In the Eye of the Storm
Reality, the calm before the storm or in the eye of the storm?
Yet another diabetes day for awareness and we seem to be gearing up to the reality of the complications of diabetes encountered. This pandemic has taught us a great deal about dealing with all medical conditions and complications and the diabetic foot management has in particular thrown up a few more challenges.
The scary statistics mentioned below, the natural history of the disease and the aforementioned experience during the pandemic have left us already in the eye of the storm of complications of diabetic foot.
To recap on the statistics related to DM and diabetic foot,
DM in India – 6.9 crore cases
Jharkhand 5.3%
Tamil Nadu 10.4%
Chandigarh 13.2 %
1 in 4 population say “I don’t know” i.e., 52.1% is still undiagnosed, that’s another 3.6 crore which brings us close to 9.3% of the population involved.
In the US alone, 84 million above the age of 20 are prediabetic!
90 – 95% people with type II diabetes
Incidence increases with age: 25% over age 65
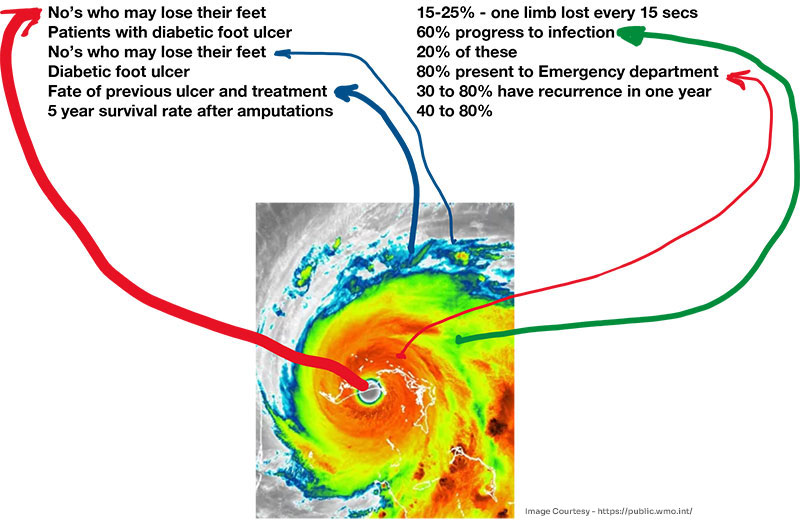
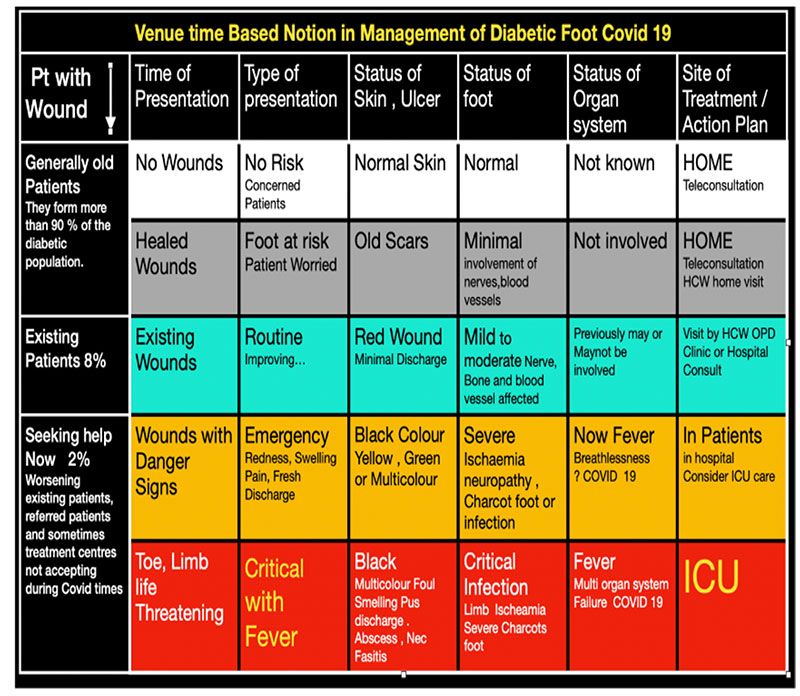
The patients and the health care providers are in the storm of diabetes. We are the diabetic capital of the world, etc., is an often-repeated term. Diabetic foot as a subset also experiences a storm. Where we stand and how we progress is the question to be solved. The eye of the storm is the end point where the diabetic foot with its complications gets sucked into the stages of going to the hospital for treatment at various stages of complications and finally the patient succumbs. A happy ending is a reverse where the diabetic foot stays in the green and the blue zone and finally gets restored to functional foot and resumes daily normal functions. The idea is to weaken the storm. Education is the key.
Education imparts knowledge which finally creates awareness and helps prevent complications and finally helps conquer the complications.
So, in correlating the storm and the table above with colour codes, we find that there is a role for everyone in the medical field dealing with diabetic foot.
