avoid death from heart disease.
Rob Quinn: My name is Rob Quinn. Im 63 years old. I was diagnosed HIV-positive in 1993 at the age of 34. So, God willing, this November will be 30 years Ive been living with HIV/AIDS. I was diagnosed in 1993, so that was before the advent of protease inhibitors and other medications. So for 2 years, I was really just taking some vitamins. And then of course, medications came along in 95. I was doing very well, but then I remember being at the beach and I felt like a bump on the back of my head, and I looked and it just looked like a little black and blue. It was Kaposis sarcoma, which, as you know, is a skin cancer as a result of HIV/AIDS, and now I had a diagnosis of AIDS.
I was diagnosed with AIDS, and shortly after, I remember I was home and my heart started racing and I started to feel really like I just was going to fall. Sure enough, I had my first heart attack in 1999. I was 39, so not even 40. At that time, I remember going to my provider, sharing with him that I was having chest pain, I had these symptoms, I had the heart attack. And he felt that there was no correlation, nothing tying it to the HIV. Things seemed OK on paper, but we never brought it up again.
Then in 2012, I had a second heart attack. And I had been telling providers that there was something wrong. There was something wrong. And they would do these blood-pressure tests and these really simple tests, and everythings coming back normal. I spoke to my primary care provider, and I think he just to please me ordered an echocardiogram. Because he did my blood pressure, my blood pressure was fine. Did some routine lab work, my routine lab work was fine. But Im like, Somethings not fine. He said, Well, we could do a cardiac catheterization and see if theres any blockages. And sure enough, I did have blockages. And as a result, I now have two stents and a defibrillator. But if it wasnt for me pushing them, I probably would be six feet under, because on paper, things were coming back in normal range.
I was living in Springfield, and there were no cardiologists that had HIV experience. So I decided, Well, let me move back to Boston. I ended up at Massachusetts General Hospital with an amazing cardiologist, and he did a whole battery of tests, and then he ordered an echocardiogram, which showed that my ejection fraction was at 35. So my heart wasnt pumping the blood out fast enough, which means it was backing up, so that could have led to stroke and other things, so it had to be corrected.
I ended up having to have the defibrillator implanted because I went into AFib so fast, my heart rate went so fast, that they were very concerned. HIV is the easy part now its all the aging stuff thats coming up, but we hit those markers earlier than people who are not living with HIV. Were classified as the silver generation, because were really the first generation of long-term survivors. So a lot of this is new to everybody. Its new to the patients, its new to the providers. So we have to take a step back every now and then just realize were all learning this together.
When I first started taking HIV meds, I was taking upwards of 40 pills. And its funny, now I take a single tablet of HIV med, but I have seven medications for my heart. Thank God that I got the care that I needed and I deserve, and is allowing me to thrive.
Alicia Diggs: My name is Alicia Diggs. I am 51 years young, and I was diagnosed at the age of 29, which was in 2001. I actually contracted HIV from my now ex-husband who failed to disclose to me after I asked had he been diagnosed or had he been tested. This person who I thought I knew was actually living with an AIDS diagnosis at the time and kept that information from me.
So, when I was diagnosed, there was no treatment for me because I was considered at a normal range. Nowadays, its get into care, get on meds. That was not the thing back in the early 2000s. It was as long as your CD4 levels were at a certain point, there was no treatment you needed to get in. For 10 years, I was considered a nonprogressor. But by the time that 10th year came, my CD4 numbers started to drop. Those numbers continued to drop every time I went to the doctor, so I asked for a medication. I was the one who asked, What treatments are available for me that would allow me to work full-time, go to school full-time, and take care of my children without being sick? Then I was introduced to medication.
I had been doing absolutely great, and my CD4 levels are through the roof, meaning theyre over 1000. Now, theres not been any heart issues, any lung issues, anything like that. So as far as my organs and everything are concerned, Im thankful that, for me, I have not experienced those, but Im aware of it because I do know many peers who have experienced HIV for a long time and aging through HIV. They are dealing with heart issues, so heart disease. Theyre also dealing with kidney issues, kidney disease, sight issues, cognitive issues.
I have heard that people living with HIV age faster. So, yes, as a person living with HIV, though I am in my 50s, sometimes my body feels as if Im in my 60s. And there is a concern as a person taking medication and living as long as I have lived with HIV, the long-term effects. So Im trying to do everything that I can to prevent any long-term effects, or to at least combat them before it happens.
For me, I am learning to see this from a different lens, see aging and HIV from a different lens, because this virus has affected our immune system and our organs for so many years, its a battlefield on the inside. I honestly didnt put it together that because Im living with HIV, Im at greater risk for other comorbidities, that I was twice as likely to develop heart disease because of HIV. Why its not talked about, Im not sure. And it should be talked about, so that people understand the true severity of what HIV does to the body. If you just look past all of that, then youre doing an injustice. So now that Im seeing it from a different lens, Im not just saying, OK, well, Im just aging. So Im trying to do everything that I can to prevent any long-term effects, or to at least combat them before it happens.
Rachel Gotbaum: This is Intention to Treat from the New England Journal of Medicine. Im Rachel Gotbaum. There are millions of people worldwide living with HIV. Their virus can be controlled with effective antiretroviral therapies, but fighting the virus is taking a toll on their bodies, and these patients are more likely to develop heart disease and other diseases of aging early. Were joined now by Dr. Steven Grinspoon. Hes chief of the Metabolism Unit at Massachusetts General Hospital. Dr. Grinspoon led a global study that helped prevent heart disease in thousands of HIV patients.
Dr. Grinspoon, lets first talk about what is the status of HIV patients and heart disease and some of these other diseases from inflammation?
Steven Grinspoon: People living with HIV are doing much better now, of course, because of the efficacy of long-term, effective antiretroviral therapy. What we see now is a closing mortality gap people with HIV are living longer but there is a persistent comorbidity gap, including specifically cardiovascular disease. Cardiovascular disease is increased twofold among patients living with HIV compared to other populations without HIV, in which its decreasing. And we also know that people living with HIV have significantly increased inflammation. And we and others have shown that the surface of the arterial system is inflamed among people living with HIV.
So, the current antiretroviral therapy is effective at keeping the virus in check, but there is still a little bit of virus living in the macrophages, hunkered down in there. And the innate immune system is turned on to try and fight that chronically. This is a good thing in general, because the body is effectively trying to fight the virus along with the antiretroviral therapy, but there may be collateral damage from this persistent immune activation, including to other organ systems, such as the cardiovascular system.
Rachel Gotbaum: So Dr. Grinspoon, can you explain how these patients are different and how theyre more likely to have diseases of aging earlier and what that looks like?
Steven Grinspoon: People living with HIV do have indices of premature aging, and we think thats also related to this persistent immune activation and inflammation. For example, people living with HIV have coronary artery disease plaque at a level thats seen in patients 10 years older, and thats a prime example of this premature aging phenomena. In addition, patients living with HIV often show frailty, chronic kidney disease, some problems with cognition. So the focus of our research has been specifically on the cardiovascular system, and we have shown that it is inflamed, and that 50% of people with HIV age 50 have coronary plaque.
And particularly, its shocking because the predicted risk in that group was only 5%. So those patients in that study, they were young, age 50, and despite that, half of them had coronary plaque. Thats something you would not expect, not in a 50-year-old. Now in addition, there are certain features of plaque which make them vulnerable, vulnerable to rupture. And when it ruptures, you have a heart attack. The features of vulnerability of plaque include noncalcification, soft plaque, and those features were seen in 23% of the patients in the study Im referring to significant evidence of premature aging in that population.
Rachel Gotbaum: Lets talk about your hunch, because this all came from your research over the years. So ,tell me what your hunch was and what brought us to this study, and how this study worked?
Steven Grinspoon: Our hunch was if we enrolled a group of relatively young patients living with HIV, theyd be inflamed, theyd have cardiovascular risks, but they wouldnt be showing that cardiovascular risk by traditional risk scores. So our hunch was we could come up with a strategy to prevent that disease in that population. And thats a pretty out-there hypothesis, because most doctors would not treat young patients without traditional risk factors. They just dont fall into the typical algorithms of treatment. So we really pushed the boundary by enrolling this population that no one would seem to treat but we knew, based on our data, would have significant cardiovascular disease.
So, what did we do? We picked a statin strategy. And you might say, Statins, well, those drugs are used to lower cholesterol. People know that they work to lower cholesterol, but what people dont realize so much about statins is that they also have significant anti-inflammatory effects. So our hypothesis was that we could get a two-for-one strategy. In other words, we could give patients a statin, which would work to lower cholesterol. Thats not a bad thing, and that does help with cardiovascular disease. Its important, very important. But at the same time, this drug would be lowering inflammation and residual immune activation, and it was our hope that that package would prevent cardiovascular disease in this population. Because in the study that we conducted, we only enroll people who never had a history of heart disease. That doesnt mean that they didnt have plaque at baseline, subclinical plaque. In fact, we showed that they did, but they didnt have clinical manifestations, so they were ticking time bombs. We enrolled that population that was a ticking-time-bomb population. And in fact we were able to show, over 5 years of follow-up, a 35% reduction in the rates of cardiovascular disease in the treatment group compared to placebo. And our data and safety monitoring board met in late March of this year and actually stopped the study prematurely because the signal of efficacy was so robust and strong. And they also found that there were no unexpected or unanticipated adverse events.
Rachel Gotbaum: This trial was hugely ambitious. Tell us more about that.
Steven Grinspoon: There are approximately 38 to 39 million people living with HIV today. The great majority is in sub-Saharan Africa and other places, though there are substantial numbers in North America. Yet most studies focus on people living in North America and other higher-income regions. We purposely set out to broaden the net and enroll participants across the globe, in high-income and low-income regions. Sub-Saharan Africa, the Caribbean, Haiti, South America, Thailand, India, and other places as well. So our results are absolutely generalizable to all the populations across those regions.
Importantly, a large percentage of people living with HIV are women. Thirty-one percent of the trial population were female. Also, only 35% of the participants were White, which means 65% were non-White. So our study population is reflective of that diversity across the globe. But to do a prevention trial, its much harder than doing a treatment trial. We pick people specifically excluding anyone who had known clinical cardiovascular disease. And you have to enroll a very large number of patients into a trial to be able to show a clinically relevant reduction in heart disease. And in fact we enrolled 7769 participants, which was a very large number and very ambitious indeed, in 12 countries.
Rachel Gotbaum: Theres been this theory that the antiretroviral therapies are contributing to this problem, the cardiovascular and other diseases of aging early on that we are seeing among HIV patients. What does your research and this study and other research tell us?
Steven Grinspoon: Theres been an evolution in thought of whats contributing to the excess cardiovascular risk in people living with HIV. In the beginning, much was attributed to antiretroviral therapy and its effects. The earlier drugs led to changes in body fat with increasing fat in the abdominal area, or belly fat, and loss of fat in the subcutaneous areas, particularly in the face. In addition, some of these therapies led to insulin resistance and outright diabetes. The more current antiretroviral therapies do not lead to these significant side effects and complications.
Another piece of the puzzle is the fact that initially people thought, Oh, these antiretroviral therapies are toxic enough that we should actually be delaying their initiation to avoid toxicity in them. But in fact, interestingly, the opposite was shown that initiation and a more aggressive use of antiretroviral therapy led to fewer comorbidities in addition to less AIDS-specific diseases. Well, thats because earlier use just shut the virus down. But what weve learned subsequently, in antiretroviral therapy knowledge 2.0, is that shutting it down doesnt shut it down entirely. Theres still this low-grade inflammation that persists. The therapies are excellent, they are necessary, they are lifesaving, but they are not good enough to prevent this low-grade inflammation.
Thats where our hunch came in, that if we added an anti-inflammatory strategy that was safe on top of the antiretroviral therapy, we would have patients who could more effectively control these comorbidities, specifically cardiovascular disease in our case. We certainly showed there was a reduction in major adverse cardiovascular events, heart attacks and strokes. There are other anti-inflammatory strategies. The problem with some of the anti-inflammatory strategies is that if you tweak the system too much and you lower that innate immune function, you may actually increase the risk of infection too much.
So, you have to thread the needle. You have to come up with a strategy that effectively lowers it, a low level of inflammation, but also doesnt do it to such a degree that it unleashes the virus and causes the primary infection to rear its head again and cause a problem. We dont want that to happen. So its a very interesting task of threading the needle here and finding the right strategy.
Now going forward, we could try other therapies if we want, or I think more likely, we should recommend statin therapy, at least, for patients with low-to-moderate disease living with HIV who would not ordinarily be recommended that. Current guidelines do recommend that physicians discuss with their patients if they have HIV that that could potentially increase the risk of cardiovascular disease. Yet statin prescribing was still very low among people living with HIV, despite the fact that that was noted as a risk enhancer.
Rachel Gotbaum: If in fact we knew HIV patients were twice as likely to get cardiovascular disease, we knew that, and there were recommendations that the statins were prescribed, why were they not? What happened here?
Steven Grinspoon: Right now, the traditional risk algorithms that people use to put people on a statin dont typically measure inflammatory pathways, in the case of HIV dont measure any HIV-specific scoring. We have an important opportunity to actually use the REPRIEVE data to develop our own scoring system, to perhaps come up with a new risk-prediction algorithm thats more specific and accurate in people living with HIV. We have not done that yet. It is a hope of ours to be able to do that, and I think we have the data to do that.
Rachel Gotbaum: How does this change how we are going to be looking at HIV, looking at inflammation, these risk factors, and how were going to be caring for possibly millions of patients? I mean, how do you see this moving forward now?
