Image-guided Biopsies – A Safer Technique for Diagnosing Lumps

“Precise diagnosis- a beginning for the right and effective treatment”
Quick facts on the image-guided biopsy:
- In the biopsy procedure, we take a tissue sample from the lump in the body to make a diagnosis.
- Utilizing “imaging guidance” makes the biopsy effective and paves the way for a right diagnosis
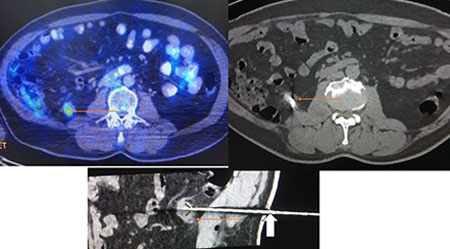
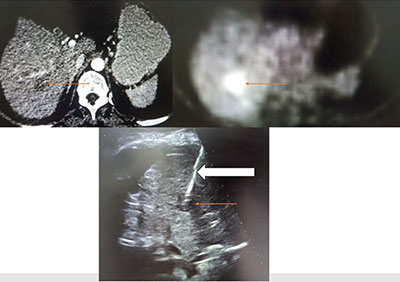
- “Biopsy” under image guidance means that images or pictures taken through a CT scan, an ultrasound, or an X-ray will be used by us to get the tissue samples from the right place where the disease is located.
- The procedure usually takes about 45 minutes to 2 hours.
- This procedure has got a few special rules for eating and drinking before the procedure
Please read this article fully to understand more about the procedure, usefulness, and risks associated with the procedure.
What is an image-guided biopsy procedure?
A biopsy procedure is done to find out the swelling or lump, the nature of the lump or swelling, type of the disease, and severity of the swelling. Sometimes we also take biopsy of the liver or kidney without any swelling to know more about the pre-existing liver or kidney disease.
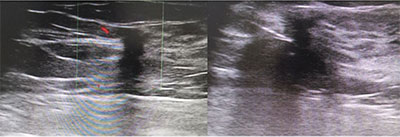
Imageguidance is being used commonly to find out the best and safest location to take the tissue. Hence, we usually use an ultrasound or a CT or a special type of X-ray (angiogram or fluoroscopy) to see inside the body where the swelling is located. Using these images as a guide, we will place a thin needle into the spot while taking maximum precautions not to injure any normal structure. The needle will take out the tissue which can be tested in the lab under the microscope to know about the disease process completely.
Since images are required to guide the needle placement, the procedure will commonly be done in two areas
- In the ultrasound scan room or CT scan room using ultrasound or CT scanner, respectively.
- In the Interventional radiology (IR) suite using ultrasound or fluoroscopy (special type of X-ray).
What are the home preparations required before the procedure?
There are some “eating”, “drinking”, and “medicine” rules to be followed at home on the day or the day before the procedure day.
- Eating should be stopped 4-6 hrs before the procedure, and nothing solid should be taken by mouth during this time
- Drinking water should be stopped, atleast 2 hours before the procedure.
- Medicines like blood-thinners (commonly used after heart problems) may have to be stopped a few days before the procedure. Other common medicines for diabetes (sugar) and high BP may be continued. These have to be discussed with the biopsy-performing doctor beforehand.
- If the patient is not cooperative for the procedure, then an anaesthetist consultation may be required to use sedation or anaesthesia to perform the procedure.
The rules that need to follow for children include
- You may need to bring along a “comfort” item- like a favourite toy for your child to hold during the procedure.
- More than adults, for children we may need to use sedation or anaesthesia to perform the procedure, so anaesthesiologist opinion may be required. “Eating” and “drinking” rules are to be followed as per the anaesthetist opinion.
- Otherwise, the “eating”, “drinking” and “medicine” rules apply the same as that of adults.
How the procedure will be performed?
The image-guided biopsy will be done by the radiology doctor (interventional radiology doctor) at the Department of diagnostic and interventional radiology, Kauvery hospital. Interventional radiology is a branch that deals with performing minimally invasive procedures with imageguidance.
The procedure will take place in the CT/ ultrasound room (daycare procedure room) or interventional radiology suite (cath lab. An interventional radiology doctor will be there in the room who will perform the procedure and nurses and technologists who will assist the procedure. The doctor and other staff will wear caps, gloves, masks, and gowns during the procedure as a part of strict infection control measures.
