A case of severe malaria complicated by concurrent H3N2 influenza infection: Diagnostic and therapeutic challenges
A. Mahalakshmi
Physician Assistant, Dept of General Medicine, Kauvery Hospital, Cantonment, Trichy
Case Presentation
A 29 year old male patient, oil gas engineer by profession – in Nigeria reached India on last week, presented with following chief complaints,
- Fever with chills on & off × 6 days.
- Cough and cold × 3 days.
- Headache on and off × 3 days.
- Breathing difficulty on &off × 3 days.
- Generalized body pain
- Decreased appetite × 3 days.
- Nausea × 3 days.
- High coloured urine. × 2 days
- H/O- abdominal pain × 2 days
- H/O- jaundice × 2 days
- H/O- pale stool & diarrhea × 2 days
Past history: Nil comorbidities
Personal history
- Non smoker
- Non alcoholic
- Mixed diet
- Normal bowel bladder movement
- Normal sleep and appetite
On Examination
- Patient is conscious, oriented and afebrile
- Pallor ++
- Icterus+
- No clubbing
- No pedal edema
- No cyanosis
Vitals
- PR- 111/ bpm
- BP- 130/80 mmHg
- Spo2- 98% in RA
- Temperature-98.5f
Systemic Examination
- CVS-S1, S2+
- RS- Bilateral NVBS
- P/A- Soft , hepatosplenomegaly
- CNS – GCS 15/15, No functional neurological defecits
Investigations
Inflammatory blood markers test
| S. LDH | 1918 |
| S. Procal | 5.25 |
| ESR | 35 |
| CRP | 33.12 |
Discussion on Investigations
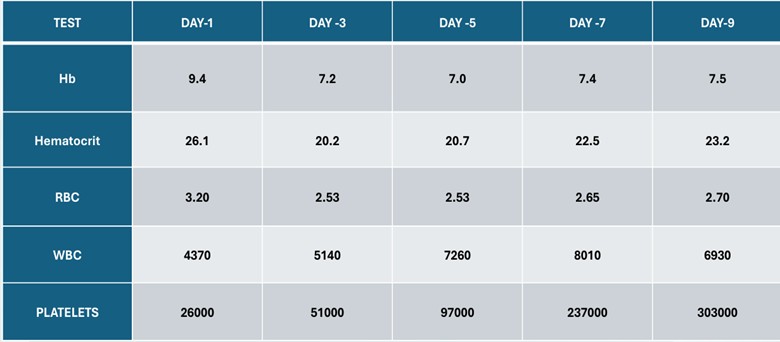
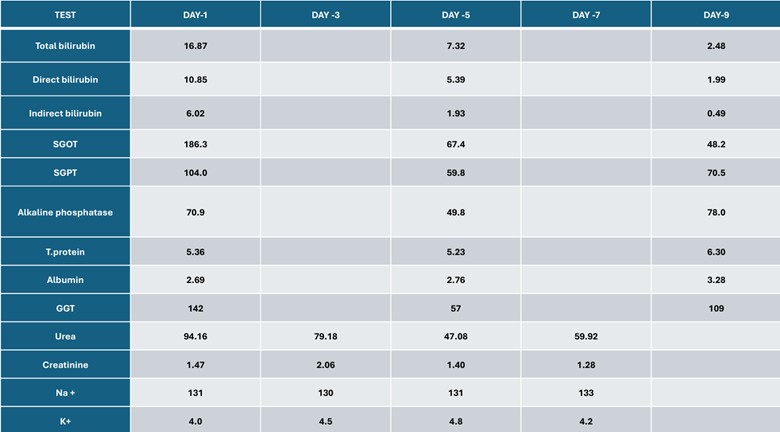
- The results of hematological testing revealed normocytic normochromic anemia, pancytopenia
- LFT- were high level
- RFT- Deranged
- Hypoalbuminemia
- High LDH-indicating an active hemolysis.
- Peripheral blood smear- p.falciparum and p.vivax
- High S. Procalcitonin level
- CRP& ESR- which are both inflammatory blood markers that indicate an ongoing infection, were higher than the normal levels.
Serological Testing – Negative
RT PCR – H3N2 influenza infection
MP/MF – Positive
Case Overview
Patient Diagnosis: Severe Malaria with Concurrent H3N2 Influenza Infection.
Initial Management
Admitted to ICU for intensive care and close monitoring. Started on Artesunate Combination Therapy for malaria treatment. Antibiotics was started or potential secondary bacterial infections. (Inj. Doxycycline 100mg IV BD), (Inj. Cefoperazone sulbactam 1.5 gm IV BD). Proton Pump Inhibitors (PPI) to manage gastric acid and potential risk of gastrointestinal bleeding. Hepatoprotectives to protect the liver from the effects of severe malaria and medications. Blood Transfusion was done 2 units of packed RBC transfused because of low hemoglobin.
Combination of drugs (Artesunate)
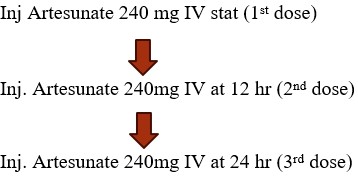
Day-1: Tab Artesunate 240mg + sulfadoxine 1500mg Day -2:Tab.Artesunate 200mg + Tab.primaquine 45mg Day-3:Tab.Artesunate 200mg and then started on Tab. Primaquine 15 mg OD for 10 days.
Serological Testing and Diagnosis
- RT-PCR Testing: Confirmed H3N2 influenza infection.
