A case study on Heart Transplantation
Nalini Sivakumar*
Dietician, Department of Clinical Nutrition & Dietetics, Kauvery Hospital, Chennai
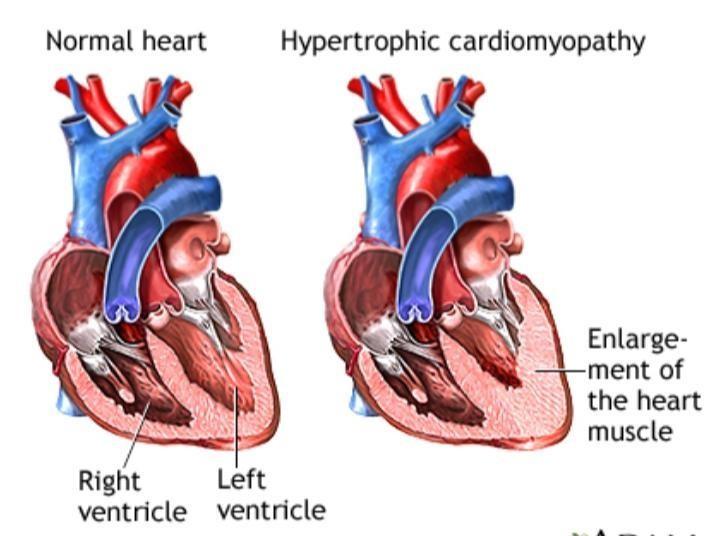
Background
Hypertrophic cardiomyopathy (HCM) is a condition in which the heart muscle becomes thick. Often, only one part of the heart is thicker than the other parts. The thickening can make it harder for blood to leave the heart, forcing the heart to work harder to pump blood. It also can make it harder for the heart to relax and fill with blood.
Etiology
Cardiomyopathy is most often passed down through families (inherited). It is thought to result from defects in the genes that control heart muscle growth. Younger people are likely to have a more severe form of hypertrophic cardiomyopathy. However, the condition is seen in people of all ages.
Sign & Symptoms
- Chest pain, especially during exercise
- Fainting, especially during or just after exercise or exertion. Heart murmur, which a health care provider might detect while listening to the heart
- Sensation of fast, fluttering or pounding heartbeats (palpitations)
- Shortness of breath, especially during exercise.
Common causes of Heart Failure
- Heart attack (myocardial infarction or MI)
- Viral infection of the heart muscle- Myocarditis
- High blood pressure
- Heart valve disease (Eg: Rheumatic Heart Disease)
- Heart defects present at birth (congenital heart disease)
- Irregular heartbeats (arrhythmia)
- High blood pressure in the lungs (pulmonary hypertension)
- Alcoholism or drug abuse
- Heart Disease secondary to Chronic lung diseases, such as emphysema or chronic obstructive pulmonary disease (COPD)
- Heart muscle is enlarged, thick, and stiff (cardiomyopathy)
Case scenario
A 35-year-old female, had been diagnosed to have hypertrophic cardiomyopathy. She was experiencing breathlessness on exertion (NYHA-III) from 2017. Echo revealed severe left ventricular dysfunction. Hence patient was worked up and admitted for heart transplant.