Steven Grinspoon: I think this is a game changer, because weve got the virus pretty much under control with the use of effective antiretroviral therapy, but the problem thats emerged is people living with HIV are now living with a chronic disease. It happens to be a chronic inflammatory disease. So theyre living with this chronic inflammatory disease, yet theres been no focus on that. The only focus has been to get the virus in check which is great, but its not enough. Its critical, but not sufficient.
This is the first global study to try to prevent a condition thats associated with HIV, which is, surprisingly, cardiovascular disease. Weve known its a risk enhancer, weve kind of ignored that. Weve known that there are strategies, weve kind of ignored that. REPRIEVE has, I hope, woken people up to the fact that people living with HIV have cardiovascular disease, even when theyre young. And that cardiovascular disease can be prevented, and its a chronic condition that needs to be treated. We need to pay attention to it. We need to pay attention to other conditions as well that are associated with living with HIV chronically.
Rachel Gotbaum: Thank you so much, Dr. Grinspoon.
Steven Grinspoon: Thank you, Rachel. I really appreciate it. Its been a wonderful discussion.
Rachel Gotbaum: Dr. Steven Grinspoon is chief of the Metabolism Unit at Massachusetts General Hospital.
This is Intention to Treat from the New England Journal of Medicine.
(3). Hiroko Fukushima et al. Cold Agglutinin Syndrome. N Engl J Med. 2023;389:642.
A 3-year-old girl presented to the emergency department with a 1-day history of dark urine and jaundice after the development of an upper respiratory tract infection 1 week earlier. The physical examination was notable for pharyngeal erythema and exudates, conjunctival pallor, and scleral icterus. There was no hepatosplenomegaly, rash, or acrocyanosis. Laboratory studies showed a new anemia and findings consistent with hemolysis
A subsequent peripheral-blood smear (Panel A) showed varied sizes and shapes of red cells that included reticulocytes (arrows) and spherocytes (arrrowheads), as well as erythrocyte agglutination (asterisks). Many neutrophils were coated with agglutinated erythrocytes, forming rosettes (Panel B). Phagocytosis of erythrocytes in macrophages (Panel C) and neutrophils (Panel D) was also seen rare findings in autoimmune hemolytic anemia.
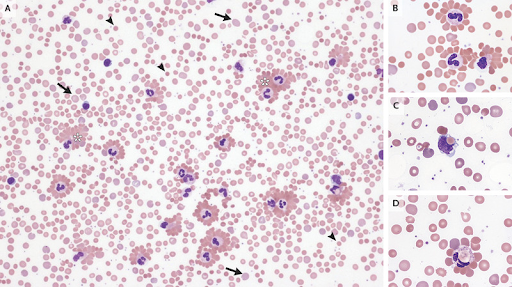
A direct antiglobulin test was positive for C3d and weakly positive for IgG. The cold agglutinin titer was 1:1024. Tests for Mycoplasma pneumoniae, Epstein-Barr virus, and other common respiratory viruses were negative. A diagnosis of autoimmune hemolytic anemia from cold agglutinin syndrome associated with an upper respiratory infection was made. Supportive care, including blood transfusions and cold avoidance, was provided. At the 3-week follow-up, the child felt well and the anemia had abated.
(4). Daan Rauwerdink et al. Burrow Ink Test for Scabies. N Engl J Med 2023;389:e12.

A 20-year-old man presented to the dermatology clinic with a 3-month history of generalized itchiness. A sexual partner of the patient had similar pruritus. On physical examination, multiple erythematous papules were seen on the trunk, in the genital area, and on the flexor aspects of the wrists (Panel A). There were no visible skin burrows. However, when a papule on the wrist was covered with a purple skin marker (Panel B) and then wiped with an alcohol swab, an ink-filled skin burrow became visible (Panel C). On the basis of this positive burrow ink test, a diagnosis of scabies was made. Scabies is a pruritic skin infestation caused by Sarcoptes scabiei var. hominis, the only mite known to burrow into the stratum corneum. The burrow ink test is a simple, rapid, and inexpensive method to visualize the pathognomonic burrows. A negative test does not rule out scabies, however, and further testing with dermoscopy or microscopic examination of skin scrapings is necessary. Treatment with both ivermectin and topical permethrin was given owing to the severity of the patients symptoms. The patients close contacts were also notified of the diagnosis and treated. Four weeks after the initial presentation, the patients symptoms had completely abated.
(5). Raymond Hang Wun Li et al. Oral emergency contraception with levonorgestrel plus piroxicam: a randomised double-blind placebo-controlled trial. Lancet, 2023.
Background
Levonorgestrel, a standard drug for emergency contraception (EC), is not effective if administered post-ovulation. A cyclo-oxygenase inhibitor could contribute synergistic effects. We investigated whether a single 40 mg oral dose of piroxicam as co-treatment with levonorgestrel improved emergency contraceptive efficacy.
Methods
This was a randomised double-blind placebo-controlled trial carried out in a major community sexual and reproductive health service in Hong Kong. Women who required levonorgestrel EC within 72 h of unprotected sexual intercourse were recruited and block-randomised in a 1:1 ratio to receive a single supervised dose of levonorgestrel 1.5 mg plus either piroxicam 40 mg or placebo orally. Group assignment was concealed in opaque envelopes and masked to the women, clinicians, and investigators. At follow-up 1-2 weeks after the next expected period, the pregnancy status was noted by history or pregnancy test. The primary efficacy outcome was the proportion of pregnancies prevented out of those expected based on an established model. All women randomised to receive the study drug and who completed the follow-up were analysed. The trial was registered with ClinicalTrials.gov, NCT03614494.
Findings
860 women (430 in each group) were recruited between Aug 20, 2018, and Aug 30, 2022. One (0.2%) of 418 efficacy-eligible women in the piroxicam group were pregnant, compared with seven (1.7%) of 418 in the placebo group (odds ratio 0.20 [95% CI 0.02-0.91]; p=0.036). Levonorgestrel plus piroxicam prevented 94.7% of expected pregnancies compared with 63.4% for levonorgestrel plus placebo. We noted no significant difference between the two groups in the proportion of women with advancement or delay of their next period, or in the adverse event profile.
Interpretation
Oral piroxicam 40 mg co-administered with levonorgestrel improved efficacy of EC in our study. Piroxicam co-administration could be considered clinically where levonorgestrel EC is the option of choice.
(6). Pulmonary Hypertension, 2023
The field of pulmonary hypertension has been transformed by advances in understanding of pathophysiological mechanisms and the development of a wide range of therapeutic options.
The five main groups of pulmonary hypertension differ in epidemiology, causes and risk factors, underlying disease mechanisms, and clinical presentation. Approaches to diagnosis and management reflect the distinctive features of each condition.
In the first of a Series of three papers, Marc Humbert and colleagues provide an overview of the pathophysiology of pulmonary arterial hypertension, current therapeutic approaches, and emerging treatment options, with a forward-looking discussion of innovative solutions for future clinical trials.
Karen Olsson and colleagues consider the pathomechanisms of pulmonary hypertension associated with lung disease, outline approaches to diagnosis and management, and emphasise the need for safe, effective treatment options and non-invasive diagnostic tools to detect and characterise pulmonary hypertension in this patient population.
Finally, Marion Delcroix and colleagues review the anatomy and pathophysiology of chronic thromboembolic pulmonary tension, describe surgical, interventional, and medical therapeutic options, and outline approaches to multimodal management.
Marc Humbert et al. Treatment of pulmonary arterial hypertension: recent progress and a look to the future
Pulmonary arterial hypertension (PAH) is a severe but treatable form of pre-capillary pulmonary hypertension caused by pulmonary vascular remodelling. As a result of basic science discoveries, randomised controlled trials, studies of real-world data, and the development of clinical practice guidelines, considerable progress has been made in the treatment options and outcomes for patients with PAH, underscoring the importance of seamless translation of information from bench to bedside and, ultimately, to patients.
However, PAH still carries a high mortality rate, which emphasises the urgent need for transformative innovations in the field.
In this Series paper, written by a group of clinicians, researchers, and a patient with PAH, we review therapeutic approaches and treatment options for PAH. We summarise current knowledge of the cellular and molecular mechanisms of PAH, with an emphasis on emerging treatable pathways and optimisation of current management strategies. In considering future directions for the field, our ambition is to identify therapies with the potential to stall or reverse pulmonary vascular remodelling. We highlight novel therapeutic approaches, the important role of patients as partners in research, and innovative approaches to PAH clinical trials.
Karen M Olsson. Pulmonary hypertension associated with lung disease: new insights into pathomechanisms, diagnosis, and management.
Patients with chronic lung diseases, particularly interstitial lung disease and chronic obstructive pulmonary disease, frequently develop pulmonary hypertension, which results in clinical deterioration, worsening of oxygen uptake, and an increased mortality risk. Pulmonary hypertension can develop and progress independently from the underlying lung disease. The pulmonary vasculopathy is distinct from that of other forms of pulmonary hypertension, with vascular ablation due to loss of small pulmonary vessels being a key feature. Long-term tobacco exposure might contribute to this type of pulmonary vascular remodelling. The distinct pathomechanisms together with the underlying lung disease might explain why treatment options for this condition remain scarce. Most drugs approved for pulmonary arterial hypertension have shown no or sometimes harmful effects in pulmonary hypertension associated with lung disease. An exception is inhaled treprostinil, which improves exercise capacity in patients with interstitial lung disease and pulmonary hypertension. There is a pressing need for safe, effective treatment options and for reliable, non-invasive diagnostic tools to detect and characterise pulmonary hypertension in patients with chronic lung disease.
Marion Delcroix et al. Chronic thromboembolic pulmonary hypertension: realising the potential of multimodal management.
Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare complication of acute pulmonary embolism. Important advances have enabled better understanding, characterisation, and treatment of this condition. Guidelines recommending systematic follow-up after acute pulmonary embolism, and the insight that CTEPH can mimic acute pulmonary embolism on initial presentation, have led to the definition of CTEPH imaging characteristics, the introduction of artificial intelligence diagnosis pathways, and thus the prospect of easier and earlier CTEPH diagnosis. In this Series paper, we show how the understanding of CTEPH as a sequela of inflammatory thrombosis has driven successful multidisciplinary management that integrates surgical, interventional, and medical treatments. We provide imaging examples of classical major vessel targets, describe microvascular targets, define available tools, and depict an algorithm facilitating the initial treatment strategy in people with newly diagnosed CTEPH based on a multidisciplinary team discussion at a CTEPH centre. Further work is needed to optimise the use and combination of multimodal therapeutic options in CTEPH to improve long-term outcomes for patients.
Joseph Newman et al. Illuminating the many faces of pulmonary hypertension
The field of pulmonary hypertension has been transformed beyond recognition over the past 30 years. Advances in the understanding of pathophysiology has led to the testing of multiple therapies and interventions in clinical trials. This productive bench-to-bedside pipeline, from basic mechanisms through to evidence-based clinical guidelines, is something to be celebrated. Here, we reflect on a Series of three important translational reviews, published in The Lancet Respiratory Medicine, that acknowledge recent advances and look ahead to new challenges and opportunities.
(7). Catherine Le Berre et al. Ulcerative colitis. 2023
Ulcerative colitis is a lifelong inflammatory disease affecting the rectum and colon to a variable extent. In 2023, the prevalence of ulcerative colitis was estimated to be 5 million cases around the world, and the incidence is increasing worldwide. Ulcerative colitis is thought to occur in people with a genetic predisposition following environmental exposures; gut epithelial barrier defects, the microbiota, and a dysregulated immune response are strongly implicated. Patients usually present with bloody diarrhoea, and the diagnosis is based on a combination of clinical, biological, endoscopic, and histological findings. The aim of medical management is, first, to induce a rapid clinical response and normalise biomarkers and, second, to maintain clinical remission and reach endoscopic normalisation to prevent long-term disability. Treatments for inducing remission include 5-aminosalicylic acid drugs and corticosteroids. Maintenance treatments include 5-aminosalicylic acid drugs, thiopurines, biologics (eg, anti-cytokines and anti-integrins), and small molecules (Janus kinase inhibitors and sphingosine-1-phosphate receptor modulators). Although the therapeutic options are expanding, 10-20% of patients still require proctocolectomy for medically refractory disease. The keys to breaking through this therapeutic ceiling might be the combination of therapeutics with precision and personalised medicine.
(8). Michael Tran et al. Venous eczema and chronic venous disease. BMJ 2023;382:e074602
What we need to know
Comprehensive assessment of venous eczema includes asking about triggers, time course of symptoms, discomfort or pain, complications, and quality of life
Effective management is multifaceted, and requires patient engagement and concurrent treatment of contributing lifestyle factors
Frameworks such as the revised venous clinical severity score can help categorise and monitor the burden of disease and guide management
What we should cover
History
Venous eczema is a common inflammatory dermatosis of the lower extremities, occurring in patients with chronic venous disease.1 It occurs secondary to chronic inflammation, which arises from venous hypertension and a failure of the venous pump, obstructed venous flow, and dysfunctional venous valves, with reflux of blood from deep into now high pressure superficial venous systems (fig 1).1 Symptoms of venous eczema vary according to chronicity. Initial presentation can be highly variable and overlap with symptoms of chronic venous disease, including lower extremity heaviness, aching, swelling, itching, and discomfort.2 Exclude differential diagnoses (box 1).
