The Art and Science of Preparation and Publication of Medical Research from Kauvery Hospitals
Dr. Venkita S. Suresh
Group Medical Director, Kauvery Hospitals, India
Dear colleagues,
Across seven units, we at Kauvery Hospitals offer effective health care economically efficiently, energetically, and enthusiastically.
COVID-19 brought the best out of all of us; we always stayed several steps ahead of the virus and its onslaught and salvaged health and happiness, and secured the future of our patients from its carnage.
Valiant and versatile work was done in service of our patients.
This was exceptional team-work that had only one objective, to keep our patients safe while also keeping our health workers safe.
During the nine months from April to December 2020, Kauvery Hospitals admitted over 7,000 patients of COVID-19, with moderate, severe, or critical disease, and sent 95% of patients safely home.
We also treated well over 100 doctors in the community and sent 98% of them safely home.
Those outcomes owe their genesis to the practice of Evidence-Based Medicine.
That evidence now deserves to be published.
Also, Kauvery Hospitals undertook the entire range of Non-COVID work during this pandemic as health care for compromised patients cannot wait for the convenience of one virus to abate.
That work even deserves greater attention to see the light of the day.
The “KAUVERIAN” has put together a team and service in honour of our busy colleagues, to assist them in processing, presenting, and publishing their work.
The steps of this process are very simple:
- Identify the subject of your study,
- Examine and verify your data,
- Write the skeleton of your study, kindly use the ‘Instruction to authors” to prepare your manuscript,
- Begin your discussion with the team at KAUVERIAN,
- Our team will assist you in further growth and development of the study, including statistical analysis, preparation of tables and graphs, and processing of images,
- Parallel publication in the KAUVERIAN shall be done, if permitted.
Collection and verification of your data are paramount. The Central Support Team of Kauvery Hospitals, coordinated by Mr. Vairamuthu, holds the repository of all our data on HIS and EMR.
The first such paper, written by the primary author, fully supported by the content creating team, appears below this introduction as RESEARCH ARTICLE: COVID-19 in a haemodialysis unit: our experience in the pandemic, and the measures taken
Before I close, let me also catch an old bull by its new horns “Why publish? Why bother?! Why not continue “business as usual?”
Socrates, one of the greatest philosophers the world ever saw, had said “the unexamined life is not worth living”.
To paraphrase that towards our article on the art and science of preparation and publication of medical research, “the unexamined work is not worth doing”!
We wish you all “Happy writing”; there is an author and researcher of great talent inside each of you!
COVID-19 in a haemodialysis unit: Our experience in the pandemic, and the measures taken
Balaji Kirushnan*
Department of Nephrology, Kauvery Hospital, Chennai, Tamilnadu, India
*Correspondence: Email: balajikirushnan@gmail.com
Abstract
Background: Patients on haemodialysis are more susceptible to the novel 2019 corona virus disease (COVID-19). Its complications remain high in the presence of co-morbidities such as CKD. However, there is a relative lack of data on impact of COVID on patients undergoing haemodialysis, and on infection control measures to prevent further spread in the haemodialysis unit. The objective of this study is to describe the clinical features and outcome of patients undergoing haemodialysis at our unit with COVID-19, and the measures taken to prevent further transmission of the infection.
Methods: This is a single-center, descriptive, observational study. There were 189 patients on regular haemodialysis at our dialysis unit at the tertiary care hospital in Chennai, India during the study period of March–October 2020. We included in this study 32 haemodialysis (HD) patients who were diagnosed with COVID-19, confirmed by RT–PCR and CT chest.