- The patient will be asked to change the dress (hospital dress) and placed comfortably on a bed or CT scan table on the back down or abdomen down position depending on the location of the lump. Head rests, pillow, and blanket will be given for maximal comfort during the procedure.
- A special antiseptic solution will be used to clean the part where biopsy will be performed.
- Once the cleaning process is over, the body of the patient will be covered with a sterile sheet all over except for the place where the biopsy will be done. The sterile sheet will be clean and infection-free.
- Then, a small medication will be given through a small needle to numb the area so that the patient will be locally anesthetisized and he/she will not feel any pain.
- A special type of needle (known as biopsy gun) will be passed through the chosen area under the imageguidance. The biopsy gun is of two types: “automatic” and “semi-automatic”. This will be chosen based on the location of lump and accessibility of the lump.
- When the needle is inside the desired location after confirming with the imaging, the needle inside the lump will be taken a snapshot for future references. Then the biopsy gun will be clicked to remove the tissue, and during this time, the patient will hear a click sound.
- Once the needle is removed, it will contain the tissue from the lump. This is called a sample. 2 to 3 good samples will be taken, enabling the pathologist to accurately diagnose the nature and type of the lump.
- The taken sample will be sent in containers with a special solution (mostly formalin) to the pathology department.
- After completing the procedure, the body part where the biopsy is done will be bandaged.
- The patient will be observed for 4 to 6 hours after the procedure in the hospital itself for any complications or risks incurred during the procedure
- A pathologist (a doctor who studies these tissues under the microscope) will examine the tissues sent and give a precise diagnosis.
As a patient, there may be concerns regarding the safety (risks) of the procedure and also about the radiation procedure. There may be small risks associated, which will be explained to the patient and attenders before the procedure. Regarding radiation, ultrasound image guidance has no radiation danger, but CT and fluoroscopy (a special type of X-ray) may have radiation.However, it will be reduced as we use advanced equipment anddo periodical inspection of the equipment.Parts of the body not in the vicinity of biopsy will be protected.
Our goal is to do the procedure correctly and thoroughly. At the same time, the risks are minimum and the patient does not suffer any complications related to the procedure or to the radiation while using the image guidance.
Quick facts about sedation:
- If sedation or local anaesthesia medication is being used, it is likely that the patient will not feel pain during the procedure or after the procedure.
- A doctor (radiologist or anaesthesiologist) will always be present during the procedure to look for the effects of sedation or anaesthesia medication.
- “Eating” and “”drinking” rules are already described above (vide supra).
Role of the attendee during the procedure:
We welcome and require your help and support before and after the biopsy procedure. The most important role of the attendee (bystander) is to help the patient stay relaxed before the procedure
During the procedure, our team will always be there taking care of the patient, and hence the attendee (bystander) may have to co-operate with us and wait outside the procedure room.
After the procedure:
When the patient is out of the biopsy room, he/she will be observed in the daycare room for 4 hours (if the patient is an out-patient) or sent to the ward-room (if the patient gets the procedure done as an in-patient after admission) to prevent any bleeding or complications after the biopsy.
The patient should lie on the biopsy side down to prevent any inadvertent bleeding from the site.
The interventional radiology doctor will give specific instructions regarding “eating”, “drinking”, and “medication” advice after the procedure.
The biopsy report will usually be available after 3 days to 1 week, depending on the biopsy. The report will be sent to the treating doctor, and the doctor will relay these results to you.
Special needs and patient preparation:
If the patient has any special needs or health issues and feels the doctor performing biopsy should know about it, please call the Centre for diagnostic and interventional radiology and speak with a nurse before the biopsy is done. It is important to notify us in advance about any special needs.
Before coming to the hospital, it is better to explain the patient about the procedure in words that they can understand. Preparing the patient before and comforting them as well will help the patient to gain a positive experience. If you have any questions to help prepare the patient for the procedure, please contact us (Centre for diagnostic and interventional radiology, Kauvery hospital).
“Wishing all our patients have a healthy and speedy recovery”

Dr. S. Santhakumar
Consultant Interventional Radiologist
Kauvery Hospital, Chennai

