Renukadevi
Senior Dietician, Department of Clinical Nutrition & Dietetics, Kauvery Hospital, Chennai.
Acute Pancreatitis: the nutrition care process
Background
Acute pancreatitis is a condition where the pancreas becomes inflamed (swollen) over a short period of time. The pancreas is a small organ, located behind the stomach, that helps with digestion. Pancreatitis can occur as acute pancreatitis – meaning it appears suddenly and lasts for days. Some people develop chronic pancreatitis, which is pancreatitis that occurs over many years.
Sign and Symptoms
Acute pancreatitis signs and symptoms include:
- Upper abdominal pain
- Abdominal pain that radiates to your back
- Tenderness when touching the abdomen
- Fever
- Rapid pulse
- Nausea
- Vomiting.
Pancreatitis occurs when digestive enzymes become activated while still in the pancreas, irritating the cells of the pancreas and causing inflammation. Conditions that can lead to acute pancreatitis include:
- Gallstones
- Alcoholism
- Certain medications
- High triglyceride levels in the blood (hypertriglyceridemia)
- High calcium levels in the blood (hypercalcemia), which may be caused by an overactive parathyroid gland (hyperparathyroidism)
- Pancreatic cancer
- Abdominal surgery
- Cystic fibrosis
- Infection
- Injury to the abdomen
- Obesity
- Trauma
- Endoscopic retrograde cholangiopancreatography (ERCP), a procedure used to treat gallstones, also can lead to pancreatitis.
Case Scenario
A 35-year-old male was admitted with complaints of epigastric pain and abdominal distension, along with 2 episodes of vomiting. He also had shortness of breath.
USG abdomen showed pancreatitis. Patient was admitted to the ICU for further management.
Nutrition Care Process
1. Anthropometric Data
| Height | 165cm |
| Weight | 72kg |
| Body Mass Index | 26.4kg/m2
According to WHO BMI classification patient falls under overweight category |
| Ideal Body Weight | 60-65 kg |
2. Biochemical Data
| Biochemial Parameters | 9/6/22 | 10/6/22 | 11/6/22 | 13/6/22 | 14/6/22 | 17/6/22 | 18/6/22 | 19/6/22 | 24/6/22 | 26/6/22 | |
| Urea | 108.5 | 80 | 47.5 | 47.4 | 54.2 | 51.1 | 39.1 | 14.4 | 18.2 | ||
| creatinine | 2.16 | 1.35 | 0.87 | 0.79 | 0.62 | 0.57 | 0.52 | 0.43 | 0.42 | ||
| Na | 132.7 | 137.2 | 135.6 | 134.5 | 140.6 | 140.4 | 144.2 | 136.7 | |||
| K+ | 4.71 | 4.14 | 3.91 | 4.09 | 5.12 | 6.18 | 4.64 | 4.42 | |||
| cl2 | 97.6 | 105.3 | 101.4 | 105 | 109.8 | 104.6 | 98.4 | ||||
| HCO3 | 14 | 16.3 | 19.6 | 25.2 | 19 | 19.5 | 25.2 | ||||
| Sr. uric acid | 7.79 | 6.06 | 6.05 | 6.6 | 7.17 | 6.92 | 2.71 | ||||
| T.cholesterol | 156.5 | ||||||||||
| Bilirubin – T | 7.41 | 7.36 | 4.15 | 3.94 | 4.1 | 1.34 | 0.69 | 0.68 | |||
| Bilirubin – D | 5.41 | 5.36 | 2.02 | 2.94 | 3.24 | 0.38 | 0.39 | 0.42 | |||
| Bilirubin – I | 2 | 2 | 2.13 | 1 | 0.86 | 0.96 | 0.3 | 0.26 | |||
| SGOT (AST) | 81.2 | 84.9 | 72.9 | 58.9 | 65 | 52.7 | 47.4 | 36.9 | |||
| SGPT | 25.9 | 38.5 | 34.85 | 31.8 | 28.6 | 21.4 | 18.4 | 16.5 | |||
| T. Protein | 5.45 | 5.09 | 72 | 5.34 | 6.03 | 5.64 | 5.44 | 6.39 | |||