- Anthropometric data
| Height | 151cm |
| Weight | 53kg |
| Body mass index | 23.2kg/m2 (according to WHO BMI classification
patient falls under healthy weight category) |
| Ideal body weight (IBW) | {height (m2)x19} to {height (m2x24)} =43 to 55kg |
- Biochemical parameters
| Parameter | 4/9/22 | 5/9/22 | 6/9/22 | 7/9/22 | 8/9/22 | 9/9/22 | 10/9/22 | 11/9/22 | 12/9/22 | 13/9/22 |
| Urea | 17.5 | 18.4 | 20.7 | 35.9 | 34.9 | 29.8 | 35.6 | 46.7 | 41.4 | 26.1 |
| Creatinine | 0.54 | 0.57 | 0.42 | 0.50 | 0.50 | 0.53 | 0.69 | 0.83 | 0.73 | 0.44 |
| Na | 135 | 141.7 | 132.7 | 132.8 | 135.5 | 133.5 | 133.5 | 133.8 | 132.7 | 134.1 |
| Potassium | 4.21 | 3.94 | 5.04 | 3.91 | 3.84 | 4.15 | 4.23 | 4.32 | 3.91 | 4.47 |
| Cl 2 | 108.1 | 115.1 | 106.4 | 103 | 103.8 | 103.7 | 104.7 | 102.2 | 102 | 104.8 |
| HCo3 | 15.6 | 18.5 | 19.8 | 18.3 | 17 | 19.0 | 20.01 | 20.6 | 16.6 | 19.6 |
| Bilirubin-T | 0.38 | 1.63 | - | 0.64 | - | - | 0.63 | - | | |
| Bilirubin-D | 0.16 | 0.41 | - | 034 | - | - | 0.35 | - | | |
| Bilirubin- I | 0.22 | 0.72 | - | 0.30 | - | - | 0.28 | - | | |
| SGOT | 24.6 | 103.7 | - | 31.9 | - | | 19.5 | | | |
| SGPT | 15.6 | 27.9 | - | 22.2 | - | | 23.1 | | | |
| T. Protein | 6.84 | 5.60 | - | 5.30 | - | | 4.79 | | | |
| Albumin | 4.19 | 3.84 | 3..77 | 3.55 | 3.23 | 3.09 | 3.05 | 3.43 | 3.44 | |
| Globulin | 2.65 | 1.76 | | 1.75 | | | 1.74 | | | |
| Calcium | 8.47 | 7.62 | | 8.32 | | | 7.73 | | 7.99 | 7.71 |
| Al phosphatase | 18.0 | 8.3 | | 11.5 | | | 18.0 | | | |
| Phosphatase | 4.60 | 1.19 | 3.42 | 1.18 | | | 1.48 | | 2.03 | |
| Hb | 10.3 | 10 | 9.0 | 8.8 | 8.6 | 8.4 | 7.8 | 9.4 | 11.3 | 10.7 |
| PCV | 32.8 | 30.6 | 27.9 | 26.7 | 25.9 | 25.2 | 23.4 | 28.6 | 34.9 | 32.5 |
| WBC | 6000 | 15300 | 188001 | 19600 | 12900 | 8800 | 11800 | 11900 | 12700 | 13830 |
| Platelet count | 247000 | 164000 | 113000 | 117000 | 118000 | 118000 | 142000 | 138000 | 188000 | 265400 |
| GGT | 12.1 | 18.5 | | | | | | | | |
| A/G Ratio | 1.6 | 2.2 | | | | | | | | |
| Parameters | 14/9/22 | 15/9/22 | 16/9/22 | 17/9/22 | 18/9/22 | 19/9/22 | 20/9/22 | 22/9/22 | 24/9/22 | 26/9/22 |
| Urea | 31.3 | 46.4 | 44.9 | 49.2 | 0.47 | 35.6 | 46.7 | 41.4 | ||
| Creatinine | 0.54 | 0.60 | 0.62 | 0.58 | 0.66 | 0.69 | 0.83 | 0.73 | ||
| Na | 132.8 | 132.4 | 132.5 | 131.0 | 134.1 | 133.5 | 133.8 | 132.7 | ||
| Potassium | 4.49 | 4.57 | 4.51 | 4.50 | 103.7 | 4.23 | 4.32 | 3.91 | ||
| Cl2 | 103.7 | 102.6 | 102.3 | 101.0 | 19.6 | 104.7 | 102.2 | 102 | ||
| HCo3 | 18 | 15.9 | 14.8 | 17.5 | 1.76 | 20.01 | 20.6 | 16.6 | ||
| Bilirubin-T | 0.55 | 0.63 | – | |||||||
| Bilirubin-D | 0.25 | 0.35 | – | |||||||
| Bilirubin- I | 0.30 | 0.28 | – | |||||||
| SGOT | 14.0 | 30.7 | ||||||||
| SGPT | 23.0 | 157.2 | 82.2 | |||||||
| T. Protein | 4.72 | 5,85 | ||||||||
| Albumin | 36 | 3.29 | 2.90 | 3.85 | 3.95 | |||||
| Globulin | 1.82 | 1.90 | ||||||||
| Calcium | 7.82 | 7.94 | 7.93 | 7.75 | 8.21 | 8.22 | 8.62 | 9.14 | 8.68 | |
| Al phosphatase | 51.0 | |||||||||
| Phosphatase | 2.72 | 3.00 | 2.90 | 2.67 | 2.36 | 2.18 | 2.20 | 3.67 | 3.53 | |
| Hb | 9.1 | 8.8 | 9.6 | 9.5 | 9.8 | 8.6 | 8.4 | 8.6 | ||
| PCV | 27.3 | 27.6 | 29.7 | 28.8 | 29.5 | 26.6 | 25.6 | 26.0 | ||
| WBC | 15900 | 14800 | 16800 | 15000 | 13700 | 11200 | 5900 | 7200 | ||
| Platelet count | 164000 | 200000 | 236000 | 209000 | 205000 | 178000 | 176000 | 220000 | ||
| GGT | 58.5 | 2.1 | ||||||||
| A/G Ratio |
- Clinical data
| Chief complaints | Tiredness, Palpitation, Shortness of breath and fatigue |
| Diagnosis | Hypertrophic cardiomyopathy/ CCF |
| History of past illness | Nil |
| Plan of treatment | Heart transplantation |
| Nutrition-focused physical findings | Appearance (eyes, hair, nails, skin, lips & mouth were found to be normal)
No presence of ascites and edema |
Dietary Habits – Non-vegetarian
Food Allergy – Nil
- Diet History
| SUBJECTIVE GLOBAL ASSESSMENT | |
| Rating | B |
| Category | Well nourished but at risk |
Medical Nutrition Therapy
Energy: To provide adequate amount of energy to meet Post -surgery requirements and to maintain optimal nutrition status.