Results: 17.9% of patients undergoing haemodialysis were detected to have COVID-19. Among the 32 patients, 22 were males and the median age was 62.9 ± 2.10 years. The most common clinical features reported were fever (78.1%), body pain (56.3%) followed by cough (50%). CT chest showed positive findings in 28 patients – ground glass opacity was present in 18 patients, consolidation in eight patients and crazy-paving pattern was present in two patients. Of the 32 patients, only seven patients required hospitalization. The rest of the patients were managed as outpatients, with telemedicine monitoring of their symptoms. Among them, three patients were discharged, three died due to ARDS and one patient among the non-hospitalized suffered sudden cardiac death at home.
Conclusion: Strict isolation protocols and identification of cases were the keys to the low prevalence of COVID-19 in our unit.
Keywords: Haemodialysis, COVID-19, CT chest, Acute Respiratory Distress Syndrome
Background
The Coronavirus disease (COVID-19) has emerged as a pandemic in 2019 affecting large populations worldwide, becoming a serious public health concern. WHO reported 1,178,475 deaths worldwide in October 2020 [1]. COVID-19 affects all age groups in the population and several studies have demonstrated an association of poor prognosis with age and co-morbid conditions [2–4].
According to the Global Burden of Disease (GBD) study, China and India are two major contributors to Chronic Kidney Disease (CKD) worldwide. CKD has been the 12th leading cause of death in 2017 and has affected 9.1% of the world population [5]. In 2017, 1.2 million deaths were reported due to CKD diagnosis and it has been estimated to increase to an astounding 2.2 million by 2040 and reports suggest that this will continue to rise [6]. Patients with End Stage Renal Disease are predisposed to infectious diseases due to impaired immune system and the co-existence of other morbid conditions [7,8]. Published data has revealed that patients with CKD are more susceptible to pneumonia [9,10].
Quarantine and social distancing strategies have been proposed to contain COVID-19 transmission [11]. However, this is a challenge in haemodialysis patients as they have to undergo haemodialysis multiple times a week at an outreach haemodialysis centre or a hospital. The haemodialysis patients carry a high risk of contracting COVID-19 from asymptomatic SARS-Co-V positive carriers; studies from India and other countries have reported asymptomatic carriers at an incidence of 20–35%, causing concern [12–14]. Dialysis patients need frequent transport, and accompanying attendees, to visit the hospital. Furthermore, the dialysis sessions require interaction with hospital staffs, patients have to remain in a closed environment with reduced ventilation for several hours. These factors are conducive to easy acquiring of COVID-19 infection.
Our main aim of this present study is to describe the clinical presentations and management of haemodialysis patients with COVID-19 infection in our dialysis unit at a tertiary care hospital. We also highlight the importance of strict infection control measures and isolation policies and practises in a haemodialysis unit to prevent spread to other patients.
Methods
Study population
In this retrospective study, we included 32 haemodialysis (HD) patients who were diagnosed with symptomatic COVID-19 at our hospital from March–October 2020 in a tertiary care hospital in Chennai, India. There were 189 haemodialysis patients in our unit during the study period. We did not screen all patients for asymptomatic infection.
Study method
The baseline data of patients include age, sex, presence of co-morbid conditions, the onset of symptoms, frequency of haemodialysis, need for admission to hospital, treatment with steroids and remdesivir, results of CT chest radiograph of SARS-Co-V-2 RNA real-time reverse transcription–polymerase chain reaction (RT–PCR) were collected. Co-morbidities included the history of diabetes mellitus, hypertension, ischaemic heart disease, peripheral vascular disease, obstructive sleep apnoea/chronic obstructive pulmonary disease and stroke syndromes
Statistical analysis
The data was entered in Microsoft Excel 2016 and statistical analysis was performed using the statistical package for social sciences (SPSS) version 27 for Windows. Continuous variables were presented as mean ± standard deviation and categorical variables were presented in number (percentage).
