Lateral medullary syndrome
Nithya P1, Gowsalya P2, Gayathri3, Harish R Kamath4
[1, 2]PG Diploma in Anesthesiology, Kauvery Hospital, Hosur
3Senior Consultant – Anaesthesia, Kauvery Hospital, Hosur
4Consultant Neurologist, Kauvery Hospital, Hosur
Abstract
Lateral medullary syndrome or Wallenberg syndrome is the syndrome that occurs due to thrombosis, emboli, or dissection of the vertebral artery or PICA. It is the most common posterior circulation ischemic stroke. Posterior circulation strokes represent about 20% of all ischemic strokes. A typical patient with this syndrome is an elderly patient with vascular risk factors and the onset is acute. The most common symptoms of onset are dizziness with vertigo, loss of balance with gait instability, hoarseness of voice, and difficulty swallowing. The symptoms often progress over several hours to few days.
We report here two cases of LMS with varied neurological manifestations. First patient is a 42-year-old male with no known risk factors who came with complaints of giddiness, slurring of speech and ataxia over the left side. Another case of a 55-year-old male with DM, CAD not on regular treatment presented with complaints of giddiness, difficulty in speaking, hoarseness of voice, difficulty in swallowing & numbness over the right side of the face. Clinical examination and radiological investigations confirmed the diagnosis of lateral medullary syndrome in both of these patients.
Background
Lateral medullary syndrome is a neurological disorder associated with various symptoms resulting from atherothrombotic occlusion of the vertebral artery or by occlusion of the posterior inferior cerebellar artery. Lateral medullary syndrome is also called Wallenberg syndrome/posterior inferior cerebellar artery syndrome.
Gaspard Vieussex first describes it in 1808 and Adolf Wallenberg gives a detailed clinical description in 1895 who is a renowned Jewish neurologist.
The arteries commonly involved in LMS are the posterior inferior cerebellar artery (PICA) or the vertebral artery. Most cases result from ipsilateral vertebral artery occlusion and sometimes PICA occlusion can occur. Occlusion of the medullary penetrating branches of vertebral or PICA results in partial syndromes.
The constellation of vertigo, numbness of ipsilateral face and contralateral limbs, hoarseness dysarthria, diplopia, dysphagia, nystagmus, ipsilateral ataxia and ipsilateral Horner’s syndrome constitutes lateral medullary syndrome. Ipsilateral upper motor neuron facial weakness can also occur. Hemiparesis is not typical feature of vertebral artery occlusion. The condition shows a predominance for men in their sixth decade. Overall LMS patients have a better prognosis than most other stroke syndromes, even those with severe dysphagia .Most patients return to activities of daily living. The commonest sequel is gait instability.
Case Presentation
Case 1
A 42-year-old male patient presented to ER within three hours of onset of symptoms with the history of giddiness, left sided incoordination, slurring of speech, pain over left shoulder, vomiting and profuse sweating. No h/o headache, diplopia, weakness, loss of sensation in any limb, loss of consciousness, altered sensorium, Patient had no history of Hypertension, DM, IHD, epilepsy in the past.
On Examination
On clinical examination, patient was conscious, oriented, responded to all axial commands with vitals – mildly raised blood pressure right 170/120 mmHg and 160/100 mmHg left side and maintaining saturation in room air. The patient had Skew deviation with left eye hypo ducted, nystagmus +, Pupils -Left 2mm RTL, right 3mm RTL, left impulsion. Left-sided severe incoordination of both upper and lower limbs, Left sided power up to grade 4 to 5 deviation of angle of mouth to the right side and severe dysarthria, palatial movement reduced on left side. Systemic examination of cardiovascular, respiratory, and abdomen is unremarkable. His investigations hematological and biochemical are within normal limits, with lactate 2.6 mmol. ECG showed normal sinus rhythm.
Management
CT brain done, which showed both cerebral hemisphere appears normal the grey and white matter attenuation pattern is normal, subtle hyper dense noted in right MCA. Hence, a clinical diagnosis of posterior circulation stroke was considered and patient was thrombosed with Tenecteplase 18 mg slow IV under closed monitoring. His GCS was E2V3M5; patient was feeling better, vitals stable, severe dysarthria, deviation of angle of mouth to right persisted, left-sided incoordination present, nystagmus improving, skew deviation reduced. T. Betahistine 16 mg and Inj levetiracetam 500mg and anti-hypertensives Nifedipine retard 10 mg and Olmesartan 20mg started.

