Sarcopenia – Loss of Skeletal Muscle Mass
Introduction:
Sarcopenia is the progressive loss of skeletal muscle mass, strength, and function with aging. The term SARCOPENIA is derived from the Greek phrase “poverty of flesh”.
It was Critchley who was the first to identify (way back in 1931) the reduction of mass of the hand and feet muscles with age. This reduction has adverse physiological as well as psycho-social effects on the elderly since it makes it difficult for them to perform their daily activities, increases fall risk and increases their dependence on others. The loss of independence can lead to social isolation and depression while physical inactivity increases the risk of chronic conditions and mortality.
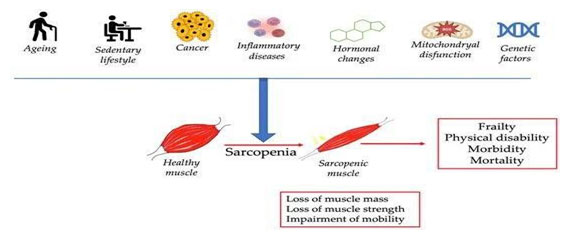
Sarcopenia has also been associated with other chronic inflammatory conditions like diabetes, obesity, and cancer. Neurological, metabolic, hormonal, nutritional and physical-activity-related changes with age are likely to contribute to the loss of muscle mass.
Causes:
- Age-related natural processes.
- Reduction in type 2 muscle fibre, size and number.
- Being sedentary without any exercise, obesity and insulin resistance.
- Diminished androgen and growth factor serum concentration, reduced protein consumption and inadequate muscle protein synthesis (MPS) response to strength training and protein intake.
- Furthermore, sarcopenia is linked to, and may partially result from, various chronic conditions that adversely impact the musculoskeletal system, and physical activity.
- The elderly population often experiences inadequate protein intake and insulin resistance. This deficiency in protein results in reduced levels of several amino acids essential for skeletal muscle metabolism and overall health.
Pathophysiology:
- Age-related reductions in anabolic hormones like testosterone, HGH, and IGF-1, which are crucial for muscle development and maintenance, are commonly seen in individuals with sarcopenia.
- Aging individuals often develop “sarcopenic obesity”, characterized by increased fat and reduced muscle mass, which is linked to metabolic dysfunction and insulin resistance (IR). IR promotes visceral fat accumulation and is inversely related to skeletal muscle mass. This pathology is likely due to insulin’s impaired effects on muscle, hindering its ability to prevent muscle breakdown and promote protein Additionally, the loss of lean body mass reduces glucose uptake by muscles, exacerbating IR.
- Age-related neurodegeneration, including a decline in alpha motor neurons in the spinal cord, peripheral nerve fibers, and neuromuscular junctions, contributes to reduced muscle strength and size in sarcopenia.
- Increased levels of inflammatory markers such as CRP, TNF, IL-6, and IL-1 are commonly seen in the These cytokines are known to have catabolic effects on skeletal muscles, potentially contributing to the development of sarcopenia with aging.
- Sarcopenia has been associated with cognitive decline and dementia in older adults. Research indicates that reduced muscle mass increases the risk of dementia, with a clear link between muscle loss and cognitive deterioration in those aged 60 and above. This connection is believed to be mediated by inflammatory factors and myokines, such as CRP and IL-6, which are also involved in muscle mass reduction.
Symptoms:
- Loss in muscle strength, quality and physical performance
- Mobility disorders
- Impaired ability to perform activities of daily living
- Disabilities
- Loss of independence
- Reduced quality of life, and therefore, higher risk for morbidity (falls, bone fracture, metabolic diseases, etc.) and mortality.
Dietary Protein Strategy Against Sarcopenia
As people age, there is an imbalance between protein synthesis and breakdown which causes a reduction of muscle mass and decreased functionality. This affects muscle plasticity and its interaction with organs like the liver, fat, and bones. This condition, known as primary sarcopenia, is mostly due to reduced anabolic hormones, which cause reduced muscle response. In this metabolic state, consuming enough protein through diet plays an important role in preserving muscle health. How much protein a person should consume is dependent on age, gender, health status and fitness.