Results
Patient characteristics
The mean age was 62.9 years with the oldest being 82-years-old. We found a higher proportion of males (68.75%) in this study. Among the total of 32 patients, 28 (87.5%) patients were predominantly hypertensive and 22 (68.8%) were diabetic. 9 (28.1%), 3 (9.4%), 4 (12.5%) and 3 (9.4%) had ischaemic heart disease, peripheral vascular disease, Chronic obstructive pulmonary disease and cerebrovascular disease respectively. Table 1 illustrates the clinical characteristics of patients. The most common symptom was fever (78.1%) and body pain (56.3%) followed by cough (50%) (Fig. 1).
Table 1. Baseline Characteristics of haemodialysis patients with COVID-19.
| Patient Characteristics | Total n(%) (n=32) |
| Age | |
| Mean age (years) ± SD | 62.90 ± 2.10 |
| Sex (n%) | |
| Male | 22 (68.75) |
| Co-morbidities | |
| Type 2 Diabetes Mellitus | 22(68.8) |
| Hypertension | 28(87.5) |
| Ischaemic heart disease | 9(28.1) |
| Peripheral vascular disease | 3(9.4) |
| Obstructive sleep apnoea/ Chronic obstructive pulmonary disease | 4(12.5) |
| Cerebrovascular accident | 3(9.4) |
*Data are presented as mean ± standard deviation or n(%)
 Fig. 1. Clinical features of haemodialysis patients with COVID-19.
Fig. 1. Clinical features of haemodialysis patients with COVID-19.
CT Chest findings
Abnormal CT Chest radiograph findings were present in 87.5% of patients and were classified into mild, moderate and severe categories based on COVID-19. Reporting and Data System (CORADS) scoring system. CT Chest findings revealed ground glass opacity in 18 patients, consolidation in eight patients and a crazy-paving pattern in two patients (Table 2).
Table 2. Severity of lung involvement on CT Chest in Haemodialysis patients with COVID-19.
| Classification | Patients (n=32) n(%) |
| Normal | 4(12.5) |
| Mild | 18(56.25) |
| Moderate | 8(25) |
| Severe | 2(6.25) |
Infection control measures and isolation protocols
All patients visiting our haemodialysis unit were thoroughly examined by the medical team in a designated screening area as recommended by the Indian Society of Nephrology. Patients with clinical symptoms suggestive of COVID-19 infection were tested for RT–PCR swab and CT Chest. Patients who are suspicious of COVID-19 infection and who require a CT scan are transported to the CT scan room in a separate stretcher after a green channel was established between the screening area and the CT scan room, and with an N95 mask. All other routine scans were postponed. The CT scan room is then deep-cleansed with Bacillol solution. Confirmed or highly suspected patients (CORADS 4 or 5) were isolated and haemodialysis was performed in designated wards for COVID-19 patients for 14 days. Patients with mildly symptomatic or those with CORADS 1, 2 or 3 by CT scan were allocated to the last shift of the day and were dialyzed in few dedicated machines in one corner of the HD unit for two weeks. If they worsened clinically, a repeat RT–PCR swab was ordered and they were transferred to designated wards (Fig. 2) The Haemodialysis unit was fumigated daily after the last shift. N95 mask was made compulsory for all patients, manager, housekeeping staff and dialysis technicians.
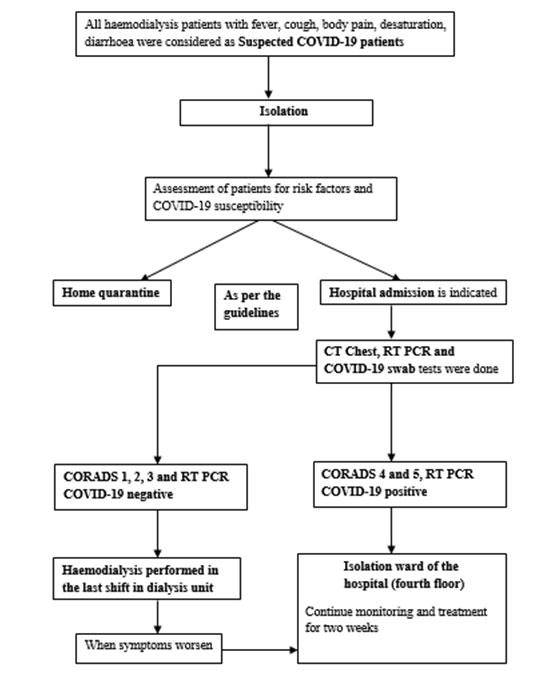
Fig. 2. Identification and management of haemodialysis patients with suspected/confirmed COVID-19 infection. Abbreviation: CORADS – COVID-19 Reporting and Data System (CORADS), COVID-19 – corona virus disease.