MRI Brain
MRI brain showed periventricular and subcortical white matter ischemic changes (Fazeks grade 1), acute infarcts seen at left thalamus, temporal & occipital lobe, left cerebellar hemisphere, vermis, left lateral aspect of medulla and right occipital lobe due to left PCA thrombosis. 7th and 8th cranial nerves appear normal USG Carotid Doppler showed normal flow pattern with no demonstrable hemodynamic abnormality in both carotids, flow within right vertebral artery is normal and left vertebral artery is not demonstrable-likely to be hypoplastic. 2D ECHO – concentric LVH, no RWMA, LVEF-60 % good RV function, clinically patients vitals remained stable, he was conscious, oriented, torsional and horizontal jerky nystagmus, hemianopia and incoordination left side persisted. Occasional hiccoughs present. Patient is diagnosed as a case of acute posterior circulation stroke -PCA and PICA territory thrombosis suggestive of embolic etiology. Hence dual antiplatelets – T. Aspirin 150mg, T. Clopidogrel 75mg, Statins and Neuro protective agents were started. The patient improved gradually, he was able to swallow fluids without aspiration and can take semisolid feeds, though nystagmus persisted it was better, finger-nose coordination better, power in limbs improved, touch and pain normal, hoarse voice and occasional hiccoughs persisted and the patient was discharged on 8th day.
Case 2
A 55-year-old male known case DM and CAD on irregular treatment, presented to us with h/o of giddiness, slurring of speech, imbalance to right, hoarseness of voice, difficulty in swallowing, numbness over right side of face and extremities. There is no h/limb weakness, diplopia and facial deviation Personal and family history was unremarkable.
On Examination
On clinical examination, patient was conscious, oriented, vitals-afebrile,
HR of 80/min sinus rhythm with BP -220/120 on Right, 200/100 on Left, and maintained saturation in room air.
On neurological examination – pupils 2mm RTL left beating horizontal jerky with left torsional nystagmus present, which aggravates on left gaze, on right gaze -Left torsional nystagmus.
Palatal movements – minimally reduced on right with, right side facial sensation impaired, right side finger nose incoordination present, Stance-severe ataxia to right, right -lower limb touch impaired, power-grade 5 bilateral.
Diagnosis: Hence clinically diagnosed as a case of acute ischemic stroke – posterior circulation stroke-Right lateral medullary syndrome with accelerated hypertension.
Management
His investigations revealed – normal CBC, biochemistry and GRBS 382 MG/dl, ECG -normal Echo – no RWMA, LVEF 64%, normal RV function, no clots or vegetations CT Brain -early age-related atrophic changes MRI/ MRA brain showed periventricular and sub cortical white matter ischemic changes (FAZEKAS GRADE 1). Hypoplastic posterior communicating artery, tiny R lateral medullary infarct Pt thrombosed with Inj. Tenecteplase 18 MG IV, labetalol infusion started and oral antihypertensive and oral hypoglycemic agents, dualantiplatelets, statins, antibiotic and neuroprotective agent were started. In next few days he became drowsy, arousable and was obeying all axial commands, Right side ptosis with miosis, right eye hypo ducted, reduced right palatal movements, phonation reduced but was able to articulate and had hiccoughs, He developed hypotension, CO2 retention and type2. resp failure when he went to sleep.