Differential diagnoses of venous eczema
Common
Cellulitis
Irritant or allergic contact dermatitis
Asteatotic eczema (eczema craquele)
Lichen simplex chronicus
Psoriasis
Dermatophyte infection (tinea corporis)
Actinically damaged skin (sun damage)
Autosensitisation dermatitis (secondary dermatitis that has developed at a location distant from the primary inflammatory focus)
Less common
Skin cancer
(9). Prof Anurag Bhargava et al. Nutritional supplementation to prevent tuberculosis incidence in household contacts of patients with pulmonary tuberculosis in India (RATIONS): a field-based, open-label, cluster-randomised, controlled trial. Lancet 2023;402(10402):P627-640.
In India, tuberculosis and undernutrition are syndemics with a high burden of tuberculosis coexisting with a high burden of undernutrition in patients and in the population. The aim of this study was to determine the effect of nutritional supplementation on tuberculosis incidence in household contacts of adults with microbiologically confirmed pulmonary tuberculosis.
Methods
In this field-based, open-label, cluster-randomised controlled trial, we enrolled household contacts of 2800 patients with microbiologically confirmed pulmonary tuberculosis across 28 tuberculosis units of the National Tuberculosis Elimination Programme in four districts of Jharkhand, India. The tuberculosis units were randomly allocated 1:1 by block randomisation to the control group or the intervention group, by a statistician using computer-generated random numbers. Although microbiologically confirmed pulmonary tuberculosis patients in both groups received food rations (1200 kcal, 52 grams of protein per day with micronutrients) for 6 months, only household contacts in the intervention group received monthly food rations and micronutrients (750 kcal, 23 grams of protein per day with micronutrients). After screening all household contacts for co-prevalent tuberculosis at baseline, all participants were followed up actively until July 31, 2022, for the primary outcome of incident tuberculosis (all forms). The ascertainment of the outcome was by independent medical staff in health services. We used Cox proportional hazards model and Poisson regression via the generalised estimating equation approach to estimate unadjusted hazard ratios, adjusted hazard ratios (aHRs), and incidence rate ratios (IRRs). This study is registered with CTRI-India, CTRI/2019/08/020490.
Findings
Between Aug 16, 2019, and Jan 31, 2021, there were 10345 household contacts, of whom 5328 (94.8%) of 5621 household contacts in the intervention group and 4283 (90.7%) of 4724 household contacts in the control group completed the primary outcome assessment. Almost two-thirds of the population belonged to Indigenous communities (eg, Santhals, Ho, Munda, Oraon, and Bhumij) and 34% (3543 of 10345) had undernutrition. We detected 31 (0.3%) of 10345 household contact patients with co-prevalent tuberculosis disease in both groups at baseline and 218 (2.1%) people were diagnosed with incident tuberculosis (all forms) over 21869 person-years of follow-up, with 122 of 218 incident cases in the control group (2.6% [122 of 4712 contacts at risk], 95% CI 2.2-3.1; incidence rate 1.27 per 100 person-years) and 96 incident cases in the intervention group (1.7% [96 of 5602], 1.4-2.1; 0.78 per 100 person-years), of whom 152 (69.7%) of 218 were patients with microbiologically confirmed pulmonary tuberculosis. Tuberculosis incidence (all forms) in the intervention group had an adjusted IRR of 0.61 (95% CI 0.43-0.85; aHR 0.59 [0.42-0.83]), with an even greater decline in incidence of microbiologically confirmed pulmonary tuberculosis (0.52 [0.35-0.79]; 0.51 [0.34-0.78]). This translates into a relative reduction of tuberculosis incidence of 39% (all forms) to 48% (microbiologically confirmed pulmonary tuberculosis) in the intervention group. An estimated 30 households (111 household contacts) would need to be provided nutritional supplementation to prevent one incident tuberculosis.
Interpretation
To our knowledge, this is the first randomised trial looking at the effect of nutritional support on tuberculosis incidence in household contacts, whereby the nutritional intervention was associated with substantial (39-48%) reduction in tuberculosis incidence in the household during 2 years of follow-up. This biosocial intervention can accelerate reduction in tuberculosis incidence in countries or communities with a tuberculosis and undernutrition syndemic.
(10). Richard Lafayette, et al. Efficacy and safety of a targeted-release formulation of budesonide in patients with primary IgA nephropathy (NefIgArd): 2-year results from a randomised phase 3 trial. 2023.
Background
IgA nephropathy is a chronic immune-mediated kidney disease and a major cause of kidney failure worldwide. The gut mucosal immune system is implicated in its pathogenesis, and Nefecon is a novel, oral, targeted-release formulation of budesonide designed to act at the gut mucosal level. We present findings from the 2-year, phase 3 NefIgArd trial of Nefecon in patients with IgA nephropathy.
Methods
In this phase 3, multicentre, randomised, double-blind, placebo-controlled trial, adult patients (aged 18 years) with primary IgA nephropathy, estimated glomerular filtration rate (eGFR) 35-90 mL/min per 1.73 m2, and persistent proteinuria (urine protein-creatinine ratio 0.8 g/g or proteinuria 1 g/24 h) despite optimised renin-angiotensin system blockade were enrolled at 132 hospital-based clinical sites in 20 countries worldwide. Patients were randomly assigned (1:1) to receive 16 mg/day oral capsules of Nefecon or matching placebo for 9 months, followed by a 15-month observational follow-up period off study drug. Randomisation via an interactive response technology system was stratified according to baseline proteinuria (2 or 2 g/24 h), baseline eGFR (60 or 60 mL/min per 1.73 m2), and region (Asia-Pacific, Europe, North America, or South America). Patients, investigators, and site staff were masked to treatment assignment throughout the 2-year trial. Optimised supportive care was also continued throughout the trial. The primary efficacy endpoint was time-weighted average of eGFR over 2 years. Efficacy and safety analyses were done in the full analysis set (ie, all randomly assigned patients). The trial was registered on ClinicalTrials.gov, NCT03643965, and is completed.
Findings
Patients were recruited to the NefIgArd trial between Sept 5, 2018, and Jan 20, 2021, with 364 patients (182 per treatment group) randomly assigned in the full analysis set. 240 (66%) patients were men and 124 (34%) were women, and 275 (76%) identified as White. The time-weighted average of eGFR over 2 years showed a statistically significant treatment benefit with Nefecon versus placebo (difference 5.05 mL/min per 1.73 m2 [95% CI 3.24 to 7.38], p0.0001), with a time-weighted average change of -2.47 mL/min per 1.73 m2 (95% CI -3.88 to -1.02) reported with Nefecon and -7.52 mL/min per 1.73 m2 (-8.83 to -6.18) reported with placebo. The most commonly reported treatment-emergent adverse events during treatment with Nefecon were peripheral oedema (31 [17%] patients, vs placebo, seven [4%] patients), hypertension (22 [12%] vs six [3%]), muscle spasms (22 [12%] vs seven [4%]), acne (20 [11%] vs two [1%]), and headache (19 [10%] vs 14 [8%]). No treatment-related deaths were reported.
Interpretation
A 9-month treatment period with Nefecon provided a clinically relevant reduction in eGFR decline and a durable reduction in proteinuria versus placebo, providing support for a disease-modifying effect in patients with IgA nephropathy. Nefecon was also well tolerated, with a safety profile as expected for a locally acting oral budesonide product.
(11). Christian Seerup Frandsen, et al. SURMOUNT-2: new advances for treating obese type 2 diabetes with Tirzepatide. Lancet 2023;402(10402):P586-588.
Obesity is the primary driver of developing type 2 diabetes and cardiovascular disease, and weight loss in people with type 2 diabetes is an effective means for improving glycaemic control and cardiovascular risk factors. 1 In the 2022 consensus report by the American Diabetes Association and the European Association for the Study of Diabetes, 2 a conceptual change was introduced in the treatment of type 2 diabetes that focused on a weight-centric approach inspired by recent results with semaglutide and tirzepatide trials. 2 The DIRECT study, 3 which used intensive lifestyle weight management in people with type 2 diabetes, reported a progressive improvement in glycated haemoglobin (HbA1c) and a reduced requirement of antidiabetic drugs with increasing weight reduction. A 15% weight loss-induced remission of diabetes in 31 (86%) of 36 participants was reported without use of antidiabetic drugs. 3 Tirzepatide, a glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 (GLP-1) receptor agonist that is taken once weekly, has been shown to lower HbA1c by about 2.2%, with around 50% of participants reaching HbA1c less than 5.7% in phase 3 trials assessing efficacy and safety in type 2 diabetes (SURPASS), 4 and this outcome was accompanied by bodyweight reduction of 9.5% to 12.5%.
(12). Talha Burki et al. Understanding postpartum haemorrhage. Lancet 2023
WHO has a new roadmap to tackle postpartum haemorrhage, the leading cause of maternal mortality. How much of a role does anaemia play?
Postpartum haemorrhage, typically defined as blood loss amounting to 500 mL or more within 24 h of birth, affects 14 million women annually. It is the world’s leading cause of maternal mortality, with around 70 000 deaths every year, almost all of which occur in sub-Saharan Africa and south Asia.
The failure of the uterus to contract, a phenomenon known as uterine atony, is widely thought to be the main reason for excessive bleeding during childbirth. Andrew Shennan, Professor of Obstetrics at King’s College London, UK, told The Lancet, When you are pregnant, your uterus has a pint of blood pumped to it per minuteIf the uterus stays relaxed after the baby has been delivered, it fills up with blood, the body assumes the pregnancy is ongoing and so the heart pumps more blood to the uterus, which comes straight out of the placental bed.
In which case, inducing contractions ought to minimise the bleeding. There are big blood vessels which need to be constricted after childbirth; contractions make those blood vessels constrict, and we have uterotonic drugs to induce contractions, explained Shennan. WHO recommends that all women giving birth are provided with uterotonics to prevent postpartum haemorrhage. A 2018 meta-analysis on prophylactic uterotonics, used by WHO to inform its recommendations, concluded that all seven of the examined agents were generally effective for preventing PPH [postpartum haemorrhage]. But not everyone agrees.
Ian Roberts, Professor of Epidemiology and Public Health at the London School of Hygiene & Tropical Medicine, UK, said, The WHO strategy for reducing maternal mortality from postpartum haemorrhage centres on the use of uterotonics, but there is no epidemiological evidence that uterine atony causes postpartum haemorrhage or that uterotonics have any effect on maternal mortality. He added, WHO is basing its policy on assumptions. The obstetrician treating a woman with PPH [postpartum haemorrhage] feels that her uterus is distended and decides that the cause is uterine atony. That is not causation in any epidemiological sense; it is just an opinion.
Roberts noted that a distended uterus could result from the bleeding, rather than the other way around. He was principal investigator on a study published earlier this year, which involved over 10 000 women. The study concluded that severe anaemia almost doubled the risk of postpartum haemorrhage, compared with moderate anaemia, and that uterine atony was commonly diagnosed as the cause of postpartum haemorrhage for women with anaemia. None of the obstetricians who treated the 742 women who had postpartum haemorrhage listed anaemia as the cause. Roberts argues that many obstetricians are unaware of the role of anaemia in postpartum haemorrhage and so erroneously attribute the condition to uterine atony. 500 million women of reproductive age have anaemia, 20 million of whom are severely anaemic.
WHO is stuck. They have classified uterotonics as life-saving, so they cannot realistically perform any randomised trials, but there is no evidence to back their position. They cannot say with certainty what effect uterotonics have, or whether the risks outweigh the benefits, said Roberts. He added that tranexamic acid is the only intervention proven to reduce maternal mortality from postpartum haemorrhage in a randomised trial the 2017 WOMAN trial published in The Lancet, for which Roberts was also principal investigator. He has communicated his concerns to WHO. However, Shennan believes that the opinion of the treating obstetrician matters. I have witnessed hundreds of situations where African women are dying in childbirth from bleeding. The uterus is relaxing and blood is pouring out and if you make the uterus contract the bleeding stops, he said. Shennan pointed out that randomly assigning someone who is bleeding to death to receive a drug or placebo would be unethical and very challenging to study. We know that uterotonics work because in countries where they do not have uterotonics, there are literally hundreds of times more women dying in childbirth. You do not need a trial to show that, said Shennan. He drew an analogy with blood transfusions, which have never had their effectiveness proven in randomised trials, and noted that factors such as anaemia and obesity could be increasing the risk of postpartum haemorrhage by increasing the risk of uterine atony.
Roberts expressed his dismay that the 2023-30 WHO Roadmap on postpartum haemorrhage states that uterotonics are lifesaving without hard evidence demonstrating this to be true. A spokesperson for WHO told The Lancet that the organisation’s recommendations are formulated by external, independent experts convened by WHO, based on consideration of the entirety of available evidence on a given topic, including, but not limited to randomised controlled trials. He said that the contributions of anaemia and uterine atony to postpartum haemorrhage and maternal death are well documented. We clearly need multiple approaches to save lives. The approaches are not necessarily mutually exclusive.
(13). Robert Spencer et al. Noisy breathing in a 2-month-old baby: a pulmonary artery sling. Lancet 2023.
A 2-month-old baby boy, who had noisy breathing since birth that increased in volume during feeding and times of agitation, was referred to our unit for assessment (video).
The baby had been born at full term by vaginal delivery; there was no history of infection, foreign body aspiration, intubation, or other airway injury. Investigations previously done included a laryngoscopy, which showed no evidence of laryngomalacia or other abnormalities, an unremarkable barium swallow, and a chest x-ray that showed a left-sided aortic arch.
On examination the patient was in mild respiratory distress. He had wheezing and stridor and was mildly tachypnoeic with a respiratory rate of 68 breaths per min (normal in a 2-month-old: 30-60). His temperature was 36.4deg C.