The staffs in the dialysis ward wore the disposable gown, gloves, cap, N95 face mask and face shield. The staffs were screened for COVID-19 infection daily and any staffs suspicious for COVID-19 infection were quarantined in the hospital. They were not allowed to go to their hostel or their residence. They were tested for COVID-19 and after completing the quarantine period and confirming negative status, they were assigned to the dialysis unit. Due to manpower shortage, at a time when there were more COVID-19 positive HD patients, COVID-19 positive staffs who were recovering but still in the quarantine period handled COVID-19 positive HD patients in the isolation ward. The staffs were not allowed to dine together and no more than one staff went for a break at one point of time. The staffs were instructed not to use the common canteen as it could serve as a point of spread of COVID-19. All dialysis filters were disposed of as infectious waste after use following a single use dialyzer system.
In this outbreak, we experienced two waves of COVID-19 infection and we followed the same measures for the medical team and patients. Most of the cases, in patients as well as the staff, presented as clusters. The index case was traced and we followed all people in contact. We had contacted the patient’s family members and enquired about their symptoms. They were all isolated and told to report if any symptoms arise.
Outcomes and treatment
Admission criteria
Any patient with fever for more than five days, desaturation (SpO2 < 93%), or hypotension required admission. We also had to admit patients who did not satisfy the above criteria for logistic reasons also. All hypoxic patients received Inj. Dexamethasone; 8 mg IV once a day for three days, followed by 6 mg per day for three days, followed by 4 mg once a day for three days and stopped. Five admitted patients received Inj. Remdesvir; 200 mg IV was given on Day 1, followed by 100 mg IV for a total of five doses, before the next haemodialysis sessions. The first two patients who were admitted did not receive Remdesivir because of a lack of data among usage in CKD patients at that point of time. Among the total 32 patients included in the study, 8 (25%) patients received glucocorticoid therapy, 5 (15.6%) patients received remdesivir and 7 (21.8%) patients required hospitalization. Among the seven patients, three (9.37%) patients were discharged and a total of 4 (12.5%) patients died in our study. two patients died due to Acute Respiratory Distress Syndrome (ARDS) and one patient died due to ARDS and secondary sepsis. All COVID-19 positive patients received oral nicomalone, an oral anticoagulant, 1 mg per day on a non-dialysis day. All admitted patients received unfractionated heparin 5000 units per day intravenously and later switched over to oral nicoumalone. at the time of discharge. We did not use newer oral anticoagulants on our haemodialysis patients. Those patients who were in home quarantine were followed up daily over the phone by our manager and dialysis technicians. In the non-hospitalized patient group, one patient succumbed to sudden cardiac death at home.