Young people and adults need a protein intake of approximately 0.7 g/kg body weight/day; in older people, the European Society for Clinical Nutrition and Metabolism (ESPEN) recommends a diet containing at least 1.0–1.2 g protein/kg body weight/day for healthy older adults (≥ 60 years old), whereas a higher protein intake (1.2–1.5 protein/kg body weight/day) may be beneficial for elderly and sarcopenic adults with acute or chronic diseases.
Physical Exercise vs. Sarcopenia
Lifestyle is a key factor in sarcopenia, with a sedentary lifestyle contributing to muscle weakness and a reduction in muscle mass and strength. In contrast, an active lifestyle helps prevent muscle deterioration, suggesting that exercise is beneficial for all age groups.
High-intensity exercise for a long duration stimulates muscle protein synthesis and enhances fatty acid breakdown for ATP production, consequently reducing adipose tissue. Additionally, physical exercise along with sufficient protein intake boosts protein production and reduces protein breakdown due to increased blood insulin concentration.
The musculoskeletal system is not the only system to benefit from regular exercise. The risk of chronic conditions like cardiovascular conditions, hypertension, diabetes, cancer, etc. is also reduced. For the elderly, physical activity not only helps prevent/manage sarcopenia but it also serves to increase muscle mass and strength. A combination of resistance training, aerobic training, functional training, etc. is advised. The exercise intensity is usually increased in a gradual manner by the physiotherapist. The physiotherapist will also give a personalized plan for the patient after taking into consideration factors like age, gender, activity level and the presence of other medical conditions.
Exercise-Induced Protein and Sarcopenia
In recent years, exercise-induced skeletal muscle contractions have led to the production of myokines — small proteins and proteoglycan peptides that help maintain skeletal muscle health by regulating muscle mass, energy metabolism, and inflammation. Myokines act locally and systemically, influencing organs like the liver, brain, and fat tissue. Key myokines, such as IL-6, IGF-1, and irisin, play roles in muscle growth, mitochondrial function, and metabolic homeostasis. Understanding how these myokines work can help prevent muscle loss and improve health in the elderly.
Evaluation:
- Screening Tools to Identify Probable Sarcopenia: The SARC-F questionnaire is a screening tool that assesses strength, assistance with walking, rising from a chair, climbing stairs, and
- Physiotherapist assessing muscle strength like handgrip test, chair stands test, etc.
- Confirming Sarcopenia – Muscle Quantity or Quality:
- Magnetic resonance imaging (MRI): Considered a “gold standard” modality for confirming sarcopenia, it gives precise muscle mass measurements.
- Computed Tomography (CT): Also considered a “gold standard” for accurate lean muscle mass measurement.
- Dual-Energy X-Ray Absorptiometry (DEXA): While not as accurate as either CT or MRI, DEXA presents with greater convenience.
- Bioelectrical Impedance Analysis (BIA): Perhaps the most widely available and portable modality of muscle mass quantification.
- Physiotherapist measuring physical performance to identify sarcopenia Once sarcopenia is confirmed through body composition assessment, the severity of the condition is determined by measuring physical performance.
- Gait speed test
- SPPB test (Short Physical Performance Battery)
- TUG test (Timed up and Go test)
- 400 meter walk test
Treatment:
According to the assessment of the SARC- F questionnaire, muscle strength of upper body and lower body, muscle girth and physical performance test, the physiotherapist will give a tailored exercise therapy program according to individual needs and goals (specifically resistance training). Therapeutic techniques to restore muscle strength, mobility, and independence will also be taught. This approach reduces muscle loss and enhances strength thus helping in both prevention and management of sarcopenia.
Increasing the intake of protein, either through food or with supplements, is also effective in sarcopenia management. 20 – 30 gm of protein consumption during every meal is recommended. This will help meet amino acid requirements to boost MPS and reduce muscle loss associated with aging.
Combining resistance training with protein-rich diets has shown the maximum effectiveness in handling the condition.
Sarcopenia is a multifactorial condition requiring a combination of resistance training, functional exercise therapy, and targeted nutritional strategies. Physiotherapists, along with dietitians, can design personalized programs to preserve muscle mass and improve quality of life. Early intervention is key to preventing severe muscle loss and maintaining independence.
Takeaway: Stay active, eat a balanced diet, and consult professionals to effectively combat and overcome sarcopenia!

Mrs. Selvambikai Srinath
Physiotherapist
Kauvery Hospital, Chennai