Transthoracic echocardiography showed normal intracardiac anatomy and a left-sided aortic arch with normal branching of the head and neck vessels. However, the left pulmonary artery had an anomalous course (figure): a CT angiogram showed the left pulmonary artery originated from the right pulmonary artery confirming the suspected diagnosis of a pulmonary artery sling (figure; appendix).
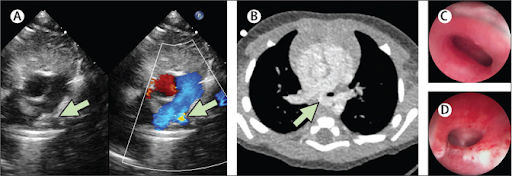
A rigid bronchoscopy showed a long segment of tracheal stenosis, with complete tracheal rings in the distal half of the trachea. Additionally, external compression of the carina by the left pulmonary artery was noted (figure; appendix).
We referred to a specialist centre for an operation to reimplant the left pulmonary artery into the main pulmonary artery; a slide tracheoplasty, which involved dividing and reconstructing part of the trachea to create a wider airway, was also done.
The baby was allowed home after 3 weeks. At follow-up, 2 months later, our patient was well without any symptoms.
Congenital stridor a sign of upper airway obstruction results from several conditions including laryngomalacia, vocal cord paralysis, and laryngeal webs. Stridor may also occur due to extrinsic compression on the airway by vascular rings: a double aortic arch or right aortic arch with an aberrant left subclavian artery.
Pulmonary artery sling is a rare vascular anomaly causing external airway obstruction. In contrast to a vascular ring, which may cause respiratory and feeding problems, a sling does not encircle the trachea and oesophagus. Rather, the left pulmonary artery arises from the posterior aspect of the right pulmonary artery, passes over the right main-stem bronchus, turns to the left, and courses between the trachea and oesophagus, before reaching the left pulmonary hilum.
When a sling is suspected, advanced imaging modalities confirm the diagnosis and delineate the anatomy. A bronchoscopy is necessary to evaluate the airway because associated anomalies of the tracheobronchial tree are common and approximately 50% of patients have tracheal stenosis. Additionally, patients frequently have concomitant cardiac lesions such as tetralogy of Fallot, which can be repaired simultaneously.
(14). Combining anti-inflammatory drug with the morning after pill boosts effectiveness, study finds. BMJ 2023;382.
A combination of levonorgestrel known as plan B or the morning after pill and the anti-inflammatory drug piroxicam is more effective in preventing pregnancy compared with levonorgestrel alone, according to a randomised controlled trial.1
The study involved 860 women who sought emergency contraception within 72 hours of unprotected intercourse at a major community sexual and reproductive health service in Hong Kong between 2018 and 2022. The results, published in the Lancet, showed that the combination regimen prevented 94.7% of expected pregnancies, compared with 63.4% with levonorgestrel alone.
Lead author Raymond Li, clinical associate professor at the University of Hong Kongs department of obstetrics and gynaecology, said, Our study is the first to suggest that a readily available and safe drug taken at the same time as the levonorgestrel pill can prevent more pregnancies than levonorgestrel alone.
(15). Peter J. Blankestijn et al. Effect of Hemodiafiltration or Hemodialysis on Mortality in Kidney Failure. N Engl J Med 2023;389:700-709.
Background
Several studies have suggested that patients with kidney failure may benefit from high-dose hemodiafiltration as compared with standard hemodialysis. However, given the limitations of the various published studies, additional data are needed.
Methods
We conducted a pragmatic, multinational, randomized, controlled trial involving patients with kidney failure who had received high-flux hemodialysis for at least 3 months. All the patients were deemed to be candidates for a convection volume of at least 23 liters per session (as required for high-dose hemodiafiltration) and were able to complete patient-reported outcome assessments. The patients were assigned to receive high-dose hemodiafiltration or continuation of conventional high-flux hemodialysis. The primary outcome was death from any cause. Key secondary outcomes were cause-specific death, a composite of fatal or nonfatal cardiovascular events, kidney transplantation, and recurrent all-cause or infection-related hospitalizations.
Results
A total of 1360 patients underwent randomization: 683 to receive high-dose hemodiafiltration and 677 to receive high-flux hemodialysis. The median follow-up was 30 months (interquartile range, 27 to 38). The mean convection volume during the trial in the hemodiafiltration group was 25.3 liters per session. Death from any cause occurred in 118 patients (17.3%) in the hemodiafiltration group and in 148 patients (21.9%) in the hemodialysis group (hazard ratio, 0.77; 95% confidence interval, 0.65 to 0.93).
Conclusions
In patients with kidney failure resulting in kidney-replacement therapy, the use of high-dose hemodiafiltration resulted in a lower risk of death from any cause than conventional high-flux hemodialysis. (Funded by the European Commission Research and Innovation; CONVINCE Dutch Trial)
(16). Mohammed Shanshal et al. Serum Sickness. N Engl J Med 2023;389:749.
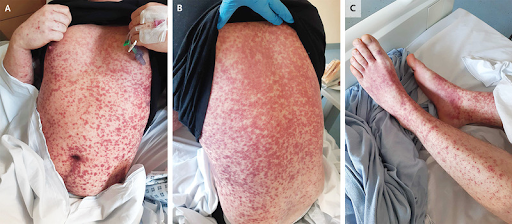
A 30-year-old man with recently diagnosed aplastic anemia presented to the emergency department with a 2-day history of fever, nonpruritic rash, and ankle and knee pain. He reported having no hives or jaw pain. Ten days before the onset of symptoms, he had completed a course of horse antithymocyte globulin as treatment for his aplastic anemia. His body temperature was 39.6deg C. Physical examination was notable for a morbilliform rash across his torso (Panels A and B) and arms and a purpuric rash on the legs (Panel C). Mild swelling was noted in the periorbital region, but the mucous membranes were not involved. Laboratory studies were notable for worsening neutropenia, low C3 and C4 levels, a C-reactive protein level of 114 mg per liter (reference value, 5), and negative blood cultures. A clinical diagnosis of serum sickness was made. Serum sickness is a type III hypersensitivity reaction due to the formation of antigen-antibody or immune complexes. The condition classically occurs after the therapeutic administration of nonhuman protein and manifests as a triad of fever, rash, and arthralgia, as in this case. After a 5-day course of intravenous glucocorticoids, the patients symptoms had resolved. Horse antithymocyte globulin was added to the patients list of drug allergies and not used again.
(17). Ke Xiao, M.D. et al. Testicular Tuberculosis. N Engl J Med 2023;389:e13.
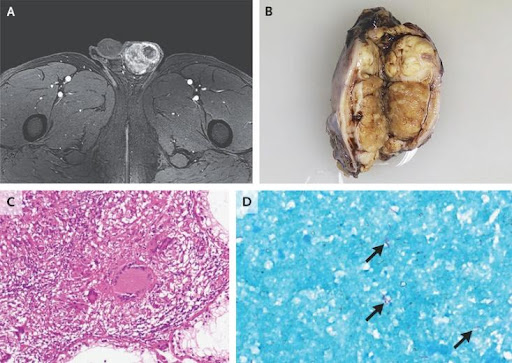
A 42-year-old man presented to the urology clinic with a 2-month history of painless enlargement of the left testicle. He reported no fevers, night sweats, weight loss, respiratory symptoms, or urethral discharge. The physical examination was notable for an enlarged, firm, nontender left testicle. Magnetic resonance imaging of the pelvis showed a lobulated left testicular mass with heterogeneous enhancement (Panel A). Testing for serum tumor markers for testicular cancer was negative. Owing to concern about testicular cancer, a radical inguinal orchiectomy was performed. Gross examination of the excised testis showed necrotic nodules (Panel B), and histopathological examination showed granulomatous inflammation with caseous necrosis (Panel C) and acid-fast bacilli (Panel D, arrows). A real-time-polymerase-chain-reaction assay identified Mycobacterium tuberculosis. Computed tomography of the chest was normal. A diagnosis of testicular tuberculosis was made. A 9-month course of antituberculosis therapy was prescribed. At follow-up 1 year after the initial presentation, the patient was in good health.
(18). Steven K. Grinspoon et al. Pitavastatin to Prevent Cardiovascular Disease in HIV Infection. N Engl J Med 2023;89:687-699.
Background
The risk of cardiovascular disease is increased among persons with human immunodeficiency virus (HIV) infection, so data regarding primary prevention strategies in this population are needed.
Methods
In this phase 3 trial, we randomly assigned 7769 participants with HIV infection with a low-to-moderate risk of cardiovascular disease who were receiving antiretroviral therapy to receive daily pitavastatin calcium (at a dose of 4 mg) or placebo. The primary outcome was the occurrence of a major adverse cardiovascular event, which was defined as a composite of cardiovascular death, myocardial infarction, hospitalization for unstable angina, stroke, transient ischemic attack, peripheral arterial ischemia, revascularization, or death from an undetermined cause.
Results
The median age of the participants was 50 years (interquartile range, 45 to 55); the median CD4 count was 621 cells per cubic millimeter (interquartile range, 448 to 827), and the HIV RNA value was below quantification in 5250 of 5997 participants (87.5%) with available data. The trial was stopped early for efficacy after a median follow-up of 5.1 years (interquartile range, 4.3 to 5.9). The incidence of a major adverse cardiovascular event was 4.81 per 1000 person-years in the pitavastatin group and 7.32 per 1000 person-years in the placebo group (hazard ratio, 0.65; 95% confidence interval [CI], 0.48 to 0.90; P=0.002). Muscle-related symptoms occurred in 91 participants (2.3%) in the pitavastatin group and in 53 (1.4%) in the placebo group; diabetes mellitus occurred in 206 participants (5.3%) and in 155 (4.0%), respectively.
Conclusions
Participants with HIV infection who received pitavastatin had a lower risk of a major adverse cardiovascular event than those who received placebo over a median follow-up of 5.1 years. (Funded by the National Institutes of Health
(19). Abdullah K Malik et al. Appendicectomy remains treatment of choice for patients with acute appendicitis. BMJ 2023;382:e074652
Although many patients were safely managed with antibiotics during covid-19, Abdullah K Malik and colleagues argue that the associated risks and patient burden make surgery the best approach for appendicitis
Acute appendicitis is a common condition that almost all doctors will encounter at some point during their career. Until recently patients were usually treated surgically with an appendicectomy, with antibiotics used for those with prohibitively high perioperative risks because of comorbidities or an appendiceal mass. However, conservative management of acute appendicitis was advocated during the covid-19 pandemic because of concerns about aerosol formation during laparoscopic surgery and higher risk of morbidity and mortality in patients with covid-19.12 Further evidence has accumulated on the safety and effectiveness of antibiotics in adults with acute appendicitis.345678 This, together with greater use of computed tomography to identify complications, has shifted attitudes and led to antibiotic treatment becoming more widely used.
Although antibiotic treatment can be effective in patients with uncomplicated appendicitis (box 1), some will still require surgery, which may be more extensive if antibiotics fail and surgery is delayed, and there is a substantial risk of recurrence.910111213 Patients need to be informed about treatment alternatives and made aware of all the relevant risks so that they can decide what is most suitable for their circumstances. However, we argue that antibiotics should not be presented as an equivalent treatment to surgery when explaining therapeutic options.
What we need to know
Uncomplicated appendicitis
Uncomplicated appendicitis is acute inflammation of the appendix without appendicolith, perforation, abscess, pelvic inflammatory changes, or suspicion of tumour
Diagnosis is based on computed tomography or intraoperative findings
Lack of standardised definitions about the features of complicated appendicitis may lead to variability in reported outcomes of patients with acute complicated or uncomplicated appendicitis
Evidence supports appendicectomy as firstline therapy
(20). Jerry H. Gurwitz. The Paradoxical Decline of Geriatric Medicine as a Profession. JAMA. 2023;330(8):693-694.
Thirty-five years ago, geriatrics officially became a specialty of medicine. At that time, there were 76 million baby boomers who would begin turning 65 in 2011, a compelling demographic imperative for this new specialty that specifically focused on older adults.
Geriatrics is a field especially attractive to some physicians because of its differences from other specialties, including elements beyond single medical conditions such as multimorbidity, polypharmacy, function, and cognition. Geriatrics also places a special emphasis on interdisciplinary team care for complex older patients, and the needs of family caregivers.
However, accumulating evidence suggests that the profession of geriatric medicine has fallen into decline. The number of board-certified geriatricians in the US fell from 10 270 in 2000 to 7413 in 2022.1 This attrition relates to the retirement of many physicians who were among the first to be certified in geriatrics, as well as some choosing not to recertify as required every 10 years. This drop has been further exacerbated by a failing trainee pipeline. In the 2022 national geriatrics fellowship match, only 177 positions were filled of 411 positions offered (43%), the lowest percentage of all fellowships across 71 specialties of medicine.2
The irony is that despite substantial investments in geriatric research and education, the stars have never seemed to align for geriatricians. The National Institute on Aging (NIA), with an annual budget exceeding $4 billion (third largest across the National Institutes of Health), has funded applied geriatrics research and generous training awards for early-stage clinician-investigators who pursue research activities focused on improving the health of older Americans. However, of the small number of fellowship-trained geriatricians, very few pursue research careers. Over the past 3 years (2020, 2021, and 2022), of 33 Beeson scholars, the NIAs most prestigious career development award program, just 2 have been geriatricians.