Discussion
The incidence of COVID-19 infection in our unit was 17.9%. This is similar to studies reported from the US (14%) and France (19%) during their peak transmission period [15,16]. Data from India are sparse. One study from Mumbai reported COVID infection incidence in haemodialysis patients to be only 6.74%. But this study duration was for two months and also early in the pandemic in India. In our study, we have spanned our data collection to eight months and have seen peaks and troughs during the COVID pandemic [17]. We have reported the baseline characteristics of 32 haemodialysis patients with COVID-19 infection. In our study, we found a higher proportion of patients with hypertension (71.8%), followed by diabetes (56.4%). Hypertension, cardiovascular disease, diabetes mellitus, renal disease, smoking and COPD were most common among hospitalized patients with COVID-19 [18]. In our study, we found the most common symptoms in the COVID-19 positive patients included fever, body pain and cough, which were similar to the findings of other studies on haemodialysis patients with COVID-19 [19,20]. Screening of the entire cohort of haemodialysis patients was not done as per the instructions from the hospital administration. So, we could not decipher the asymptomatic caseload in our unit. If strict infection control and isolation policies are followed, these asymptomatic patients who are known to have prolonged viral shedding rates still may not be a threat and cause the spread of COVID-19 [21].
Management of haemodialysis patients who have contracted the COVID-19 is challenging. We did not administer HCQ, ivermectin or macrolide antibiotics to our patients. Those patients who were hypoxic received steroids as highlighted above. Available data suggest that the use of dexamethasone lowered mortality in patients on invasive ventilation [22]. Remdesivir was initially shown to be contraindicated in eGFR < 30 ml/min/m2 [23]. We gave Remdesivir to all our patients after there was evidence from studies showing a safety profile in CKD Haemodialysis patients [24]. In our study, we found mortality in three patients who had been put on steroid therapy and remdesivir. However, this finding cannot be generalized as this study was conducted in a small sample. We reported a very low mortality rate of 12.5%. This is in contrast to the western countries, where the mortality rate is 20–30% [25]. Dialysis patients may not mount a severe cytokine response due to weakened immune system from uraemia and this could be postulated as one of the reasons, they do reasonably well. Another reason for the difference in mortality rates could be the advanced age of the geriatric population in western countries.
We reemphasize the isolation and standard precautionary measures advised by the European Dialysis Working Group (EUDIAL) and the Centre for Disease Control and Prevention (CDC) have framed protocols for COVID-19 management of the dialysis population [26,27]. A report revealed the measures taken in Wuhan to contain the risk of infection of patients on long term haemodialysis included patient education, compulsory temperature screening, designated COVID-19 hospitals, and chest CT screening were key to early identification [28]. Similar reports have been published in a study conducted in Korea [29].
The limitation of our study is that it is a descriptive study and the sample size is small. Further research with a large sample and analytical studies are recommended.
We have gained experience in the management of haemodialysis patients during the COVID-19 outbreak by prompt implementation of strict standardized measures. We brace ourselves to the next wave of the new strains of COVID-19, with the ray of hope that the vaccine would be available to all in the near future.
Competing interests
The authors have no competing interest to declare.
References
- World Health Organization. Weekly operational update on COVID-19–30 October 2020. Available from: https://www.who.int/publications/m/item/weekly-operational-update—30-october-2020.
- Liu D, Cui P, Zeng S, et al. Risk factors for developing into critical COVID-19 patients in Wuhan, China: A multicenter, retrospective, cohort study. EClinicalMedicine 2020;25:100471.
- Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 2020;395(10298):1678–1680.
- Chang AY, Cullen MR, Harrington RA, Barry M (Stanford University, Stanford, CA, USA). The impact of novel coronavirus COVID-19 on noncommunicable disease patients and health systems: a review. J Intern Med. 2020;joim.13184.
- Bikbov B, Purcell CA, Levey AS et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020;395(10225):709–733.
- Foreman KJ, Marquez N, Dolgert A et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet 2018;392(10159): 2052–2090.
- Kato S, Chmielewski M, Honda H et al. Aspects of immune dysfunction in end-stage renal disease. Clin J Am Soc Nephrol. 2008;3(5):1526–1533.
- Kazancioǧlu R. Risk factors for chronic kidney disease: An update. Kidney Int Suppl. (2011). 2013;3(4):368–371.
- Sarnak MJ, Jaber BL. Pulmonary infectious mortality among patients with end-stage renal disease. Chest 2001;120(6):1883–1887.