| Albumin | 2.83 | 2.6 | 2.41 | 2.53 | 2.74 | 2.2 | 2.53 | 3.1 | |||
| Globulin | 2.62 | 2.49 | 3.31 | 2.81 | 3.29 | 3.44 | 2.91 | 3.29 | |||
| Calcium | 5.35 | 6.77 | 7.22 | 7.48 | 6.61 | 6.96 | 7.97 | ||||
| Sr.Al. Phosphatase | 43 | 39.2 | 60.4 | 64 | 121.4 | 70.7 | 40.3 | ||||
| Phosphorus | 2.9 | 1.39 | 2.55 | 3.73 | 2.84 | 2.16 | 3.76 | ||||
| Magnesium | 1.87 | ||||||||||
| CRP | 553.43 | 336.89 | 364.72 | 359.44 | |||||||
| Amylase | 192 | ||||||||||
| Lipase | 589.2 | 59.5 | 8.1 | ||||||||
3. Clinical Data
| Chief complaints | Abdominal pain, vomiting, loose stools, tiredness |
| Diagnosis | Acute pancreatitis
Multiple organ dysfunction syndrome |
| History of past illness | Nil |
| Plan of treatment | Medical management |
| Nutrition-focused physical findings |
|
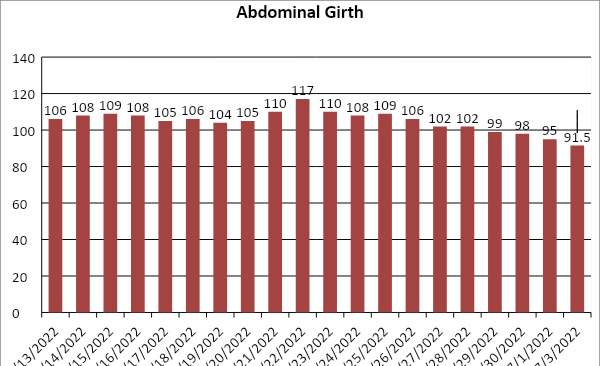
Fig. 1. Graphical Presentation of Abdominal Girth.
4. Diet History
| Diet Habit | Ova – vegetarian |
| Food allergies | Nil |
Subjective Global Assessment
| Rating | B |
| Category | Well-nourished but at risk |
PES Statement
| Problem | Etiology | Symptom | ||
| Altered GI function | Related to | Underlying medical condition of the patient (ASBO) | As evidenced by | Abdominal pain, vomiting and loose stools |
Medical Nutrition Therapy
| Energy | To provide adequate amount of energy to meet the requirements and to maintain optimal nutritional status |
| Carbohydrates | To provide adequate amounts of carbohydrates to replenish energy reserves |
| Protein | To provide a high protein diet to aid in tissue repair and prevent weight loss |
| Fat | To provide moderate amount of fat to maintain normal bodily function |
| Fluids | Adequate fluids should be provided to prevent dehydration |
| Micronutrients | Micronutrients are to be provided as per RDA to maintain physiological functions |
Nutrition Prescription
| Energy | 1600 @25kcal/kg IBW |
| Carbohydrates | 60% of total calories |
| Protein | 65 @1 g/kg IBW Followed by 1.5 g/kg IBW |
| Fat | 20% of total calories |
| Fluids | Liberal |
| Salt | 3 g/day |
| Vitamins | As per RDA |
| Minerals | As per RDA |
Diet History
| Days | Date | Type of Diet | Energy (Kcal) | Protein (G) | Remarks |
| Day 01 | 09-06-22 | Renal, clear liquid diet; total volume: 750 ml | 112.5 | 1.8 | Oral soft solid bland diet initiated |
| Day 02 | 10-06-22 | Oral clear liquids; total volume: 1200 ml | 180 | 3 | Diet was modified to liquid diet since the patient had c/o loose stools – 2 episodes |
| Day 03 | 11-06-22 | Oral clear liquids; total volume: 690 ml | 103.5 | 1.7 | |
| Day 04 | 12-06-22 | Oral clear liquids; total volume: 520 ml | 78 | 1.3 | |
| Day 05 | 13-06-22 | Oral clear liquids; total volume: 450 ml | 67.5 | 1.1 | |
| Day 06 | 14-06-22 | Oral clear liquids; total volume: 760 ml | 114 | 1.9 | Suggested ONS 4 times a day (semi-elemental formula) |
| ONS 4 times in a day | 612 | 24 | |||
| Total | 726 | 25.9 | |||
| Day 07 | 15-06-22 | Oral clear liquids; total volume: 310 ml | 46.5 | 0.7 | |