Beginning in 1988, to support efforts to increase the number of geriatrics-trained faculty and training initiatives in geriatrics focused on medical students and residents, the John A. Hartford Foundation and the Donald W. Reynolds Foundation combined to invest nearly $160 million.3 However, in 2011, the Hartford Foundation made a strategic decision to pivot away from supporting efforts to build academic capacity in geriatric medicine to fund more broadly focused health system initiatives. The other major funder of geriatric educational programs, the Reynolds Foundation, closed down permanently having spent down all of its assets.
Accrediting organizations like the Liaison Committee on Medical Education (LCME) and the Accreditation Council for Graduate Medical Education (ACGME) have overlooked the need to teach geriatric principles to medical students and residents, with no requirements of medical schools or residency programs to have geriatrics-specific, competency-based performance standards, or to have geriatricians involved in educational and training activities.
Even a favorable financial framework relating to the care of older adults under Medicare Advantage, with 31 million enrollees, has not been helpful to the profession of geriatric medicine. While insurers and health care delivery systems have invested heavily to creatively capture high-risk diagnosis codes, allowing for payment at higher rates, far less attention has been paid to implementing innovative programs developed by geriatricians to improve the care of older adults across all clinical settings,4,5 or to hire geriatricians to provide primary care to older patients with complex conditions. As a result, the profession of geriatric medicine has benefited little from this advantageous financial situation for insurers and health care delivery organizations.
Some attribute the challenges faced by the profession of geriatric medicine to lower compensation. That is because geriatric medicine is one of very few specialties for which fellowship training and board certification result in a lower salary than if neither had been pursued. According to the 2022 Association of American Medical Colleges (AAMC) faculty salary survey, the median salary of geriatricians was 9% lower than that of general internists and 14% lower than that of hospitalists. In addition, the attainment of board certification in geriatric medicine does not meaningfully influence job opportunities or practice activities.
However, the situation that has befallen geriatric medicine is more complicated than just lower compensation. Despite being a profession that also offers lower salaries, pediatrics remains an attractive career path for medical students. Attitudes of medical students and residents about aging and older adults strongly influence their career decision-making. In one study of medical students and residents training at 2 urban teaching hospitals in northern California, negative perceptions of older adults included that they were inherently end of life patients, that they were cognitively impaired, that their medical problems were complex and unlikely to be resolved, and that they were socially needy and slow to interact with.6
In her 2019 book Elderhood,7 geriatrician Louise Aronson wrote, When I tell someone what I do for a living, they usually have one of two reactions. Either their face contorts as if theyd just smelled something foul, or they offer compliments about my selfless dedicationThese apparently opposite responses are actually the same. Both imply that what Im doing is something no one in their right mind would ever do.
While the importance of the profession of geriatric medicine and the need for geriatricians seem obvious, it should not surprise anyone that it is the career choice of ever-diminishing numbers of medical students and residents. The demographic trends in our population have not attracted them to the field; societal attitudes about aging have clearly compounded the negative effects of lower compensation and lack of prestige on their career decisions.
Our nation is beginning to experience the full impact of the aging of our population. Sadly, our health system and its workforce are wholly unprepared to deal with an imminent surge of multimorbidity, functional impairment, dementia, and frailty. This is the reality that health care organizations and medical schools have not adequately appreciated, or have chosen to ignore.
It will be extraordinarily difficult to alter the trajectory of the specialty of geriatric medicine. Geriatricians will never stop advocating for better care of our aging population and the need for physicians with expertise in geriatric medicine. The decline of the profession of geriatric medicine matters, and all too soon we will all realize why.
(21). Polio vaccines: hope, hype, and history repeating? BMJ 2023;382:p1763
Announcement of new polio vaccines has once again raised hopes of eradicating polio. But the ongoing difficulties of their predecessors provide a cautionary tale, writes Robert Fortner
In June 2023, a research article in Nature heralded new, more stable versions of the vaccines against two of the three types of poliovirus (types 1 and 3).1 Super-engineered polio vaccines created to help end polio, read a BBC headline.2 Polio endgame finish is in sight,3 added a Nature news article.3 The backdrop, however, is a little muddier.
A similar fanfare had greeted the first of this new generation of oral polio vaccines in 2021. Novel oral polio vaccine type 2 (nOPV2) targets type 2 polio and went straight into widespread use. But it remains far from clear how well nOPV2 works.
Before it was approved for emergency use, scientists warned that nOPV2 would not solve the problem set for it: to stamp out vaccine-derived polio. So far, it has not done so. Instead there are unanswered questions about the vaccines performance, whether the decision to rely on it was right, and whether theres a viable path to the dream of global eradication even with a full suite of modernised vaccines.
Noblest of intentions
The quest to rid the world of polio began in earnest in the late 1980s with the formation of the Global Polio Eradication Initiative (GPEI), a public-private partnership led by the World Health Organization together with Unicef, the US Centers for Disease Control and Prevention (CDC), and Rotary International. They were joined later by the Bill and Melinda Gates Foundation and the global vaccine alliance Gavi. Just one disease smallpox has been eradicated globally; attempts have also been made to eradicate malaria and guinea worm.
Wild (naturally occurring) polio has been brought close to oblivion, restricted to Afghanistan and Pakistan.
(22). Doctors to be kind. BMJ 2023;382:p1976
The GMC, UK, elaborates on the meaning of kindness, courtesy, and respect. It means that doctors should communicate sensitively and considerately, particularly when sharing potentially distressing issues about the patients prognosis and care. Similarly, doctors should be willing to explain the reasons for the options they offer (and the options they dont) and any recommendations they make. The explanation dispels the worry that kindness is incompatible with breaking bad news, refusing patient requests, or making recommendations. Rather, it informs how these actions, and others, should be performed. This is in line with what philosopher Robert Audi called duties of manner.2 These duties relate to how we do things, since it is possible to do the right thing, like disclosing a grim prognosis to a patient, in the wrong way (e.g., insensitively or callously).
What kindness requires differs from culture to culture. Yet, the same is true of other qualities mentioned in the guidance, such as courtesy, respect, openness, fairness, trust, honesty, and professionalism. There is no need, in my view, to seek a technical definition of kindness. It is a word whose ordinary meaning most of us understand without much difficulty.
However, when determining whether a doctor has been kind or unkind, decision makers must be sensitive to context and culture.
William Osler remarked that a doctor needs a clear head and a kind heart.3 In an unpublished draft of an address to medical students, he wrote the kindly word, the cheerful greeting, the sympathetic look, trivial though they may seem, help to brighten the paths of the poor sufferers and are often as oil and wine to the bruised spirits entrusted to our careremember that every patient will examine you critically and form an estimate of you by the way in which you conduct yourself at the bedside.4 The Latin root of beneficence (doing good for your patients), one of the four principles of medical ethics along with non-maleficence (respect for autonomy and justice) is beneficentia: active kindness. It is surely right that most doctors strive to be kind but, on a bad day, at the end of a busy shift, or when confronted with unsympathetic patients or relatives, it is easy to forget this noble intention.
The GMC says little about the specific requirements of kindness with respect to colleagues, defined in the guidance as including anyone you work with, whether or not they are a medical professional. However, just as kindness does not preclude difficult conversations or unpopular advice to patients, it does not prohibit doctors from raising concerns with, or about, colleagues. Rather, it dictates the way in which these acts are done.
The fear that the kindness requirements will open floodgates of complaints is misplaced. The heavens will not fall. The current guidance already contains instructions that doctors should treat patients politely, maintain good relationships with colleagues, and treat them with respect. The reference to kindness in the updated guidance serves to remind doctors to apply their skill and knowledge in a manner that respects the dignity, vulnerability, and humanity of their sick patients, while treating colleagues with due consideration. In these times of high stress and low morale among healthcare staff, such a rminder is no bad thing.
(23). Mauro Odd et al. The Neurological Pupil index for outcome prognostication in people with acute brain injury (ORANGE): a prospective, observational, multicentre cohort study. 2023.
Background
Improving the prognostication of acute brain injury is a key element of critical care. Standard assessment includes pupillary light reactivity testing with a hand-held light source, but findings are interpreted subjectively; automated pupillometry might be more precise and reproducible. We aimed to assess the association of the Neurological Pupil index (NPi)a quantitative measure of pupillary reactivity computed by automated pupillometrywith outcomes of patients with severe non-anoxic acute brain injury.
Methods
ORANGE is a multicentre, prospective, observational cohort study at 13 hospitals in eight countries in Europe and North America. Patients admitted to the intensive care unit after traumatic brain injury, aneurysmal subarachnoid haemorrhage, or intracerebral haemorrhage were eligible for the study. Patients underwent automated infrared pupillometry assessment every 4 h during the first 7 days after admission to compute NPi, with values ranging from 0 to 5 (with abnormal NPi being 3). The co-primary outcomes of the study were neurological outcome (assessed with the extended Glasgow Outcome Scale [GOSE]) and mortality at 6 months. We used logistic regression to model the association between NPi and poor neurological outcome (GOSE 4) at 6 months and Cox regression to model the relation of NPi with 6-month mortality. This study is registered with ClinicalTrials.gov, NCT04490005.
Findings
Between Nov 1, 2020, and May 3, 2022, 514 patients (224 with traumatic brain injury, 139 with aneurysmal subarachnoid haemorrhage, and 151 with intracerebral haemorrhage) were enrolled. The median age of patients was 61 years (IQR 46-71), and the median Glasgow Coma Scale score on admission was 8 (5-11). 40 071 NPi measurements were taken (median 40 per patient [20-50]). The 6-month outcome was assessed in 497 (97%) patients, of whom 160 (32%) patients died, and 241 (47%) patients had at least one recording of abnormal NPi, which was associated with poor neurological outcome (for each 10% increase in the frequency of abnormal NPi, adjusted odds ratio 1.42 [95% CI 1.27-1.64]; p0.0001) and in-hospital mortality (adjusted hazard ratio 5.58 [95% CI 3.92-7.95]; p0.0001).
Interpretation
NPi has clinically and statistically significant prognostic value for neurological outcome and mortality after acute brain injury. Simple, automatic, repeat automated pupillometry assessment could improve the continuous monitoring of disease progression and the dynamics of outcome prediction at the bedside.
(24). Jean-Louis Pepin et al. Health trajectories before initiation of non-invasive ventilation for chronic obstructive pulmonary disease: a French nationwide database analysis. 2023.
Background
Chronic obstructive pulmonary disease (COPD) is the most common indication for long-term domiciliary non-invasive ventilation (NIV) but there is uncertainty in data supporting current guidelines. This study described health trajectories before initiation of at-home NIV in people with COPD, and compared mortality outcomes between groups with different pre-NIV health trajectories.
Methods
Data were from the French national health insurance reimbursement system database for individuals with COPD aged 40 years and 1 reimbursement for NIV between 1 January 2015 and 31 December 2019. Common health trajectories were determined using time sequence analysis through K-clustering (TAK analysis).
Findings
Data from 54,545 individuals were analysed; the population was elderly (median age 70 years) with multiple comorbidities. Four clusters were generated. Cluster 1 (n = 35,975/54,545; 66%) had NIV initiated in ambulatory settings or after the first acute event/exacerbation. Cluster 2 (6653/54,545; 12%) started NIV after 2 severe exacerbations in the previous 6 months. Cluster 3 (11,375/54,545; 21%) started NIV after frequent severe COPD-related exacerbations in the previous year. Cluster 4 (652/54,545; 1%) started NIV after many long-lasting severe exacerbations. The four clusters differed in age, sex, comorbidities, pre-NIV investigations, and prescriber/location of NIV initiation. Mortality differed significantly between clusters: highest in Cluster 4 and lowest in Cluster 1.
Interpretation
The significant heterogeneity in clinical initiation of NIV probably reflects the current lack of strong evidence and guideline recommendations. Knowledge about the characteristics and outcomes in different clusters should be used to address inequities and facilitate more consistent and personalised use domiciliary NIV in COPD.
(25). Tiffany et al. Expedited transfer to a cardiac arrest centre for Non-ST-elevation out-of-hospital cardiac arrest (ARREST): a UK prospective, multicentre, parallel, randomised clinical trial. 2023.
Background
The International Liaison Committee on Resuscitation has called for a randomised trial of delivery to a cardiac arrest centre. We aimed to assess whether expedited delivery to a cardiac arrest centre compared with current standard of care following resuscitated cardiac arrest reduces deaths.
Methods
ARREST is a prospective, parallel, multicentre, open-label, randomised superiority trial. Patients (aged 18 years) with return of spontaneous circulation following out-of-hospital cardiac arrest without ST elevation were randomly assigned (1:1) at the scene of their cardiac arrest by London Ambulance Service staff using a secure online randomisation system to expedited delivery to the cardiac catheter laboratory at one of seven cardiac arrest centres or standard of care with delivery to the geographically closest emergency department at one of 32 hospitals in London, UK. Masking of the ambulance staff who delivered the interventions and those reporting treatment outcomes in hospital was not possible. The primary outcome was all-cause mortality at 30 days, analysed in the intention-to-treat (ITT) population excluding those with unknown mortality status. Safety outcomes were analysed in the ITT population. The trial was prospectively registered with the International Standard Randomised Controlled Trials Registry, 96585404.
Findings
Between Jan 15, 2018, and Dec 1, 2022, 862 patients were enrolled, of whom 431 (50%) were randomly assigned to a cardiac arrest centre and 431 (50%) to standard care. 20 participants withdrew from the cardiac arrest centre group and 19 from the standard care group, due to lack of consent or unknown mortality status, leaving 411 participants in the cardiac arrest centre group and 412 in the standard care group for the primary analysis. Of 822 participants for whom data were available, 560 (68%) were male and 262 (32%) were female. The primary endpoint of 30-day mortality occurred in 258 (63%) of 411 participants in the cardiac arrest centre group and in 258 (63%) of 412 in the standard care group (unadjusted risk ratio for survival 1.00, 95% CI 0.90-1.11; p=0.96). Eight (2%) of 414 patients in the cardiac arrest centre group and three (1%) of 413 in the standard care group had serious adverse events, none of which were deemed related to the trial intervention.
