Non-Motor Symptoms of Parkinson’s Disease – The Elephant in the Room
Parkinson’s disease (PD), is a slow progressive neuro-degenerative disorder where symptoms occur gradually and get worse over time. As we live longer than in previous centuries, the prevalence of aging-related neurodegenerative conditions like PD will get diagnosed more frequently. A small proportion of younger adults show symptoms in their 40-50 years due to genetic reasons.

Each individual with PD will have different symptoms and no two patients are the same clinically. Most present with the following motor symptoms.
- Tremors in Hands or Feet – Often one-sided, which gradually spreads to the other side.
- Rigidity – Stiffening of limbs or trunk or low back.
- Bradykinesia – Slowness in movements and activities.
- Gait Imbalance – Stooped posture with a festinant walk and a tendency to fall backwards.
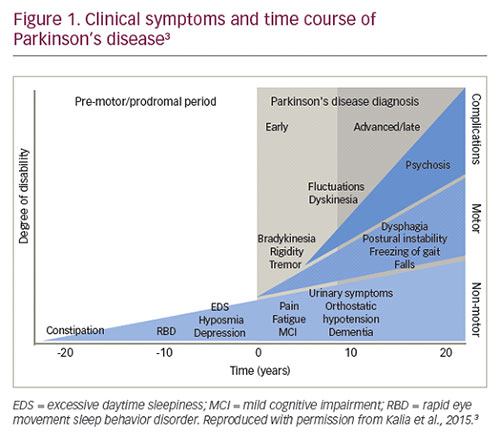
Non-motor symptoms are often considered to be “The elephant in the room.” This is because they are often overlooked by both clinicians and patients due to poor understanding and under-reporting leading to under treatment. Non-motor symptoms predate motor symptoms by 5-10 years and if picked early and treated, significant improvement in quality of life can be achieved.
Most patients I see get surprised when asked and start connecting the dots on the evolution of PD in them. Autonomic dysfunction is the commonest. For e.g., loss of sense of smell often predates motor symptoms by a few years and so does chronic constipation. Some have hyper salivation, postural dizziness due to poor blood pressure control after standing and poor bladder control or frequent night visits to the toilet. Painful feet and legs, which make them walk about in the middle of the night to get comfortable (restless legs syndrome) is noted in the minority.
Vivid dreams and sleep talking/nightmares (REM sleep behaviour disorder) are present many years before motor presentation. Anxiety and depression are common early features and hallucinations, often visual (seeing imaginary people, animals or objects) are late features. Some develop delusions, paranoia (suspicious behaviour) and memory loss.
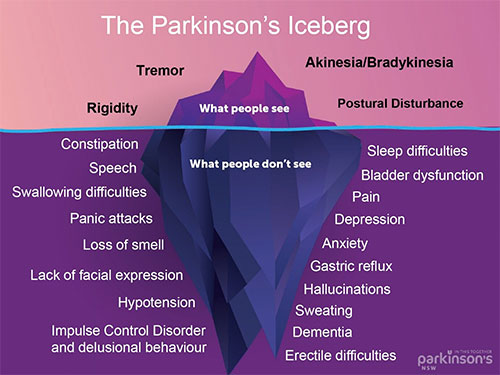
Most non-motor symptoms if not present at the time of diagnosis may evolve while on medical treatment and are challenging to manage. Sleep fragmentation, fatigue and apathy need additional drug introduction. Medications may often worsen non-motor symptoms; for e.g., dopamine drug-induced insomnia, hallucinations and postural dizziness warrant dose titration and limiting use at night.
Compulsive/Impulsive Behaviour: Carers often notice compulsive behaviour – an overwhelming urge to act in a particular way like searching the internet or collecting items or data, or an urge to keep walking. This is usually out of character and the person may be unaware of their personality changes. When they cannot resist the temptation to carry out certain activities, it is known as impulsive behaviour, or impulse control disorder (ICD). Some go on to buy online recklessly or shop excessively almost losing all their savings. Rarely, gambling or watching inappropriate content on the internet is a major issue. Some of these can be made worse by direct dopa agonist drugs and it is always discussed during treatment and follow-up visits.