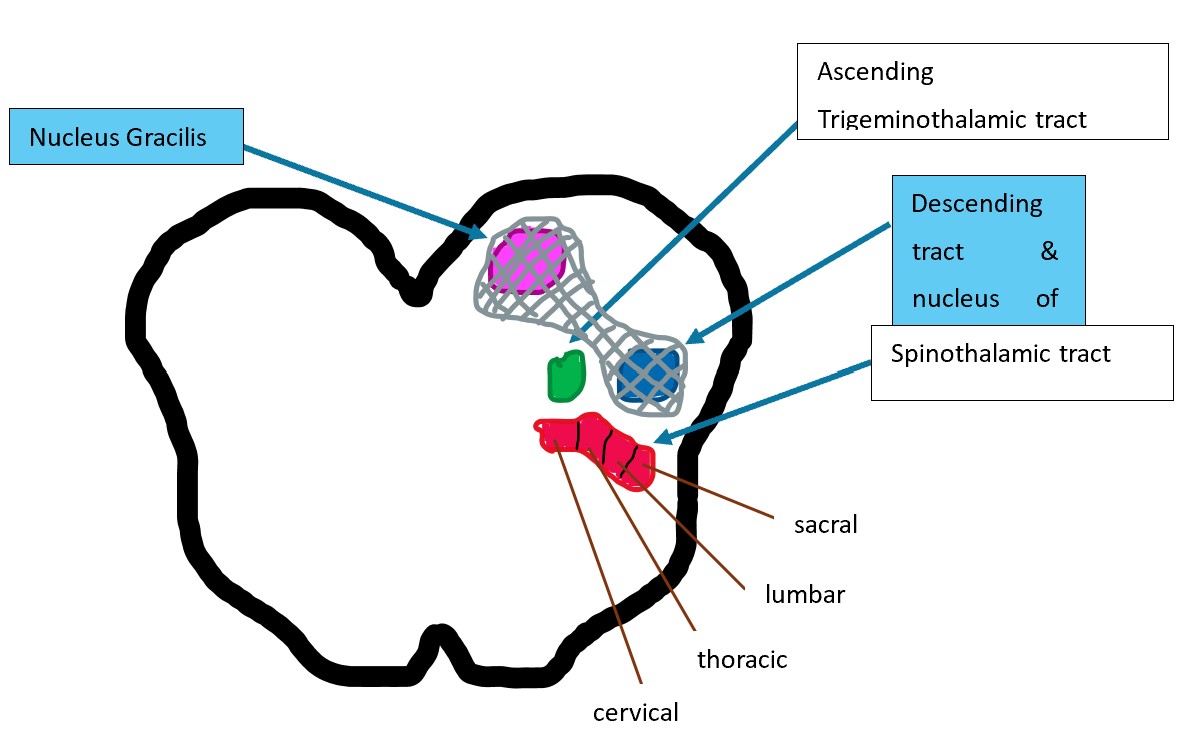
Possibility of acquired Ondine’s curse was considered and hence he was ventilated non-invasively. He was then started on Ryle’s tube feeing and other supports, CT brain repeated which was normal. Patient was intubated due to low GCS, hypoxia and Resp acidosis and connected to mechanical ventilation and ventilated overnight and morning patient was conscious E4VTM6, obeying commands, tone of extremities improved but had ataxic breathing pattern when alert and poor breathing effort when sleeping. Trial weaning failed hence planned for tracheostomy but patient’s attenders were not willing for further management and hence patient was discharged against medical advice. This case is presented for its rarity. This is an unusual pattern of lateral medullary infarct as far as clinical features are concerned. Apart from the usual structures involved in lateral medullary infarct, here the descending tract/nucleus of the trigeminal nerve is involved along with the gracile nucleus located in the lower medulla (carrying the fine touch perception from ipsilateral lower body) in addition to the descending medullo cervical pathway subserving the automatic breathing (which is located in the ventrolateral aspect of the inferior medulla). The authors want to highlight the importance of clinical localization here. An ipsilateral tactile or proprioception impairment in a case of lateral medullary syndrome (which may be missed without a thorough clinical examination) can help us to localize the extension of lateral medullary lesion inferiorly in medulla. A high index of suspicion of involvement of the automatic breathing Centre can hence be kept in all such cases.
Discussion
Anatomy
PICA plays an important role in the blood supply of the cerebellum, and the PICA territory is the most common area of cerebellar ischemic stroke of, accounting for 40%. The vertebral arteries originate from the innominate artery on the right and the subclavian artery on the left, and the two VAs converge to form the BA at the lower margin of the junction of the medulla oblongata and the pons. It is classically divided into four segments. The fourth segment gives off the branches that supply the brain stem and cerebellum. Atherothrombotic lesions have a predilection for V1 and V4 segments of the vertebral artery. The first segment may become diseased at the origin of the vessel and may produce posterior circulation emboli. Disease of the distal fourth segment of the vertebral artery can promote thrombus formation. Stenosis proximal to the origin of PICA can threaten lateral medulla and posterior inferior surface of the cerebellum. PICA is the largest branch of the vertebral artery and has no alternative collateral circulation .
