A case report: Myeloproliferative Neoplasms (MPNS) with CABG
Ms. Estharrani S1*, Ms. Kanimozhi A2, Ms.Pushpa3
1Nursing Superintendent, Kauvery Heartcity, Trichy, India
2OT Assistance Manager, Kauvery Heartcity, Trichy, India
3OT Incharge, Kauvery Heartcity, Trichy, India
Abstract
Coronary artery bypass grafting (CABG) is a major surgical operation where atheromatous blockages in a patients coronary arteries are bypassed with harvested venous or arterial conducts. The bypass restores blood flow to the ischemic myocardium, which in turn, restores the functions, viability and relieves angina symptoms.
Almost 4,00,000 CABG surgeries are performed each year making it the most commonly performed major surgical procedure, but surgeries have decreased, as the use of alternative options such as medical treatment and Percutaneous Coronary Intervention (PCI) have increased.
This activity highlights the role of the inter-professional team in the management of patients with CAD.
Myeloproliferative neoplasms are considered to increase the risk in cardiac surgery. In patients with myeloproliferative neoplasms, increased rates of perioperative infections and thromboembolic complications can be expected but studies analyzing the impact of myeloproliferative neoplasms on outcomes after cardiac surgery are lacking.
Background
Myeloproliferative neoplasms (MPNS) are hematopoietic stem cell neoplasms with a high risk of thrombosis, including acute myocardial infarction (AMI), however, outcomes after AMI have not been thoroughly characterized.
Case Presentation
A 55 years old male patient came to the emergency department with history of chest pain. He had previous history of ACS in 2020 and had undergone PCI to RCA and LAD. The recent admission was on 24/10/2023 when he had presented with complaints of chest pain. He was diagnosed as recent IW- PW- LW MI and was lysed with Inj. Streptokinase in the ER.
Echo indicated moderate LV dysfunction, grade I, diastolic dysfunction, Aortic sclerosis and mild concentric LVH. EF was 35%. His coronary angiogram revealed triple vessel disease and was advised CABG. However he needed hematologist and nephrologist opinions in view of abnormal hemoglobin and renal parameters. Hemoglobin, PCV and Creatinine were elevated.
Other symptoms
- Fatigue
- Weakness
- Weight loss
- Splenomegaly
- Brushing and bleeding
- Night sweats
- Pain in bones or joints
Symptoms pertaining to Polycythemia Vera
- Headache
- Dizziness
- Fatigue
- Blurred or double vision
Pre – Operative Lab Investigations
S No |
Investigation Name |
Patient Value |
Normal Value |
| 1 | Hemoglobin | 18.4g/dl | 13-17g/dl |