Interpretation
In adult patients without ST elevation, transfer to a cardiac arrest centre following resuscitated cardiac arrest in the community did not reduce deaths.
(26). Kyndaron Reinier et al. Warning symptoms associated with imminent sudden cardiac arrest: a population-based case-control study with external validation. 2023.
Background
Sudden cardiac arrest is a global public health problem with a mortality rate of more than 90%. Prearrest warning symptoms could be harnessed using digital technology to potentially improve survival outcomes. We aimed to estimate the strength of association between symptoms and imminent sudden cardiac arrest.
Methods
We conducted a case-control study of individuals with sudden cardiac arrest and participants without sudden cardiac arrest who had similar symptoms identified from two US community-based studies of patients with sudden cardiac arrest in California state, USA (discovery population; the Ventura Prediction of Sudden Death in Multi-Ethnic Communities [PRESTO] study), and Oregon state, USA (replication population; the Oregon Sudden Unexpected Death Study [SUDS]). Participant data were obtained from emergency medical services reports for people aged 18-85 years with witnessed sudden cardiac arrest (between Feb 1, 2015, and Jan 31, 2021) and an inclusion symptom. Data were also obtained from corresponding control populations without sudden cardiac arrest who were attended by emergency medical services for similar symptoms (between Jan 1 and Dec 31, 2019). We evaluated the association of symptoms with sudden cardiac arrest in the discovery population and validated our results in the replication population by use of logistic regression models.
Findings
We identified 1672 individuals with sudden cardiac arrest from the PRESTO study, of whom 411 patients (mean age 65.7 [SD 12.4] years; 125 women and 286 men) were included in the analysis for the discovery population. From a total of 76 734 calls to emergency medical services, 1171 patients (mean age 61.8 [SD 17.3] years; 643 women, 514 men, and 14 participants without data for sex) were included in the control group. Patients with sudden cardiac arrest were more likely to have dyspnoea (168 [41%] of 411 vs 262 [22%] of 1171; p0.0001), chest pain (136 [33%] vs 296 [25%]; p=0.0022), diaphoresis (50 [12%] vs 90 [8%]; p=0.0059), and seizure-like activity (43 [11%] vs 77 [7%], p=0.011). Symptom frequencies and patterns differed significantly by sex. Among men, chest pain (odds ratio [OR] 2.2, 95% CI 1.6-3.0), dyspnoea (2.2, 1.6-3.0), and diaphoresis (1.7, 1.1-2.7) were significantly associated with sudden cardiac arrest, whereas among women, only dyspnoea was significantly associated with sudden cardiac arrest (2.9, 1.9-4.3). 427 patients with sudden cardiac arrest (mean age 62.2 [SD 13.5]; 122 women and 305 men) were included in the analysis for the replication population and 1238 patients (mean age 59.3 [16.5] years; 689 women, 548 men, and one participant missing data for sex) were included in the control group. Findings were mostly consistent in the replication population; however, notable differences included that, among men, diaphoresis was not associated with sudden cardiac arrest and chest pain was associated with sudden cardiac arrest only in the sex-stratified multivariable analysis.
Interpretation
The prevalence of warning symptoms was sex-specific and differed significantly between patients with sudden cardiac arrest and controls. Warning symptoms hold promise for prediction of imminent sudden cardiac arrest but might need to be augmented with additional features to maximise predictive power.
(27) Dominik Stelzle et al. Evaluation of a point-of-care test for the diagnosis of Taenia solium neurocysticercosis in rural southern Tanzania: a diagnostic accuracy study. 2023.
Background
Neurocysticercosis is a common cause of epilepsy in Taenia solium-endemic areas in sub-Saharan Africa but is often undiagnosed because of an absence of affordable diagnostic tools. This study evaluated the diagnostic accuracy of a T solium cysticercosis antibody-detecting lateral-flow point-of-care assay (TS POC test) for the neuroimaging-based diagnosis of neurocysticercosis.
Methods
Patients with epileptic seizures or severe progressive headache were recruited consecutively from three hospitals in southern Tanzania. All patients were tested with the TS POC test. All patients positive for cysticercosis on the TS POC test and every tenth patient who was negative for cysticercosis received a brain CT examination and underwent reference testing for T solium cysticercosis (ie, rT24H-EITB, LLGP-EITB, and antigen ELISA). The primary outcome of the study was the sensitivity of the TS POC test for the diagnosis of neurocysticercosis.
Findings
Of the 601 recruited participants, 102 (17%) tested positive for cysticercosis with the TS POC test. Overall, 48 (62%) of the 77 patients positive for cysticercosis and five (17%) of the 29 patients negative for cysticercosis on the TS POC test had CT-confirmed neurocysticercosis. The TS POC test yielded a sensitivity of 49% (uncertainty interval [UI] 41-58) for neurocysticercosis. Sensitivity was similar to that of the rT24H-EITB (44%, UI 37-51) and the antigen ELISA (50%, 43-56). For the subset of neurocysticercosis cases with at least one active (ie, vesicular) lesion, sensitivity was above 98% for the TS POC test, the rT24H-ETIB, and the antigen ELISA.
Interpretation
The TS POC test showed promising results for the diagnosis of neurocysticercosis in patients with vesicular lesions, which need to be confirmed in a larger study. This test could be considered to support policies on screening patients with suspected neurocysticercosis in clinical settings, which would allow appropriate referral for neuroimaging and early treatment.
Funding
German Federal Ministry of Education and Research and the European Developing Countries Clinical Trials Partnership
(28). Orestis Kanter Bax et al. Personality disorder. BMJ 2023;382:e050290
What we need to know
Personality disorders are a set of complex emotional difficulties. They are common, often unrecognised, and are associated with mental and physical health comorbidities and reduced life expectancy
Personality disorders are perceived as stigmatising diagnoses. Alternative terms have been proposed. New classification systems help in moving away from rigid use of categorical diagnoses
Assessment and management in primary care require a non-judgmental approach that builds trust through attentiveness, validation, openness, and consistency
Holistic care for people with personality disorders can be improved with reflective practice structures, staff training, collaboration, and team working
Personality disorders describe a set of long standing complex emotional difficulties, which are common, highly stigmatised, and potentially disabling. They are frequently under-recognised and may run a long course when people lack access to appropriate treatment. Recent developments in evidence, guidelines, and policy have placed an emphasis on public awareness, de-stigmatisation, training professionals in generalist settings, improving access to specialist care, and improving physical health outcomes.12 This article provides an overview of the latest information on the assessment and management of personality disorders in primary care, with an emphasis on borderline personality disorder (also referred to as emotionally unstable personality disorder).
What are personality disorders?
Personality disorders are pervasive and enduring, affecting the emotional, cognitive, and behavioural functioning of a person, expressed in relation to their self (eg, identity, self-evaluation, affect regulation, direction) and others (eg, intimacy, boundaries, sense of security in relationships)
(29). Amani Meaidi et al. Venous thromboembolism with use of hormonal contraception and non-steroidal anti-inflammatory drugs: nationwide cohort study. BMJ 2023;382:e074450.
Objective: To study the influence of concomitant use of hormonal contraception and non-steroidal anti-inflammatory drugs (NSAIDs) on the risk of venous thromboembolism.
Design: Nationwide cohort study.
Setting: Denmark through national registries.
Participants: All 15-49 year old women living in Denmark between 1996 and 2017 with no medical history of any venous or arterial thrombotic event, cancer, thrombophilia, hysterectomy, bilateral oophorectomy, sterilisation, or infertility treatment (n=2029065).
Main outcome measure: A first time discharge diagnosis of lower limb deep venous thrombosis or pulmonary embolism.
Results: Among 2.0 million women followed for 21.0 million person years, 8710 venous thromboembolic events occurred. Compared with non-use of NSAIDs, use of NSAIDs was associated with an adjusted incidence rate ratio of venous thromboembolism of 7.2 (95% confidence interval 6.0 to 8.5) in women not using hormonal contraception, 11.0 (9.6 to 12.6) in women using high risk hormonal contraception, 7.9 (5.9 to 10.6) in those using medium risk hormonal contraception, and 4.5 (2.6 to 8.1) in users of low/no risk hormonal contraception. The corresponding numbers of extra venous thromboembolic events per 100000 women over the first week of NSAID treatment compared with non-use of NSAIDs were 4 (3 to 5) in women not using hormonal contraception, 23 (19 to 27) in women using high risk hormonal contraception, 11 (7 to 15) in those using medium risk hormonal contraception, and 3 (0 to 5) in users of low/no risk hormonal contraception.
Conclusions: NSAID use was positively associated with the development of venous thromboembolism in women of reproductive age. The number of extra venous thromboembolic events with NSAID use compared with non-use was significantly larger with concomitant use of high/medium risk hormonal contraception compared with concomitant use of low/no risk hormonal contraception. Women needing both hormonal contraception and regular use of NSAIDs should be advised accordingly.
(30). Jacqui Wise. Virtual wards: NICE sets out guidance on managing acute respiratory infections at home. BMJ 2023;382:p2030.
More people with acute respiratory infections could be treated outside hospitals in respiratory hubs or virtual wards this winter, advises new guidance from the UK National Institute for Health and Care Excellence.1
NHS England has prioritised the expansion of virtual ward capacity as a way to relieve pressure on hospitals,2 but health leaders have warned that staffing gaps could put the initiative at risk.3
The draft guideline, open for consultation until 15 September, covers the diagnosis and management of suspected acute respiratory infections, including pneumonia, influenza, and respiratory viruses, but not covid-19. It follows recent NICE guidance recommending the use of virtual wards and digital technology to monitor patients aged over 16 with acute respiratory infections.
(31). Govind Warrier et al. How Can Palliative Care Help Me? JAMA Intern Med. 2023.
What Is Palliative Care?
Palliative care is specialized medical care for people living with a serious illness. It focuses on providing relief from the symptoms and stress of the illness. The goal of palliative care is to improve quality of life for a patient and their family. Palliative care is provided by a specially trained team of doctors, nurses, and other specialists who work together with a patient’s other doctors to provide extra support. Palliative care is based on the needs of the patient, not on how long someone is expected to live. It is appropriate at any age and any stage of serious illness, and it can be provided alongside treatment for illness. Palliative care is not the same as hospice care. Hospice care is also focused on helping patients and their families feel better, but is specifically for patients who are in the last months of life.
Who Benefits From Palliative Care?
Palliative care can benefit people with any serious illness that affects quality of life. Some examples include people with cancer experiencing pain, nausea, or weight loss; people with lung disease or heart disease who feel short of breath; people with worsening neurologic diseases such as Alzheimer disease or Parkinson disease; or people experiencing difficulty with physical or cognitive functioning from any disease. Palliative care can also assist families and caregivers of people living with serious illness. Studies have shown that palliative care can substantially improve quality of life, symptoms, and satisfaction with care.
What Are the Benefits of Palliative Care?
Palliative care can improve your quality of life while getting treatment for a serious illness. Palliative care teams offer expert management of physical and emotional symptoms, including pain, depression, anxiety, fatigue, shortness of breath, constipation, loss of appetite, and difficulty sleeping.
Palliative care teams focus on what matters most to you in life. Palliative care teams help you clarify your goals, such as relief of pain or maintaining independence. They ensure that these values are communicated to your medical professionals so any treatments are in line with your goals.
Palliative care teams can help you make informed decisions. Treating serious illness often involves making difficult choices that affect your life and well-being in different ways. Palliative care physicians understand the risks and benefits of a treatment or exploring what would be most important toward the end of life.
Palliative care focuses on the whole person. Palliative care addresses a person’s physical needs and also places importance on the psychological, emotional, spiritual, cultural, and existential aspects of care.
When Is the Right Time to Consider Palliative Care?
Palliative care can be helpful at any stage of a serious illness. Patients are likely to benefit most when they connect with palliative care teams early in the course of a serious illness.
How Can I Access Palliative Care?
If you believe that you or a loved one would benefit from seeing a palliative care specialist, speak to your health care professional. They can likely refer you to a palliative care specialist in your area.
(31). Richard Smith. The two simple and very human reasons why all health systems, are bound to fail. BMJ 2023;382:p2080.
The two factors that make health systems unsustainable are both deeply human.
The first is the urge to care for the sick. Imagine a paediatrician confronted with an obese child and a child with meningitis. The paediatrician will inevitably concentrate on the child with meningitis who may well die without immediate care. Whole health systems do the same: they prioritise the sick. They are sickness not health systems. Similarly, those in pain and dying want care. This is deeply understandable, and resources flow to the sickness system despite health (sickness) systems accounting for 10-20% of health. Spend on the NHS has increased by 40% since 2010, whereas funding for factors more important for health as opposed to sicknesseducation, housing, transport, benefits, the environment, public health, and much morehas been cut. For example, funding per school pupil is lower today than it was in 2010 and funding of Sure Start, which strong evidence shows is beneficial for the health of the very young, has been cut by 50%. The NHS is now 44% of public expenditure, crowding out, as economists say, other programmes.
The result is an increasingly unhealthy population, which needs care from the health (sickness) system.