Carbohydrate: To provide adequate amount of carbohydrates to replenish energy reserves.
Protein: To provide high protein diet for healing and to prevent PEM.
Fat: To provide moderate amount of fat to aid in optimal growth.
Micronutrients: Micro nutrients are to provided as per RDA to maintain physiological functions and pre operatively we prescribed oral nutrition supplement.
Nutritional plan
ENERGY : 2000kcals@30kcals/kgIBW
CARBOHYDRATES : 60% of total calories.
PROTEIN : 82g@1.5g/kgIBW
FAT : 25% From Total calories
SALT : 6gms/Day
VITAMINS : As per RDA
MINERALS : As per RDA
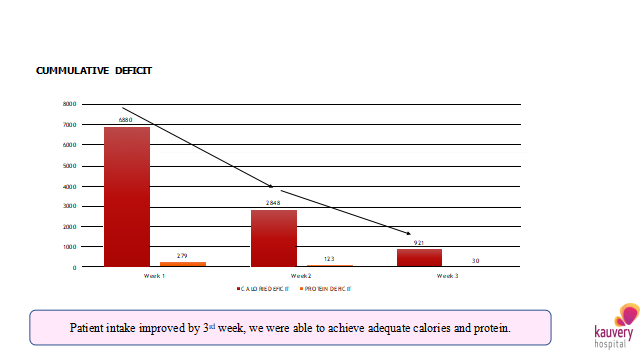
POST OPERATIVE NUTRITIONAL INTERVENTION
| Days | Date | Type of diet | Energy (kcals) | Protein (g) | Remarks |
| Day 0 | 4/09/22 | On surgery | | | |
| Day1 | 5/09/22 | NPO | 0 | 0 | Post operative |
| Day 2 | 6/09/22 | RT feed initiated @150ml 3rd hrly –
total volume:300ml +oral clear liquid diet |
527 | 33 | Pt well tolerated clear liquids |
| Day 3 | 7/09/22 | RT feed stopped, oral High Protein soft diet initiated +1.5lit f/R | 287 | 28 | Initiated oral nutrition supplement |
| Day 4 | 8/09/22 | High Protein soft diet | 383 | 28 | Intake was poor diet modified |
| Day 5 | 9/09/22 | High Protein soft diet | 869 | 56 | Intake was getting better |
| Day 6 | 10/09/22 | High Protein normal diet diet initiated | 1376 | 78 | Intake is improved |
| Day 7 | 11/09/22 | Oral high Protein high fibre diet initiated | 665 | 39 | Intake was poor due to vomiting & constipation |
| Day 8 | 12/09/22 | High Protein soft diet | 913 | 33 | Diet modified |
| Day 9 | 13/09/22 | High Protein normal diet | 1095 | 58 | Intake is fair |
| Day 10 | 14/09/22 | High Protein diet | 847 | 44 | Intake was poor due to vomiting |
| Day 11 | 15/09/22 | High Protein diet | 936 | 49 | NPO, plan biopsy |
| Day 12 | 16/09/22 | High Protein normal diet | 1185 | 61 | Intake is improved |
| Day14 | 17/09/22 | High Protein normal diet | 1449 | 93 | Intake is improved |
| Day 15 | 18/09/22 | High Protein normal diet | 1141 | 75 | Pt had c/o vomiting, diet modified accordingly |
| Day 17 | 20/09/22 | High Protein normal diet | 1221 | 59 | Pt had poor appetite, compromised and encouraged to take ONS |
| Day 18 | 21/09/22 | High Protein normal diet | 1411 | 70 | Intake was getting better |
| Day 19 | 22/09/22 | High Protein Normal diet | 1585 | 79 | Intake was better |
| Day 20 | 23/09/22 | High Protein normal diet | 1648 | 93 | Intake improved |