| 2 | Packed Cell Volume (PCV) | 57.7% | 40-54% |
| 3 | Total WBC count | 15200 cells/cumm | 4000-10000 |
Differential Count WBC |
|||
| 5 | Neutrophil | 83.8% | 40-75% |
| 6 | Lymphocyte | 8.6% | 25-40% |
| 7 | Monocyte | 5.6% | 1-8% |
| 8 | Eosinophil | 1.7% | 1-6% |
| 9 | Basophil | 0.3% | 0-1% |
| 10 | Red Blood Cell Count | 8.28 ml/10 | 4.5-6.0 |
| 11 | MCV | 69.6fl | 80-96 |
| 12 | MCH | 22.2pg | 27-32 |
| 13 | MCHC | 31.8 g/dl | 32-36 |
| 14 | Platelet Count | 366000cells/cum | 140000-400000 |
| 15 | Urea Serum | 30.5 mg/dl | 10-50 |
| 16 | Creatinine serum | 1.72mg/dl | 0.5-1.4 |
Activated Partial Thromboplastin Time |
|||
| 18 | Test | 140.2sec | 20.76-29.84 |
| 19 | Control | 25.3sec | |
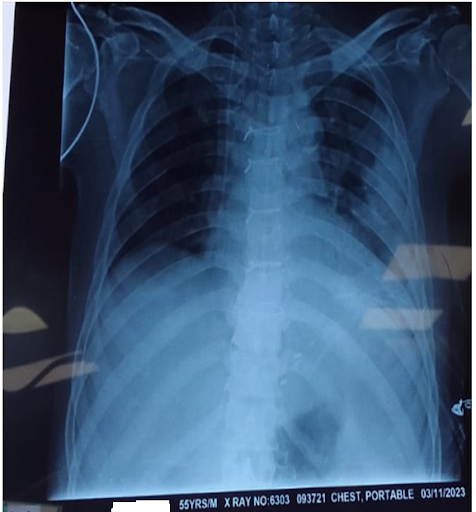
X-Ray
Serology
- HIV (1 and 2) Serum by ECLIA
- HCV antibody (ECLIA) – Non-reactive
- HBsAg (ECLIA) – Negative
USG Abdomen
- Moderate splenomegaly
- Bilateral renal parenchymal changes
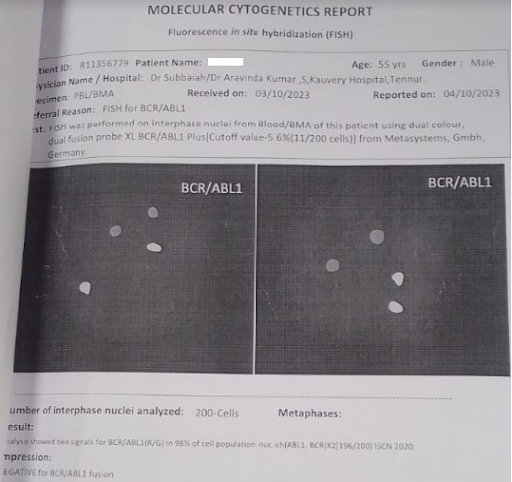
Molecular Cytogenetics Report
Negative for BCR/ABLI fusion
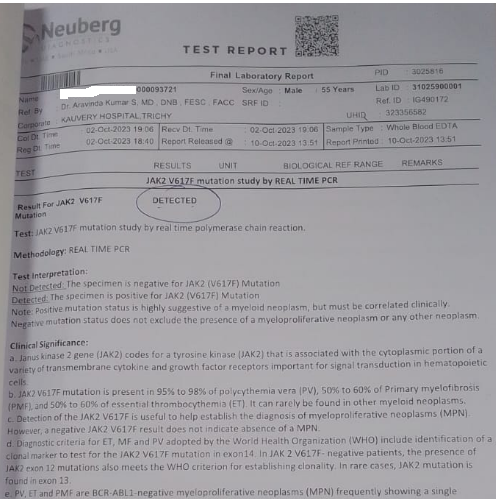
JAKV2 V617F Mutation Study by real time PCR
Result: Detected
In view of the above Myeloproliferative Neoplasm (MPNS) was diagnosed
But in view of the high-risk CAD, CABG was offered
Hematologist Oncologist Opinion
In view of the Laboratory findings, the patient was diagnosed with Polycythemia Rubra Vera and the patient was advised for
- Venesection of 450 ml if required
- Proceed for the surgery
- Post-surgery if no infection to restart with C. Hydroxyurea 500 mg
Nephrologist Opinion
- Patient can be taken for CABG
- Moderate High risk
- Kindly avoid NSAID/Aminoglycosides to avoid intraop hypotension
- I/O chart to be strictly monitored
- Fluids 1.5L/day
- To review in postop period
Hence patient was taken up for CABG.
Operational notes
- LAD artery was 1.75mm diameter. LIMA was anastomosed to end to side with 8-0 prolene sutures.
- OM1 artery was 1.5mm diameter with mild plaque. The segment of the saphenous vein was anastomosed end to side with 8-0 prolene suture and the graft flushed well. The proximal end of the graft was anastomosed to the aorta with 6-0 prolene sutures.
- PDA artery was 1.5 mm diameter with mild plaque. The segment of the saphenous vein was anastomosed end to side with 8-0 prolene sutures and the graft was flushed well. The proximal end of the graft was anastomosed to the aorta with 6-0 prolene sutures.
- Mild line sternotomy division of thymus. Peri-cardiotomy, systemic heparinisation after harvesting of conducts. Grafting done as mentioned above with tissue stabilizers. Hemostasis and sternal closure with mediastinal and left pleural drains.