The second human factor is the urge to do more for the sick, to develop new tests and treatments, to cure incurable diseases. The main factor driving health (sickness) costs rising ahead of general inflation, which is seen in all health systems, is not ageing of the population, but the fact that there are more health professionals able to do much more. Ageing, of course, interacts with the capacity to do more as age is the main cause of needing those treatments. For example, despite a huge global effort to cure cancer, much of it successful at keeping people with cancer alive for longer, we have more cancer than everbecause our ageing bodies are programmed to develop cancer. The selfish gene has no interest in those past reproductive age. We have treatments that cost tens of thousands a year to keep some people with cancer alive for some months or even years longer than without the treatment, and naturally people want the treatments and doctors want to prescribe them.
Since 1948, when the NHS began the number of drugs in the formulary has increased from 240 to over 18 000, and the number of hospital consultants in England and Wales has increased from 3488 consultants in 1949 to 46 297 in 2018 in Englanda 13-fold increase while the population grew by 30%. Those consultants are all extremely busy and unable to keep up with demand (a word I don’t like in this context). This is a phenomenon known, by economists, as supply-led demand.
In short, two simple human factors make health (sickness) systems unsustainable: more sick people and more health professionals able to do more for them.
Breaking out of this cycle will not be easy, but I’ve floated some ideas that revolve around devising a system that starts with health rather than sickness.2
References
Balls K. Conservative wipeout could bring a hard Frost. The Times 2023; June 29. https://www.thetimes.co.uk/article/conservative-wipeout-could-bring-a-hard-frost-chmzkrtfl
Smith R. From Realistic Medicine to Realistic Health. BMJ2023;381:989. doi:10.1136/bmj.p989. pmid:37116941CrossRefPubMedGoogle Scholar
(32). Sixty seconds on turmeric. BMJ, 2023;382:p2070.
What’s cooking?
A study1 has suggested that a natural compound found in the culinary spice turmeric could be as effective as the proton pump inhibitor omeprazole for treating symptoms of indigestion.
A recipe for success?
Potentially. Derived from the root of the Curcuma longa plant, turmeric contains curcumin, a naturally active compound thought to have anti-inflammatory and antimicrobial properties. It has long been used as a medicinal remedy in South East Asia.
(33). If you won’t speak up, how will the world know you exist? BMJ 2023;382:p2051
The leadership journey for me started pretty early in my careeras a trainee, in factbefore I moved on to a clinical director role within a year of my appointment. When I worked in local leadership roles, I sometimes wondered why national leaders rarely spoke out on things that clearly weren’t helping patient care. In this regard, my time in a national role over the past seven and a half years has been fascinating. I’ve been able to observe first hand why people in positions of power in the NHS so often choose not to speak up. In my experience there are about five main reasons.
Keeping the job
Many people think that raising their head above the parapet could compromise their position and their career, and they’ll lose their power to influence change. From personal experience, that’s mostly nonsense. I’ve found that a clear, loud voice centred on consistent values brings you more allies in the system, not fewer. The root of the concern here is, essentially, What would I do if I lost my job?in terms of paying bills and a mortgage, as well as losing the sense of power a title can bring.
Fear
Mixed in with the above is the genuine fear of feeling threatened. The threat of being pursued by HR, the threat of being walked out of your job, the associated loss of finances. The recent Letby case has raised queries around Why didn’t doctors do more? Threats have their way of silencing: look at the way regulatory bodies such as the GMC are used by some individuals to harm careers, or how the GMC acts in those situations.1
The bigger picture
Everyone talks about the bigger picture, yet no one knows what it is. The idea that you should keep the bigger picture in mind, rather than speaking up, is rampant. However, if you look at the progress of the NHS in recent years nothing suggests that things have improved by compromising on some smaller pictures, whatever that might mean. In private, many leaders will vouch for their commitment to a particular issue, such as primary care or tackling discrimination. But when it comes to it, few of them say much about it in meetings. The belief is that if I stay in the tent, it will be bettereven though it rarely is.
I’ll be rewarded
I’m intrigued by the idea that if I don’t speak up, I shall be bestowed with finances, positions, or something else to help the greater good. Maybe that does help at a personal level. At a system level, not so much. There’s a belief that being corporate means collaborating. The problem is that we confuse collaboration with collusion. The net result is that there’s not much benefit for patients. A gong may look lush on the mantelpiece but, beyond your personal glory, it hasn’t really helped anyone.
I believe this because it’s true
Finally, some people genuinely believe that their silence is warranted because the statement under discussion is simply true. This could apply to a whole range of issues: better pay for doctors (They get paid enough), more support for primary care (They don’t work efficiently enough), more specialist posts (We’ll train others to do their jobdoctors’ training is long and expensive), or tackling racism (It’s politically correct nonsense). If any of those reasons translates into poor care for patients or staff, you don’t need to go looking for the reasons behind ityou’re one of the reasons. As the saying goes, If you’re not going to speak up, how is the world supposed to know you exist?
Personally, I believe that everybody should speak up, or at the very least the NHS must find ways to let people do so. At the moment it doesn’t, no matter how many freedom to speak up people are appointed. Has my style hampered me personally, in delivering outcomes or getting funds? Not at all. Continuing my full time job as a clinician in the NHS stops anyone from threatening me within national roles: it takes away the financial insecurity that might come as leverage for those who want to threaten, and it also gives far more credence to a national role when you work in the trenches. Having data, science, allies, and an active patient community behind me strengthens my resolve to ignore the politics and narrowmindedness and achieve what’s needed.
A common refrain I hear privately is how much I’m admired for my bravery or uniqueness. But this uniqueness arises from others shying away from doing the very thing they profess to admire. If people did it, it would be the norm, and healthcare would be in a much better place.
I’m aware that my ability to speak up is linked with my privileges, yet so many others have the same advantages and don’t use them as they could. I’d encourage future leaders to incorporate data, science, allies, and patients into your thinking, and I promise that you’ll deliver. Most importantly, you can do so without selling your soul or compromising your valuesas long as you have them in the first place.
(34) John Launer. Living with uncertainty. BMJ 2023;382:p2052
I was recently invited to talk to a group of GP registrars about uncertainty in medicine. I resisted making a joke about not being sure if I was the right person to do it. However, once the session started I realised that I was pitching it wrongly for doctors with their level of experience.
I’d hoped to talk about what you might call existential uncertainty: how solid medical facts so often melt into thin air, how the practice of medicine seems with experience to be like a project of trial and error. Uncertainty, I’ve written elsewhere, doesn’t come occasionally, singly, or in isolated categories. It’s the ocean in which we swim for most of our working lives.1 The young doctors present were clearly expecting something more concrete and pragmatic. This included answers to questions such as, What do you say to a parent when you’re not sure if their child’s rash is chickenpox or scabies?
Between us we managed to find a middle ground. I hope that I helped those doctors to feel more comfortable about sharing momentary uncertainty with patients in a transparent way. At the same time I managed to touch on some wider philosophical issues to prepare them for the inevitable experience of finding out just how much of what we believe and do turns out to be questionable in the long run.
Sooner or later, all young doctors will all make diagnoses that turn out to be plain wrong: the viral cough that was a pulmonary embolus, the cognitive decline that was due to deafness, the accidental injury that resulted from domestic abuse, or the depressed child who recovered when she moved to a school where she wasn’t bullied. Their misjudgments will come in other forms toomost especially by speaking when they should have listened or giving advice when none was wanted.
Then there are certainties we hold collectively as a profession, which we’ll dismiss as poppycock in a decade or two. Like their predecessors this generation will see some conditions, treatments, and explanations be challenged and then disappear, while others will be summoned into existence in their place. (The idea that bacteria could cause peptic ulcers, for example, was totally unimaginable when I studied medicine.) Some solid truths such as broken bones and strokes may remain, although their treatment will probably change. But the way we understand other conditions will continually evolve. This will result from scientific and technological advances such as genomics and artificial intelligence, but culture and politics will also play a part.
Should we introduce trainees and medical students to the idea of existential uncertainty earlier in their careers? Some teachers might argue that we all need to focus on knowledge first and scepticism afterwards. I’m not so sure. Perhaps it would be better to warn our learners from the beginning that many of their certainties will seem like wishful confabulations over time. It might make the overconfident ones more tentative, and the thoughtful ones might be more secure in their legitimate doubts.
(35). Helen Salisbury. The weight of emotions. BMJ 2023;382:p2071.
Patients bring many things with them to the consulting room. Some we’re expecting, including their symptoms, thoughts, worries, and expectations; some are unexpected but a nice surprisechocolates and biscuits, homemade jam, allotment producewhile others are less welcome. These include evidence of illness presented in a nappy or handkerchief, and occasional parasites that remain after the patient has departed (we had a recent problem with bedbugs, resulting in a stressed and itchy nurse and a clinical room out of action as it awaits a deep clean).
Patients also bring their grief, anger, frustration, and fear or sense of loss in varying measures. Some have spent a long time ricocheting around our dysfunctional health and care system, and for them we try to provide a calm place and a plan, or at the very least a space where they feel heard. I’m aware of my own privilege and good fortune as I listen to complex histories of domestic violence, alcohol misuse, or just the ordinary misery of pain, stress, financial hardship, or relationship breakdowns.
But what do we do with all the things patients bring to us? The biscuits belong by the kettle, and the excreta in the clinical waste bin, but the emotional load isn’t so easily laid down. We try to tease out the areas where we can offer something practicaladvice, medicines, referralsbut we’re often left with a tangle of emotions and a sense of our own impotence in the face of a sad and unfair world. Not all patients will affect us equally, and some cases will strike a particular chord because an experience chimes in some way with our own, or because we’ve looked after a patient for many years and know not just them but their whole family.
In other professions that involve listening to people in distress, such as psychotherapy and counselling, supervision is mandatory. In those sessions the practitioner discusses both how they’re handling a case and the impact it’s having on them. Doctors, on the other hand, are generally expected just to get on with it, which can be lonely. Our specialist trainees have weekly tutorials that offer opportunities for unburdening, and some of them benefit from mentoring and peer support through the New to Practice fellowship scheme when they qualify.
But after these early years it can be a matter of luck: if you’re fortunate enough to work in a practice that has a close team and enough time to draw breath, coffee breaks may provide space for sharing and supportalthough this also requires adequate privacy and the confidence that no one is judging you. However, since many doctors will prioritise eating or going to the loo in the few minutes they have to spare in the working day, I suspect that many go home still carrying the weight of other people’s emotions, burdened by worries about their patients’ safety, and wondering if they could or should have done more.
(36). Scientists discover how brain cells die in Alzheimer’s. https://www.bbc.com/news/health-66816268
Scientists in the UK and Belgium think they have figured out how brain cells die in Alzheimer’s disease.
It has been a mystery and a source of scientific debate for decades.
But the team, writing in the journal Science, connect the abnormal proteins that build up in the brain with necroptosis – a form of cellular suicide.
The findings have been described as cool and exciting, as they give new ideas for treating the disease.
Long-awaited clues
It is the loss of brain cells, called neurons, that lead to the symptoms of Alzheimer’s, including memory loss.
And if you look inside the brains of people with the disease you’d see the build-up of abnormal proteins called amyloid and tau.
But scientists have not been able to join the dots between these key traits of the disease.
This is what the researchers – at the UK’s Dementia Research Institute at University College London and KU Leuven in Belgium – now think is happening.
They say abnormal amyloid starts to build up in the spaces between neurons, leading to brain inflammation, which the neurons do not like. This starts to change their internal chemistry.
Tangles of tau appear and the brain cells start producing a specific molecule (it’s called MEG3) that triggers death by necroptosis. Necroptosis is one of the methods our bodies normally use to purge unwanted cells as fresh ones are made.
The brain cells survived when the team were able to block MEG3.
This is a very important and interesting finding, researcher Prof Bart De Strooper, from the UK’s Dementia Research Institute, told the BBC.
For the first time we get a clue to how and why neurons die in Alzheimer’s disease. There’s been a lot of speculation for 30-40 years, but nobody has been able to pinpoint the mechanisms.
It really provides strong evidence it’s this specific suicide pathway.
The answers came from experiments where human brain cells were transplanted into the brains of genetically modified mice. The animals were programmed to produce large quantities of abnormal amyloid.
There has been recent success in developing drugs that strip amyloid out of the brain and they mark the first treatments to slow the destruction of brain cells.
New drugs for Alzheimer’s hailed as turning point
I’ve got dementia – dementia hasn’t got me
Fiona Phillips: How common is early Alzheimer’s?
Prof De Strooper says the discovery that blocking the MEG3 molecule can hold off brain cell death could lead to a whole new line of drugs development.
However, this will take years of research.
Prof Tara Spires-Jones, from the University of Edinburgh and the president of the British Neuroscience Association, told me that is a cool paper.
She said it addresses one of the fundamental gaps in Alzheimer’s research these are fascinating results and will be important for the field moving forward.
However, she stressed that many steps are needed before knowing whether it could be harnessed as an effective treatment for Alzheimer’s.
Dr Susan Kohlhaas, from Alzheimer’s Research UK, said the findings were exciting but still at an early stage.
This discovery is important because it points to new mechanisms of cell death in Alzheimer’s disease that we didn’t previously understand and could pave the way for new treatments to slow, or even stop disease progression in the future.
(37). Thomas H Tranah et al. Diagnosis and management of ectopic varices in portal hypertension. 2023.
Ectopic variceal bleeding is a rare cause of gastrointestinal bleeding that can occur in settings of cirrhotic and non-cirrhotic portal hypertension and is characterised by its development at locations remote from the oesophagus and stomach. Ectopic varices can be difficult to identify and access, and, although a relatively uncommon cause of portal hypertensive bleeding, can represent a difficult diagnostic and therapeutic challenge associated with considerable mortality. Low incidence and variance in variceal anatomy preclude large randomised controlled trials, and clinical practice is based on experience from case reports, case series, and specialist centre expertise. Optimisation of survival outcomes relies on understanding a patient’s portal venous anatomy and functional hepatic reserve to guide timely and targeted endoscopic and endovascular interventions to facilitate the rapid control of ectopic variceal bleeding.