The trunk of PICA is divided into five segments:
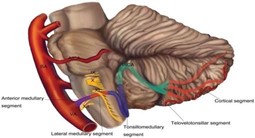
The anterior medullary segment begins at the origin of the PICA. The lateral medullary segment extends from the level of the most prominent point of the olive to the level of the origin of the glossopharyngeal (CN IX), vagus (CN X), and accessory (CN XI) rootlets. The tonsillomedullary segment begins where the PICA passes posterior to the CN IX-XI and ends at the midpoint of the PICA’s ascent toward the roof of the fourth ventricle along the medial surface of the tonsil The telovelotonsillar segment and the cortical segment. The trunk of PICA gives rise to perforating, choroidal, and cortical branches. The PICA supplies the medulla, the choroid plexus, the tela choroidea of the fourth ventricle, the tonsils, the inferior vermis, and the inferior aspects of the cerebellar hemispheres.
Etiology
LMS is commonly caused by atherothrombotic occlusion of the vertebral artery, followed by occlusion of the posterior inferior cerebellar artery and the medullary arteries. The PICA is of great clinical importance with its unique anatomical complexity and is involved in many diseases, including ischemic stroke, aneurysm, neurovascular compression syndrome (NVCS), arteriovenous malformation (AVM), brain tumor, etc. PICA infarction is more likely to cause mass effects compared with other vessels. Besides, the PICA is exposed in many surgical approaches and is vulnerable to damage. Hypertension is the most prevalent risk factor, followed by smoking and diabetes. Young patient presenting with migraine and signs and symptoms of the LMS -vertebral artery dissection and aneurysm to be considered. Cardiogenic embolism due to atrial fibrillation, mechanical prosthetic valves, left atrial or ventricular thrombus, dilated cardiomyopathy, myocardial infarction, and infective endocarditis. Embolism can also occur in cocaine misuse, neck manipulation, medullary neoplasms, radionecrosis, hematoma. Small vessel disease Hypoplastic Vertebral artery Vertebrobasilar dolichoectasia: Patients may present with vertebrobasilar territory ischemia. Risk factors for vertebrobasilar dolichoectasia include male gender, hypertension, smoking, and previous myocardial infarction. It has correlations with aortic dilations, ectatic coronary arteries, Marfan syndrome, and the autosomal dominant polycystic kidney disease. Other less common causes include subclavian steal syndrome, Fabry disease, mitochondrial encephalopathy, lactic acidosis, and migraine Large artery atherothrombotic causes account for about 75% of the cases, followed by cardio embolism in 17% and vertebral dissection in 8%.
Pathophysiology
LMS is the most prevalent posterior circulation ischemic stroke syndrome and has the typical presentation of PICA territory infarcts. The primary pathology is occlusion of the posterior inferior cerebellar artery (PICA) or one of its branches. In most (80%) cases primary pathology is caused by occlusion of the vertebral artery. The most common mechanism of occlusion of the vertebral artery or PICA is atherothrombosis. in which atheromatous plaques narrow and occlude large vessels.
Small vessels are affected by lipohyalinosis, which is closely associated with hypertension. Ischemic infarctions of these small vessels lead to small round infarctions called lacunae, which are scattered throughout the brainstem.
Clinical manifestations
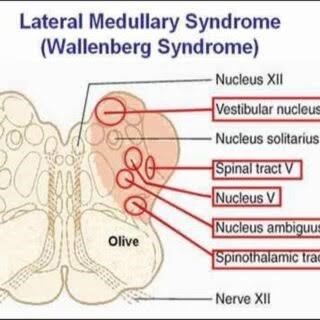
The clinical manifestations of LMS varies and depends on the exact location of the damage. Different combinations of the following deficits may be elicited in
On the side of the lesion
- Vertigo with nystagmus, nausea and vomiting appear due to inferior vestibular nucleus and vestibular-cerebellar connections involvement. nystagmus is typically central, beating to the direction of gaze. Nausea and vomiting, and sometimes hiccups, are associated with vertigo. Hiccups can often be intractable.
- Dysphagia, dysphonia and dysarthria, sometimes combined with ipsilateral loss of gag reflex ascribe to defect of nucleus ambiguus, glossopharyngeal and vagus nerve, which is more significant in LMS patients.
- Ipsilateral ataxia is correlated with cerebellar peduncles, spinocerebellar fibers and inferior cerebellar hemisphere.
- Ipsilateral Horner syndrome due to sympathetic fibers defects.