- Management Adjustments: Started on Antiviral Therapy for influenza (Oseltamivir).
- Dual Infection: Severe malaria and H3N2 influenza, requiring careful management to prevent complications.
Clinical Progress and Recovery
Patient’s Symptomatic Improvement
- Gradual recovery in ICU with support and management.
- Fever subsided, improvement in general well-being.
- Decreased malaria parasite load.
- Influenza symptoms began to resolve with antiviral therapy.
Transfer to Ward
Patient Shifted to Ward for further management after stabilization. Continued malaria treatment and supportive care. Influenza management was carried out. Close monitoring for any relapse or complications.
Discussion
Malaria is a life-threatening disease caused by Plasmodium parasites. Transmitted through the bite of an infected female Anopheles mosquito.
Common species: Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, Plasmodium malariae.
What is Mixed Malaria Infection?
Occurs when a patient is infected with more than one species of Plasmodium simultaneously.
The most common combinations:
- Plasmodium falciparum + Plasmodium vivax
- Plasmodium falciparum + Plasmodium malariae
- Plasmodium vivax + Plasmodium ovale
Importance: Co-infection can complicate diagnosis and treatment
Prevalence of Mixed Malaria Infection
More common in regions where multiple Plasmodium species co-exist. Areas in sub-Saharan Africa, Southeast Asia, and parts of South America. Prevalence varies based on geographic location and local malaria control efforts.
Clinical Features
Symptoms can be more severe than single-species infections.
Common symptoms include
- Fever
- Chills
- Sweating
- Headache
- Malaise
- Anemia
- Jaundice
Risk of severe disease increases, especially with Plasmodium falciparum.
Diagnosis of Mixed Malaria Infection
- Microscopic Examination: Blood smear to identify different Plasmodium species.
- PCR (Polymerase Chain Reaction): More sensitive, detects multiple species simultaneously.
- Rapid Diagnostic Tests (RDTs): May be less accurate for mixed infections.
Accurate diagnosis essential for proper treatment.
Challenges in Diagnosis
- Co-infection may lead to a negative RDT result for some species.
- Misidentification in blood smears due to species’ similarities.
- Delayed or incorrect diagnosis can lead to complications and increased mortality.
Artesunate
It is an artemisinin derivative and belongs to the artemisinin class of antimalarial drugs. Artesunate’s primary action in malaria is rapidly reducing the parasite burden, alleviating systemic effects, and contributing to complication resolution. Artesunate is a semi-synthetic derivative of artemisinin, a compound extracted from the plant Artemisia annua. It is the most effective first-line treatment for severe malaria, especially caused by Plasmodium falciparum.
Mechanism of Action
Artesunate works by producing free radicals that damage the malaria parasite. Its key actions include:
- Heme-Iron Interaction: The malaria parasite digests hemoglobin, releasing free heme, which reacts with artesunate to generate reactive oxygen species (ROS). These ROS destroy parasite membranes and proteins.
- Disruption of Parasite Metabolism: Artesunate targets food vacuoles and calcium homeostasis, disrupting parasite growth.
- Rapid Clearance of Parasites: It kills early-stage (ring forms) parasites, preventing them from maturing into more severe forms.
WHO Recommendations
- Artesunate is the first-line drug for severe malaria in all age groups, including pregnant women in the second and third trimesters.
- In areas where artemisinin resistance is reported (e.g., Southeast Asia), artesunate is used in combination therapies.
Dosage and Administration
Intravenous (IV) or Intramuscular (IM) Administration:
- 4 mg/kg at 0, 12, and 24 hours, then once daily until oral therapy can be initiated.
- After IV/IM treatment, switch to oral Artemisinin-Based Combination Therapy (ACT) (e.g., artemether-lumefantrine or artesunate-mefloquine).
Common Side Effects
- Post-treatment hemolysis (destruction of red blood cells)
- Dizziness, nausea, vomiting
- Mild liver enzyme elevation.
Delayed Hemolysis
Some patients experience delayed hemolysis 1-3 weeks after artesunate treatment, particularly those with high parasite loads. This is due to the clearance of damaged red blood cells. Patients should have follow-up blood tests after treatment.
Use in Pregnancy
Safe in the 2nd and 3rd trimesters, for the 1st trimester, WHO still recommends artesunate over quinine due to quinine’s high risk of hypoglycemia.
Treatment of Mixed Malaria Infection
First-line treatment typically involves Artemisinin-based Combination Therapies (ACTs). Specific species-based treatments may be needed (e.g., for Plasmodium vivax relapse). Challenges like ensuring complete eradication of all species, especially dormant forms of Plasmodium vivax and Plasmodium ovale.
Treatment Strategies
- For Plasmodium falciparum and Plasmodium vivax co-infection: ACT plus Primaquine (to clear liver stage of P. vivax).
- For Plasmodium falciparum and Plasmodium malariae co-infection: ACT for falciparum and follow-up treatment for P. malariae.
- Follow-up: Regular monitoring to detect any relapse or resistance.
Prevention and Control
- Vector control: Insecticide-treated nets (ITNs), indoor residual spraying (IRS).
- Malaria vaccines: RTS S/AS01 approved for P. falciparum prevention.
- Surveillance: Early detection and treatment to reduce transmission.
Conclusion
Mixed malaria infections pose significant diagnostic and treatment challenges. Timely, accurate diagnosis and appropriate treatment are essential to reduce morbidity and mortality. Continued research and better diagnostic tools are needed to manage mixed infections effectively.