(38). Stephane Heymans, et al. Dilated cardiomyopathy: causes, mechanisms, and current and future treatment approaches. 2023.
Dilated cardiomyopathy is conventionally defined as the presence of left ventricular or biventricular dilatation or systolic dysfunction in the absence of abnormal loading conditions (eg, primary valve disease) or significant coronary artery disease sufficient to cause ventricular remodelling. This definition has been recognised as overly restrictive, as left ventricular hypokinesis without dilation could be the initial presentation of dilated cardiomyopathy. The causes of dilated cardiomyopathy comprise genetic (primary dilated cardiomyopathy) or acquired factors (secondary dilated cardiomyopathy). Acquired factors include infections, toxins, cancer treatment, endocrinopathies, pregnancy, tachyarrhythmias, and immune-mediated diseases. 5-15% of patients with acquired dilated cardiomyopathy harbour a likely pathogenic or pathogenic gene variant (ie, gene mutation). Therefore, the diagnostic tests and therapeutic approach should always consider both genetic and acquired factors. This Seminar will focus on the current multidimensional diagnostic and therapeutic approach and discuss the underlying pathophysiology that could drive future treatments aiming to repair or replace the existing gene mutation, or target the specific inflammatory, metabolic, or pro-fibrotic drivers of genetic or acquired dilated cardiomyopathy.
(39). Miquel Serra-Burriel, et al. Development, validation, and prognostic evaluation of a risk score for long-term liver-related outcomes in the general population: a multicohort study. 2023.
Background
Liver cirrhosis is a major cause of death worldwide. Cirrhosis develops after a long asymptomatic period of fibrosis progression, with the diagnosis frequently occurring late, when major complications or cancer develop. Few reliable tools exist for timely identification of individuals at risk of cirrhosis to allow for early intervention. We aimed to develop a novel score to identify individuals at risk for future liver-related outcomes.
Methods
We derived the LiverRisk score from an international prospective cohort of individuals from six countries without known liver disease from the general population, who underwent liver fibrosis assessment by transient elastography. The score included age, sex, and six standard laboratory variables. We created four groups: minimal risk, low risk, medium risk, and high risk according to selected cutoff values of the LiverRisk score (6, 10, and 15). The model’s discriminatory accuracy and calibration were externally validated in two prospective cohorts from the general population. Moreover, we ascertained the prognostic value of the score in the prediction of liver-related outcomes in participants without known liver disease with median follow-up of 12 years (UK Biobank cohort).
Findings
We included 14726 participants: 6357 (43.2%) in the derivation cohort, 4370 (29.7%) in the first external validation cohort, and 3999 (27.2%) in the second external validation cohort. The score accurately predicted liver stiffness in the development and external validation cohorts, and was superior to conventional serum biomarkers of fibrosis, as measured by area under the receiver-operating characteristics curve (AUC; 0.83 [95% CI [0.78-0.89]) versus the fibrosis-4 index (FIB-4; 0.68 [0.61-0.75] at 10 kPa). The score was effective in identifying individuals at risk of liver-related mortality, liver-related hospitalisation, and liver cancer, thereby allowing stratification to different risk groups for liver-related outcomes. The hazard ratio for liver-related mortality in the high-risk group was 471 (95% CI 347-641) compared with the minimal risk group, and the overall AUC of the score in predicting 10-year liver-related mortality was 0.90 (0.88-0.91) versus 0.84 (0.82-0.86) for FIB-4.
Interpretation
The LiverRisk score, based on simple parameters, predicted liver fibrosis and future development of liver-related outcomes in the general population. The score might allow for stratification of individuals according to liver risk and thus guide preventive care.
(40). Charles B Majoie, et al. Value of intravenous thrombolysis in endovascular treatment for large-vessel anterior circulation stroke: individual participant data meta-analysis of six randomised trials. 2023.
Background
Intravenous thrombolysis is recommended before endovascular treatment, but its value has been questioned in patients who are admitted directly to centres capable of endovascular treatment. Existing randomised controlled trials have indicated non-inferiority of endovascular treatment alone or have been statistically inconclusive. We formed the Improving Reperfusion Strategies in Acute Ischaemic Stroke collaboration to assess non-inferiority of endovascular treatment alone versus intravenous thrombolysis plus endovascular treatment.
Methods
We conducted a systematic review and individual participant data meta-analysis to establish non-inferiority of endovascular treatment alone versus intravenous thrombolysis plus endovascular treatment. We searched PubMed and MEDLINE with the terms stroke, endovascular treatment, intravenous thrombolysis, and synonyms for articles published from database inception to March 9, 2023. We included randomised controlled trials on the topic of interest, without language restrictions. Authors of the identified trials agreed to take part, and individual participant data were provided by the principal investigators of the respective trials and collated centrally by the collaborators. Our primary outcome was the 90-day modified Rankin Scale (mRS) score. Non-inferiority of endovascular treatment alone was assessed using a lower boundary of 0.82 for the 95% CI around the adjusted common odds ratio (acOR) for shift towards improved outcome (analogous to 5% absolute difference in functional independence) with ordinal regression. We used mixed-effects models for all analyses. This study is registered with PROSPERO, CRD42023411986.
Findings
We identified 1081 studies, and six studies (n=2313; 1153 participants randomly assigned to receive endovascular treatment alone and 1160 randomly assigned to receive intravenous thrombolysis and endovascular treatment) were eligible for analysis. The risk of bias of the included studies was low to moderate. Variability between studies was small, and mainly related to the choice and dose of the thrombolytic drug and country of execution. The median mRS score at 90 days was 3 (IQR 1-5) for participants who received endovascular treatment alone and 2 (1-4) for participants who received intravenous thrombolysis plus endovascular treatment (acOR 0.89, 95% CI 0.76-1.04). Any intracranial haemorrhage (0.82, 0.68-0.99) occurred less frequently with endovascular treatment alone than with intravenous thrombolysis plus endovascular treatment. Symptomatic intracranial haemorrhage and mortality rates did not differ significantly.
Interpretation
We did not establish non-inferiority of endovascular treatment alone compared with intravenous thrombolysis plus endovascular treatment in patients presenting directly at endovascular treatment centres. Further research could focus on cost-effectiveness analysis and on individualised decisions when patient characteristics, medication shortages, or delays are expected to offset a potential benefit of administering intravenous thrombolysis before endovascular treatment.
(41). Graeme J Hankey. Does thrombolysis add value to thrombectomy for acute ischaemic stroke? Lancet 2023;402(10406):P938-939.
The first reperfusion therapy shown to improve the outcomes of patients with acute ischaemic stroke, and become standard medical care, was intravenous thrombolysis with alteplase administered within 4.5 h of symptom onset. The second reperfusion therapy to improve outcomes in patients with proximal anterior circulation artery occlusion compared with standard care was endovascular treatment with thrombectomy within 12 h of stroke onset. Most participants in the randomised controlled trials (RCTs) of endovascular treatment with thrombectomy versus control (ie, no endovascular thrombectomy) received alteplase as part of background standard care, but 15% of participants did not receive alteplase due to ineligibility. 2Subgroup analyses showed no heterogeneity of the effect of thrombectomy in those who received, and did not receive, alteplase (pinteraction=0.43). 2 These analyses resulted in the hypothesis that alteplase might not add value when administered before thrombectomy.
(41). Quentin Richier et al. Pulmonary Aspergilloma. N Engl J Med. 2023;389:1132.
A 51-year-old man from the Democratic Republic of Congo presented to the emergency department with a 1-week history of small-volume hemoptysis. Sixteen months before presentation, computed tomography (CT) of the chest had shown a right upper lung cavitation that was a sequela of treated pulmonary tuberculosis (Panel A). At the current presentation, physical examination was notable for reduced breath sounds at the apex of the right lung. A repeat CT of the chest showed thickening of the wall of the right upper lung cavitation and a new intracavitary mass (Panel B)
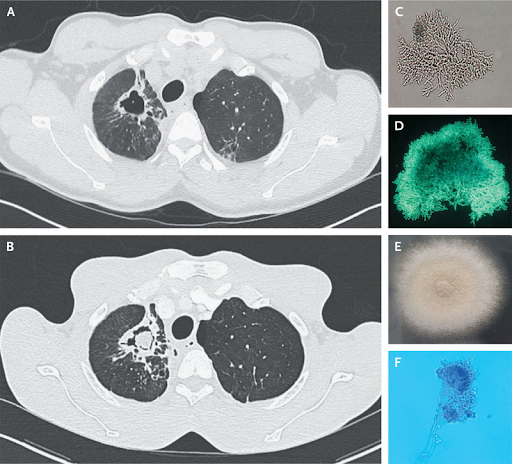
A serum sample was positive for aspergillus-specific IgG antibodies and negative for human immunodeficiency virus antibodies. A diagnosis of pulmonary aspergilloma was made. Sputum samples had been collected to identify the fungus species, test for antifungal susceptibility, and assess for concurrent tuberculosis, which was ruled out. Septate hyphae branching at acute angles were seen on microscopy (Panel C, no stain; and Panel D, fluorescent stain). A sputum culture grew a smoky-gray fungal colony (Panel E) containing uniseriate conidiophores (Panel F). Aspergillus fumigatus was identified by means of mass spectrometry. Treatment with voriconazole was initiated. The patient was lost to follow-up before plans for a lobectomy could be made. Fourteen months later, he presented with massive hemoptysis and underwent pulmonary-artery embolization.
(42). Alexis Kassotis et al. Migrating Emboli in Branch Retinal Artery Occlusion. N Engl J Med 2023;389:e24.
A 53-year-old man presented to the emergency department with sudden-onset, painless vision loss in the inferior visual field of the left eye. He had a history of an aortic aneurysm and had recently undergone multiple complex aortic-arch reconstructions. His postoperative course had been complicated by graft thrombosis, for which he had been taking apixaban and aspirin. On ophthalmologic examination, the visual acuity was 20/20 in the right eye and 20/25 in the left eye. An inferior defect was found on visual-field testing of the left eye. A funduscopic examination showed multiple filling defects in the superior division of the central retinal artery in the left eye, a finding consistent with platelet-fibrin emboli (Panel A, arrows). Trace surrounding macular edema without retinal whitening was also present. A diagnosis of branch retinal artery occlusion due to emboli from the aortic-arch graft thrombosis was made. Therapeutic anticoagulation was continued, and the patient’s visual deficit quickly improved. On repeat funduscopy 24 hours after presentation, the previously visualized emboli were absent, presumably as a result of migration (Panel B, arrows). The patient was discharged home and continued to receive therapeutic anticoagulation. At the 2-week follow-up, his visual acuity and findings on visual-field testing and funduscopic examination had normalized.
(43). Zosia Kmietowicz. Endoscopic sleeve gastroplasty can be used to treat obesity, says NICE. BMJ 2023;382:p2240.
Endoscopic sleeve gastroplasty (ESG) can be used as an alternative to bariatric surgery to help people with a body mass index (BMI) over 30 to lose weight, when combined with lifestyle modifications, the National Institute for Health and Care Excellence (NICE) has said in draft guidance.1
The procedure, which is carried out under general anaesthetic, involves folding and stitching together sections of the stomach wall to reduce the size of the stomach by about two third
(44). Adam C Levine et al. A comparison of the NIRUDAK models and WHO algorithm for dehydration assessment in older children and adults with acute diarrhoea: a prospective, observational study. 2023.
Background
Despite the importance of accurate and rapid assessment of hydration status in patients with acute diarrhoea, no validated tools exist to help clinicians assess dehydration severity in older children and adults. The aim of this study is to validate a clinical decision support tool (CDST) and a simplified score for dehydration severity in older children and adults with acute diarrhoea (both developed during the NIRUDAK study) and compare their accuracy and reliability with current WHO guidelines.
Methods
A random sample of patients aged 5 years or older presenting with diarrhoea to the icddr,b Dhaka Hospital in Bangladesh between Jan 30 and Dec 13, 2022 were included in this prospective cohort study. Patients with fewer than three loose stools per day, more than 7 days of symptoms, previous enrolment in the study, or a diagnosis other than acute gastroenteritis were excluded. Patients were weighed on arrival and assessed separately by two nurses using both our novel clinical tools and WHO guidelines. Patients were weighed every 4 h to determine their percent weight change with rehydration, our criterion standard for dehydration. Accuracy for the diagnosis of dehydration category (none, some, or severe) was assessed using the ordinal c-index (ORC). Reliability was assessed by comparing the prediction of severe dehydration from each nurse’s independent assessment using the intraclass correlation coefficient (ICC).
Findings
1580 patients were included in our primary analysis, of whom 921 (58.3%) were female and 659 (41.7%) male. The ORC was 0.74 (95% CI 0.71-0.77) for the CDST, 0.75 (0.71-0.78) for the simplified score, and 0.64 (0.61-0.67) for the WHO guidelines. The ICC was 0.98 (95% CI 0.97-0.98) for the CDST, 0.94 (0.93-0.95) for the simplified score, and 0.56 (0.52-0.60) for the WHO guidelines.
Interpretation
Use of our CDST or simplified score by clinicians could reduce undertreatment and overtreatment of older children and adults with acute diarrhoea, potentially reducing morbidity and mortality for this common disease.