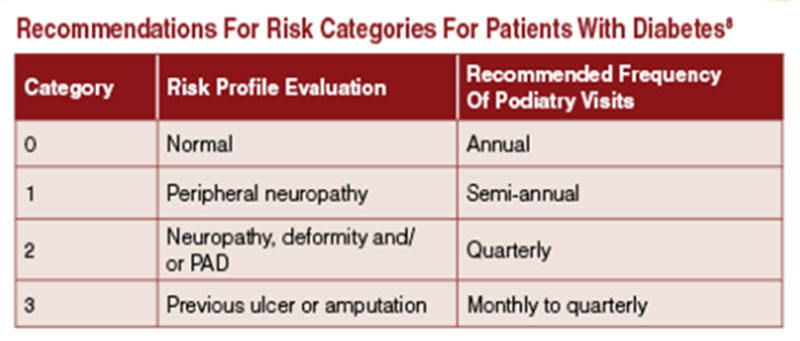
The white and grey zone is the preview of the GPs and diabetologists ably supported by the occupational therapists and the physiotherapist. The goal is early detection and preservation of the foot. Risk stratification as shown in the table below gives the severity of the foot. Regular examination of the components of the foot is essential to evaluate this.
Patients with no risk factors can be seen every year for surveillance. When neuropathy sets in which is a mild risk, patients have to be seen every 6 months. Ischemic and vascular compromise is a much more dreaded risk factor and these feet need to be seen every 3 months. When you detect deformity alone or in combination with the above complications, the risk of developing an ulcer rises exponentially. More frequent visits are necessary. With a history of ulcer presence and a healed previous ulcer the risk is much more real.
Peripheral Vascular Disease
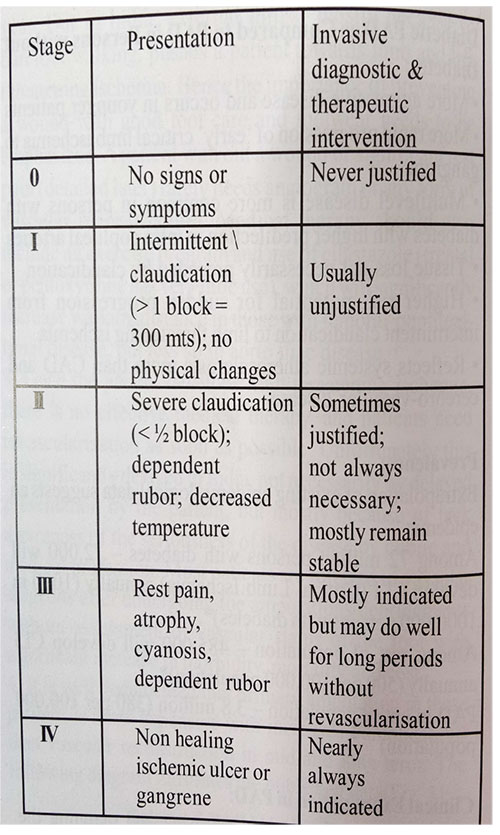
The next dreaded complication is peripheral vascular disease. Well recognised guideline for the management of this is given in this table. This gives a clear and simple method which can be used in the clinic and guides us on the future course of action.
The presence of peripheral vascular disease and the need to investigate it further is a very essential, important and urgent decision to be made. Over investigation is generally seen. This may give a false sense of normalcy. A keen history and physical examination are the key. Having done that, a reference to the table adjacent guides us to order and proceed with the investigations required. Some of these investigations have to be done very cautiously. The presence of renal and cardiac complications can get exacerbated and may precipitate a grave systemic combination. Cost also has to be kept in mind in these patients as some of these tests can be expensive. A proper educated decision is therefore of utmost importance.
Infection With or Without General Involvement:

We now have an example of a diabetic foot condition in the orange zone of the cyclonic storm. This represents the ulcer with the danger signs in the table; these have to be treated as urgent. Proper treatment will make sure the foot comes out of the storm and the cyclone weakens. The foot gets thrown out from the cyclone and lands to tell a story of success. This is an example of footwear causing necrosis and infection. This patient also has compromised vascularity. A combined team approach is necessary to not only save the foot but also to rehabilitate the foot to what it was, to be able to bear weight and last long. Improper timing of consulting a surgeon and a plastic surgeon, improper antibiotics and improper medical and wound care will push this foot into the center of the storm. The patient may have to be treated in the ICU, with appropriate antibiotics and of course timely surgical debridement. Foot and life may enter the eye of the cyclonic storm and be gone forever.
This brings us to the next question of proper footwear.

Footwear forms an important aspect of management of diabetic foot.
With neuropathy in its mild form and properly fitting footwear, the diabetic foot rides in the blue and the green portion of the storm. This is where great care has to be taken in the form of early detection and careful surveillance to detect feet at risk of developing an ulcer and all its attendant complications. The storm can become more virulent if that happens.
Footwear Should
- “Protect, protect and protect the foot.”
- “Should do the work of the normal foot in impaired foot.”
- “Be worn in the house also.” – sadly, only 15% do this.
Foot Care:
This forms an essential part of the treatment of the diabetic foot.
- Daily foot examination by the patient.
- Cleaning of the foot. Do not soak the foot for long periods.
- Moisturising creams are a must to keep the foot skin in pristine condition.
- Proper and regular nail care. Nails should be cut very carefully.
- Web spaces have to be kept dry.
- Look for signs of footwear damage or strain.
- Escalate shoe wear. Get advice from an expert for the proper fitting of footwear.
We are in the midst of a storm. The statistics numb us.
Let us ride the storm and get out.
Prof V B Narayanamurthy
Sushrutha Professor in Plastic Surgery
Kauvery Hospital, Chennai