| ONS 4 times a day | 612 | 24 | Initiated RTH by ICU team | ||
| Total | 658.5 | 24.7 | |||
| Day 08 | 16-06-22 | Oral clear liquids; total volume: 510 ml | 76.5 | 1.2 | |
| RTH @ 20 ml/h; total volume: 290 ml | 435 | 18 | |||
| Total | 511.5 | 2.2 | |||
| Day 09 | 17-06-22 | Oral clear liquids; total volume: 300 ml | 99 | 1.6 | |
| RTH @ 20 ml/h; Total volume: 440 ml | 660 | 27 | Oral egg scrambled trail | ||
| Total | 759 | 28.6 | |||
| Day 10 | 18-06-22 | Oral clear liquids; total volume: 285 ml | 42.7 | 0.7 | |
| RTH @ 30 ml/h; total volume: 460 ml | 690 | 29 | |||
| Total | 732.7 | 29.7 | |||
| Day 01 | 09-06-22 | Renal, clear liquid diet; total volume: 750 ml | 112.5 | 1.8 | Oral soft solid bland diet initiated |
| Day 02 | 10-06-22 | Oral clear liquids; total volume: 1200 ml | 180 | 3 | Diet was modified to liquid diet since the patient had c/o loose stools – 2 episodes |
| Day 03 | 11-06-22 | Oral clear liquids; total volume: 690 ml | 103.5 | 1.7 | |
| Day 04 | 12-06-22 | Oral clear liquids; total volume: 520 ml | 78 | 1.3 | |
| Day 05 | 13-06-22 | Oral clear liquids; total volume: 450 ml | 67.5 | 1.1 | |
| Day 06 | 14-06-22 | Oral clear liquids; total volume: 760ml | 114 | 1.9 | suggested ONS 4 times a day (semi-elemental formula) |
| ONS 4 times a day | 612 | 24 | |||
| Total | 726 | 25.9 | |||
| Day 07 | 15-06-22 | Oral clear liquids; total volume: 310 ml | 46.5 | 0.7 | |
| ONS 4 times a day | 612 | 24 | Initiated RTH by ICU team | ||
| Total | 658.5 | 24.7 | |||
| Day 08 | 16-06-22 | Oral clear liquids; total volume: 510 ml | 76.5 | 1.2 | |
| RTH @ 20 ml/h; total volume: 290 ml | 435 | 18 | |||
| Total | 511.5 | 2.2 | |||
| Day 09 | 17-06-22 | Oral clear liquids; total volume: 300 ml | 99 | 1.6 | |
| RTH @ 20 ml/h; total volume: 440 ml | 660 | 27 | Oral egg scrambled trail | ||
| Total | 759 | 28.6 | |||
| Day 10 | 18-06-22 | Oral clear liquids; total volume: 285 ml | 42.7 | 0.7 | |
| RTH @ 30 ml/h; Total volume: 460 ml | 690 | 29 | |||
| Total | 732.7 | 29.7 | |||
| Day 11 | 19-06-22 | Oral clear liquids; total volume: 800 ml | 120 | 2 | |
| RTH @ 30 ml/hr; Total volume: 310ml | 465 | 19 | Oral semi-solid diet initiated | ||
| Total | 585 | 21 | |||
| Day 12 | 20-06-22 | RTH @ 30 ml/h; total volume: 760 ml | 1140 | 47 | |
| Oral semi-solid diet | 83 | 4 | |||
| Total | 1123 | 51 | |||
| Day 13 | 21-06-22 | Oral clear liquids; total volume: 300 ml | 45 | 0.7 | |
| RTH @ 30 ml/h; total volume: 460 ml | 690 | 29 | Suggested TPN | ||
| Total | 735 | 29.7 | |||
| Day 14 | 22-06-22 | TPN initiated @ 30 ml/h followed by 60 ml/h | 1600 | 75 | |
| RTH @ 30 ml/h; total volume: 870 ml | 1305 | 54.5 | |||
| Oral semi solid diet | 157 | 10 | |||
| Total | 3062 | 139.5 | |||
| Day 15 | 23-06-22 | TPN @ 60 ml/h; total volume: 1320 | 1408 | 66 | Suggested RT feed @200 ml 4th hourly |
| RT feed @200 ml 4th hourly | 408 | 16 | |||
| Oral | 162 | 12 | |||
| Total | 1978 | 94 | |||
| Day | 24-06-22 | TPN @ 60 ml/h; total volume: 1080 | 1204 | 55 | |