| Day 21 | 24/09/22 | High Protein normal diet | 1900 | 113 | Intake improved |
| Day 22 | 25/09/22 | High Protein normal diet | 1857 | 86 | Intake was adequate, pt took ONS supplements |
| Day23 | 26/09/22 | High Protein normal diet | 275 | 5 |
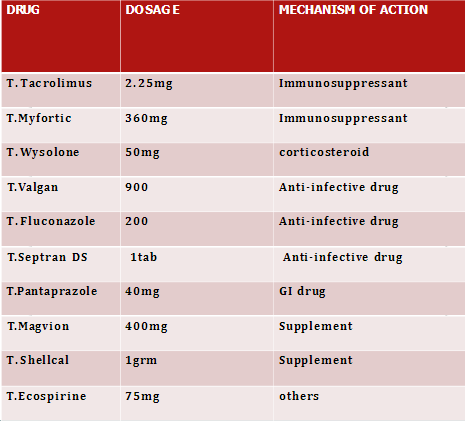
What is Tacrolimus test?
The Tacrolimus test is used to measure the amount of drug in the blood to determine whether the concentration has reached a therapeutic level and it is below the toxic level.
- Normal Tac level: 5- 10 ng/ ml
The level of Tacrolimus in the blood must be maintained within a narrow therapeutic range.
- If the concentration is too low, organ rejection may occur.
- If it is too High then the person may experience symptoms associated with toxicity.
| POD | Tacrolimus
levels ng/ml |
Dosage
(morning) mg |
Dosage
(Evening) mg |
| Pod 4 | 4.7 | 0.5 | 0.5 |
| Pod 5 | 4.8 | 0.5 | 1 |
| Pod 6 | 7.7 | 0.75 | 1 |
| Pod 7 | Not done | 0.75 | 1 |
| Pod 8 | 7.4 | 0.75 | 1 |
| Pod 9 | 7.2 | 1.0 | 1.25 |
| Pod 10 | Not done | 1.0 | 1.25 |
| Pod 11 | 6.9 | 1.0 | 1.5 |
| Pod 12 | Not done | 1.5 | 1.5 |
| Pod 13 | 7.6 | 1.5 | 1.5 |
| Pod 14 | Not done | 1.75 | 2 |
| Pod 15 | 10.9 | 1.75 | 2 |
| Pod 16 | Not done | 1 75 | 2 |
| Pod 17 | 9.4 | 1.75 | 2.25 |
| Pod 18 | Not done | 2.25 | 2.25 |
| Pod 19 | 12.1 | 2.25 | 2.25 |
| Pod20 | Not done | 2.25 | 2.25 |
| Pod 21 | 18.7 | 2.25 | Not given |
| Pod 22 | Not done | 2 | 2 |
| Pod 23 | 16.2 | 2 | 1.75 |
| Pod 24 | Not done | 3 | Not given |
Post operative medications
Summary
A 35year old female, who was known to have Hypertrophic cardiomyopathy, started experiencing NYHA- III symptoms from 2017. She completed all her workups for heart and lung transplant on April 2022. Patient got suitable organ alert call on 4/09/2022. Patient underwent Orthotropic heart transplant Surgery on 4/09/2022. After procedure the she was shifted to ICU with minimal inotropic and nitrous oxide support. During the hospital stay the nutritional management was planned according to the patient condition. Post operatively RT feed was initiated on pod 3, RT feed was stopped and oral liquid diet initiated oral nutritional supplement was prescribed. Patient tolerated oral feeds well and diet stepped up to high Protein soft diet. Patient had some Gastric issues diet modification was done. Patient intake was gradually improved, on discharge patient and family was educated High Protein, low fat neutropenic diet.