Post-Operative Management
On 30/10/2023 – 0 POD
On 02:00pm patient received from HCOT with ambu ventilation and then connected to mechanical ventilation. Pre-lateral air entry equal.
SIMV (PC+PS) with FW2 – 100%, RR – 16, PC – 15, PS – 10, PEEP – 5 in ET size of 8.5mm.
Patient chest drain was-290ml
Urine output-870ml
Supports are Inj. Adrenaline 0.1ml/hr – 2ml/hr
Inj. Noradrenaline 1.1ml/hr – 5.5ml/hr
Inj. NTG 0.1ml/hr
Blood withdrawal done-2 units (350ml + 350ml)
On 31/10/2023 I POD
Patient on extubation done connected to O2 mask
Ryles tube removed.
Chest drain – 420ml
Urine output – 1615ml
Supports are Inj. Adrenaline – 1ml/hr
Inj. Noradrenaline – 5ml/hr
Inj. Lasix – 4ml/hr
On 01/11/2023II POD
No chest drain
Urine output – 1480ml
Supports are Inj. Adrenaline – 1ml/hr
Inj. Noradrenaline – 5ml/hr
Inj. Lasix – 4ml/hr
Inj. Dopamine – 5ml/hr
On 02/11/2023 III POD
S/P left side ICD insertion done. Urea – 109, Creatinine – 3.36 so, advised to get nephrologists opinion sir ordered to do I/O chart fluid 1.5mll/day, to take a medication
Tab. Nefrosave – BD
Tab. Nodosis – BD to taper Lasix.
On 03/11/2023 IVPOD
On 4th POD patient antibiotic was changed to Inj. Magnex 1.5g. Supports were stopped.
Post-Operative Investigation
S N |
Investigations |
Patient Value |
Normal Value |
| 1 | Hemoglobin | 9.8g/dl | 13-17g/dl |
| 2 | Packed Cell Volume | 30.2% | 40-54% |
| 3 | Urea Serum | 119mg/dl | 10-50mg/dl |
| 4 | Creatinine Serum | 3.43mg/dl | 0.5-1.4 |
| 5 | Sodium Serum | 134meg/l | 136-145 |
| 6 | Potassium Serum | 4.02mmol/l | 3.5-5 |
Post OP ECHO
- S/P CABG
- Moderate LV dysfunction
- No Pericardial effusion/clot
Discharge Medication Advice
S No |
Medications |
Dose |
Frequency |
| 1 | Tab. Clavix AS | 150mg | 0-1-0 |
| 2 | Tab. Aztor | 40mg | 0-0-1 |
| 3 | Tab. Ivabrad | 5mg | 1-0-1 |
| 4 | Tab. Prolomet XL | 12.5mg | 1-0-0 |
| 5 | Tab. Flavedon MR | 35mg | 1-0-1 |
| 6 | Tab. Dytor | 10mg | 1-1-0
(08:00am and 04:00pm) |
| 7 | Cap. Pan D | 40mg | 1-0-1 |
| 8 | Tab. Dolo | 650mg | 1-1-1 |
| 9 | Cap. Becosules | – | 0-1-0 |
| 10 | Tab. Alprax | 0.5mg | 0-0-1 |
| 11 | Tab. Dulcolax | 5mg | 0-0-1 |
| 12 | Tab. Augmentin | 625mg | 1-0-1 ×5 Days |
| 13 | Tab. Bifilac | 1-0-1 | |
| 14 | Syp. Mucolite | 10ml | 1-0-1 |
| 15 | Syp. Ulgel | 10ml | 1-1-1 |
| Dr. Balaji Advice | |||
| 1 | Tab. Nefrosave | – | 1-0-1 |
| 2 | Tab. Nodosis | 500mg | 1-0-1 |
We scheduled his review after 2 weeks from the discharge date and he was advised to follow all instructions at his home.
Conclusion
Patient with coronary artery disease along with myeloproliferative neoplasm- polycythemia in thin instance – have higher risk of in hospital death as there is a higher risk of thrombosis post procedure CABG > PCI.
More case reports are needed to understand the significant of in-hospital mortality in this subset group of patients.