| 16 | RT feed @200ml 4th hourly; total Volume: 500ml | 418 | 17 | ||
| Oral semi solid diet | 83 | 4 | |||
| Total | 1705 | 76 | |||
| Day 17 | 25-06-22 | TPN @ 60 ml/h; Total volume: 1380 | 1538 | 70 | |
| RT feed @200 ml 4th hourly; Total Volume: 200 ml | 334 | 14 | |||
| Oral semi solid diet | 261 | 17 | |||
| Total | 2133 | 101 | |||
| Day 18 | 26-06-22 | TPN @ 60ml/hr; Total volume: 1320ml | 1473 | 67 | |
| RT feed @200ml 4th hourly; Total Volume: 700ml | 714 | 28 | |||
| oral semi solid diet | 200 | 8.65 | |||
| Total | 2387 | 103.05 | |||
| Day 19 | 27-06-22 | TPN @ 60ml/hr; Total volume: 1260ml | 1406 | 64 | |
| RT feed @200ml 4th hourly; Total Volume: 700ml | 714 | 28 | |||
| oral semi solid diet | 157 | 10.45 | |||
| TOTAL | 2277 | 102.45 | |||
| Day 20 | 28-06-22 | TPN @ 60ml/hr; Total volume: 1740ml | 1272 | 59 | |
| RT feed @200ml 4th hourly; Total Volume: 500ml | 510 | 20 | |||
| oral semi solid diet | 29 | 15 | |||
| TOTAL | 2074 | 94 | |||
| Day 21 | 29-06-22 | TPN @ 60ml/hr; Total volume: 660ml | 726 | 33 | |
| RT feed @200ml 4th hourly; Total Volume: 600ml | 408 | 16 | |||
| oral semi solid diet | 474 | 24 | |||
| TOTAL | 1608 | 73 | |||
| Day 22 | 30-06-22 | TPN @ 60ml/h; Total volume: 280ml | 308 | 14 | |
| RT feed @200 ml; Total Volume: 1050 ml | 1050 | 40 | |||
| oral semi solid diet | 505 | 23 | suggested to Stop TPN and encouraged oral and RT feed only; modified RT feed to 5 times in a day | ||
| TOTAL | 1863 | 79 | |||
| Day 23 | 01-07-22 | RT feed @200 ml; Total volume: 800 ml | 800 | 38 | |
| Oral High protein diet | 692 | 41 | |||
| TOTAL | 1492 | 73 | |||
| Day 24 | 02-07-22 | Oral High protein soft diet | 1538 | 75 | RT stopped |
| Day 25 | 03-07-22 | Oral High protein soft diet | 1600 | 75 | |
| Day 26 | 04-07-22 | Discharge diet issued |
Fig, 2. Graphical presentation of total parenteral nutrition.
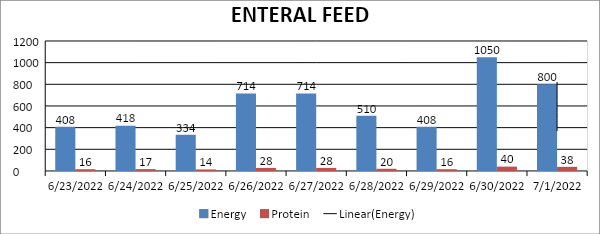
Fig. 3. Graphical presentation of enteral nutrition.
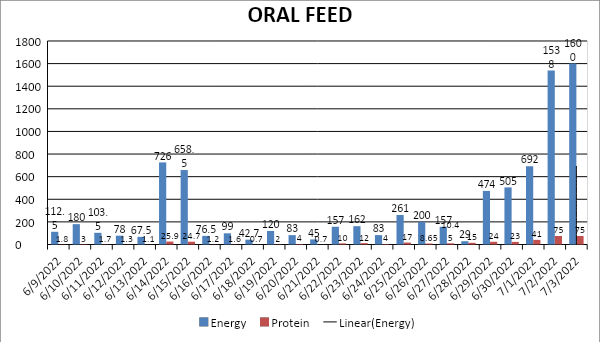
Fig. 4. Graphical presentation of oral feeds
Conclusion
A 35-years-aged male was admitted with complaints of epigastric pain and abdominal distension, along with episodes of vomiting. He also had shortness of breath at the time of admission. The patient was admitted in the ICU for further management and started on HFNC 60 litre. Necessary investigations were done. Elevated blood parameters were seen. Echo showed LV dysfunction. USG abdomen showed acute pancreatitis. The abdominal girth measurement was above 102cm. Medical and nutritional management was given accordingly.
Initially clear liquid diet and semi elemental formula was prescribed as the patient had episodes of vomiting and loose stools. Total Parenteral Nutrition was given to improve the nutritional status of the patient followed by Ryles tube feeds and transited to oral soft solid high protein diet. The patient’s condition gradually improved in nutritional status. The patient and family were educated on High protein diet at the time of discharge.