- Impairment of pain and thermal sensation on the ipsilateral face and on the contralateral trunk and limbs are associated with impaired nucleus spinalis nervi trigemini or its spinal tracts, and spinothalamic tracts respectively.
- Pain and numbness with impaired facial sensation on the face (descending trigeminal tract) -Impaired taste sensation (involvement of nucleus tractus solitarius).
- -Cerebellar infarction can lead to respiratory arrest and hemodynamic instability due to brain stem herniation.
- -Drowsiness, Babinski signs, dysarthria and bifacial weakness may be absent or present only briefly before respiratory arrest ensues. Gait, unsteadiness, headache, dizziness, nausea and vomiting may be the only early symptoms and signs and should arose suspicion of this impending complication, which may require, neurological decompression often with an excellent outcome. Also, there may be an absence of taste sensation, decreased gag reflex, and dysphagia.
Different combination of these symptoms can be found in LMS patients while more than 90% of the patients have sensory symptoms, which are the most frequent manifestations. These symptoms can appear either acutely or gradually, progressing over several hours to several days.
On the contralateral side
Usually, no weakness is associated with this syndrome (corticospinal fibers are ventral in location)
Most common pattern of sensory involvement in lateral medullary syndrome
Ipsilateral face and contralateral body is affected

Contralateral face and contralateral body sensory loss
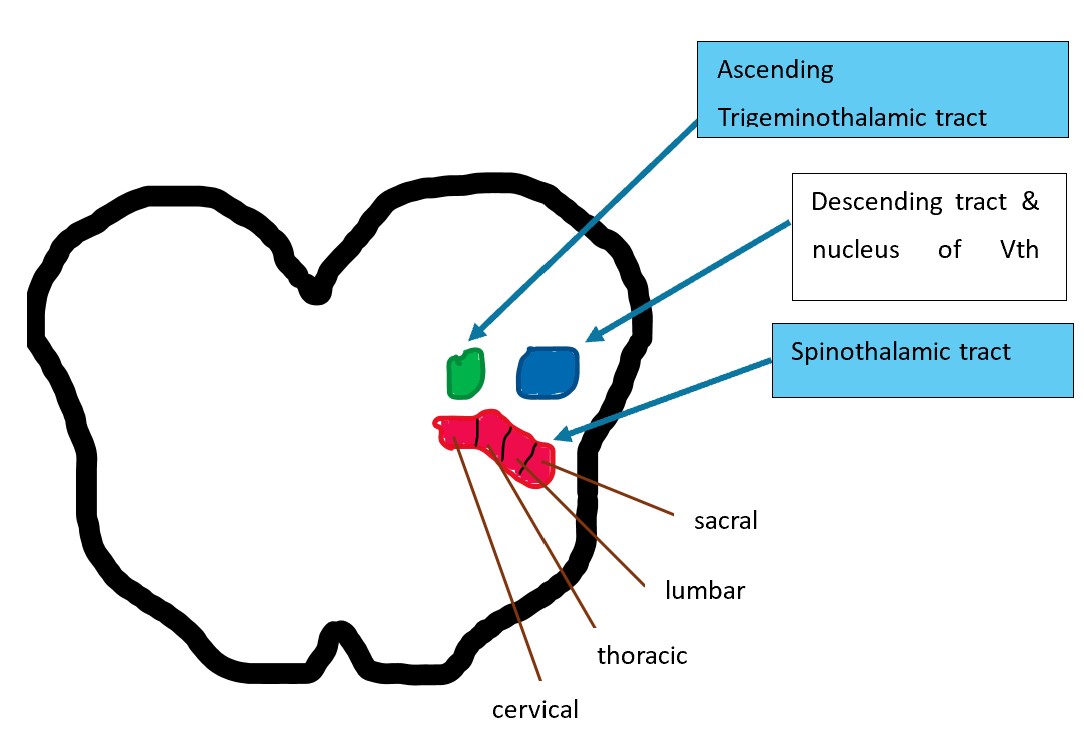
However, in our case ipsilateral facial sensation and ipsilateral lower part of body tactile sensation was affected
| Anatomical location | Presenting Symptoms |
|---|---|
| Spinothalamic tract | Contralateral loss of pain and temperature sensation |
| Spinal trigeminal nucleus | Ipsilateral facial loss of pain and temparature |
| Nucleus ambiguus | Supplies vagus and glossopharyngeal nerves; Dsyphagia/Dysphonia/diminished gag reflux |
| Inferior vestibular nucleus | Vertigo/diplopia/nystagmus/vomiting |
| Sympathetic fibress | Ipsilateral Horners syndrome |
| Central trigemial tract | Palatal clonus |
| Inferior cerebellar peduncleus | Ataxia |
Diagnosis
The diagnosis and treatment is similar to any ischemic stroke. A careful neurological examination is the key to the diagnosis. The critical points in clinical diagnosis are a combination of crossed hemiparesis or hemianesthesia to indicate a brainstem lesion and the involvement of structures in the posterolateral medulla to localize, wherein the brainstem. MRI with diffusion-weighted imaging (DWI) is the best diagnostic test to confirm the infarct in the inferior cerebellar area or lateral medulla.. Up to 30% of patients with non-disabling stroke do not have a lesion on the DWI-MRI brain. These patients are DWI-negative stroke patients, and secondary prevention should be initiated to prevent future strokes. A CT or MR angiogram helps identify the site of vascular occlusion and rule out uncommon causes such as vertebral artery dissection.