- Chou CY, Wang SM, Liang CC et al. Risk of pneumonia among patients with chronic kidney disease in outpatient and inpatient settings. Medicine (Baltimre) 2014;93(27):e174.
- Taghrir MH, Akbarialiabad H, Marzaleh MA. Efficacy of mass quarantine as leverage of health system governance during COVID-19 outbreak: A mini policy review. Arch Iran Med. 2020;23(4):265–267.
- Rincón A, Moreso F, López-Herradón A et al. The keys to control a COVID-19 outbreak in a haemodialysis unit. Clin Kidney J. 2020;13(4):542–549.
- Albalate M, Arribas P, Torres E, et al. High prevalence of asymptomatic COVID-19 in hemodialysis. Daily learning during first month of COVID-19 pandemic. Nefrologia. 2020;40(3):279–286.
- Trivedi M, Shingada A, Shah M, Khanna U, Karnik ND, Ramachandran R. Impact of COVID-19 on maintenance haemodialysis patients: The Indian scenario. Nephrol. 2020;25(12):929–932.
- Rosenberg ES, Tesoriero JM, Rosenthal EM, et al. Cumulative incidence and diagnosis of SARS-CoV-2 infection in New York. Ann Epidemiol. 2020;48:23-9.e4.
- Creput C, Fumeron C, Toledano D, Diaconita M, Izzedine H. COVID-19 in Patients Undergoing Hemodialysis: Prevalence and Asymptomatic Screening During a Period of High Community Prevalence in a Large Paris Center. Kidney Med. 2020;2(6):716-23.e1.
- Deshpande R, Dash S, Bahadur MM, et al. Study of COVID-19 pandemic in representative dialysis population across Mumbai, India: an observational multicentric analysis. J Assoc Physicians India 2020;68(10):13-17.
- Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8(1):1–14.
- Wu J, Li J, Zhu G, et al. Clinical features of maintenance hemodialysis patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Clin J Am Soc Nephrol. 2020;15(8):1139–1145.
- Tian M, Li H, Yan T, et al. Clinical features of patients undergoing hemodialysis with COVID-19. Semin Dial 2021;34(1):57–65.
- Aguilar JB, Faust JS, Westafer LM, Gutierrez JB. Investigating the impact of asymptomatic carriers on COVID-19 transmission. medRxiv. Forthcoming 2020. doi:https://doi.org/10.1101/2020.03.18.20037994
- Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with COVID-19 — Preliminary Report. N Engl J Med. 2020;NEJMoa2021436.
- Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the Treatment of COVID-19 — Final Report. N Engl J Med. 2020;383(19):1813–1826.
- Aiswarya D, Arumugam V, Dineshkumar T, et al. Use of remdesivir in patients with COVID-19 on hemodialysis: a study of safety and tolerance. Kidney Int Rep. Forthcoming 2020. doi:https://doi. org/10.1016/j.ekir.2020.12.003.
- Alberici F, Delbarba E, Manenti C, et al. Brescia renal COVID task force. management of patients on dialysis and with kidney transplantation during the SARS-CoV-2 (COVID-19) pandemic in Brescia, Italy. Kidney Int Rep. 2020;5(5):580–585.
- Basile C, Combe C, Pizzarelli F, et al. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres. Nephrol Dial Transplant 2020;35(5):737–41.
- Almonte K, Weiner DE. COVID-19 universal testing in hemodialysis facilities to reduce infection risk. Kidney Med. 2020;2(6):681–683.
- Li J, Xu G. Lessons from the experience in wuhan to reduce risk of COVID-19 infection in patients undergoing long-term hemodialysis. Clin J Am Soc Nephrol. 2020;15(5):717–719.
- Cho JH, Kang SH, Park HC, et al. Hemodialysis with cohort isolation to prevent secondary transmission during a COVID-19 outbreak in Korea. J Am Soc Nephrol. 2020;31(7):1398–1408.