Treatment
Treatment aims to reduce the size of the infarction and prevent complications with the final goal of improving patient outcomes .The most common complications of posterior circulation strokes are aspiration pneumonia, deep vein thrombosis, pulmonary embolism, and myocardial infarction. Both intravenous and selective intra-arterial rt-PA may take effect in PICA occlusion.
Intravenous (IV) thrombolysis with IV tissue plasminogen activator (TPA) within 3 to 4 1/2 hours of the onset of the ischemic stroke improves functional stroke outcome by 30%. Endovascular revascularization: indicated mainly for large vessel intracranial occlusion, Oral anticoagulation for cardioembolic strokes. Antiplatelets such as aspirin, clopidogrel, or ASA/dipyridamole for other forms of stroke Statins, Smoking cessation, Antihypertensives – to maintain the cerebral auto regulation Blood sugar: best to keep the patient normoglycemic. DVT prophylaxis -sequential pressure devices /low-dose heparin /low molecular weight heparin (LWMH) Dysphagia management and speech therapy assessment should be included for patients with corresponding symptoms. Early physical therapy and occupational therapy with a good rehabilitation plan.
Secondary stroke prevention to reduce the risk of subsequent stroke by 80%. The condition is managed using traditional stroke rehabilitation protocols, individualized to each patient. In many cases speech, language, and swallowing therapy is beneficial, physiotherapy improves balance, coordination, and movement deficits associated with this order. The use of electrical stimulation to facilitate motor recovery should be incorporated early in the rehabilitation program since it improves muscle strength and balance.
References
- Lui F, Tadi P, Anilkumar AC. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 25, 2023. Wallenberg Syndrome.
- Miao HL, Zhang DY, Wang T, Jiao XT, Jiao LQ. Clinical Importance of the Posterior Inferior Cerebellar Artery: A Review of the Literature. Int J Med Sci. 2020;17(18):3005-3019
- .Saleem F, M Das J. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 7, 2023. Lateral Medullary Syndrome.
- Inamasu J, Nakae S, Kato Y, Hirose Y. Clinical Characteristics of Cerebellar Infarction Due to Arterial Dissection. Asian J Neurosurg. 2018 Oct-Dec; 13(4):995-1000.
- .Ahmed SA, Karataş M, Öcal L, et al. Isolated left ventricular non-compaction cardiomyopathy complicated by acute ischemic stroke: a rare case report. Ann Med Surg 2022; 81:104543.
- Salerno A, Cotter BV, Winters ME. The Use of Tissue Plasminogen Activator in the Treatment of Wallenberg Syndrome Caused by Vertebral Artery Dissection. J Emerg Med. 2017 May;52(5):738-740.
- De Cocker LJ, Lövblad KO, Hendrikse J. MRI of Cerebellar Infarction. Eur Neurol. 2017;77(3-4):137-146.
- Ekechukwu END, Olowoyo P, Nwankwo KO, Olaleye OA, Ogbodo VE, Hamzat TK, Owolabi MO. Pragmatic Solutions for Stroke Recovery and Improved Quality of Life in Low- and Middle-Income Countries-A Systematic Review. Front Neurol. 2020;11:337.

