Acute Respiratory Distress Syndrome: A case report
Mercy Ezhil Rani*
Clinical Educator, Kauvery Hospital, Hosur
Abstract
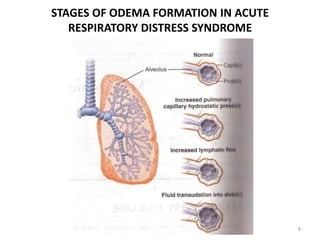
Acute respiratory distress syndrome (ARDS) is a common cause of respiratory failure in critically ill patients and is defined by the acute onset of non-cardiogenic pulmonary oedema, hypoxaemia and the need for mechanical ventilation. ARDS occurs most often in the setting of pneumonia, sepsis, aspiration of gastric contents or severe trauma and is present in ~10% of all patients in intensive care units worldwide. To those ends, the investigators recorded admissions over 4 weeks to 459 ICUs in 50 countries over 5 continents including 29,144 patients. In total, 3022 (10.4%) cases fulfilled ARDS criteria, including almost a quarter of those supported with invasive ventilation. There are reports of 30–40% mortality up until the 1990s, but over the past 20 years, there has been a significant decrease in the mortality rate, even for severe ARDS. These accomplishments are secondary to a better understanding of, and advancements in mechanical ventilation and earlier antibiotic administration and selection. The primary cause of death in patients with ARDS is sepsis or multi-organ failure. While mortality rates are now around 9–20%, it is much higher in older patients.
Case presentation
A 32-year-old male, came with the complaints of abdominal pain for 4 days. He had the history of yellowish discoloration of urine for 3 days and vomiting 2-3 episodes/day for 3 days and not passed stools for 2 days.
He also had the history of generalized tiredness and poor oral intake. He was addicted to alcohol for past 3 years, weekly thrice, and on continuous alcohol consumption for last 3 days.
On examination
- Patient was conscious and oriented, febrile, with icterus (+),
- CVS – S1S2 (+)
- RS – BAE (+)
- P/A – Soft, epigastric tenderness (+), distended, CNS: NFND
| Vitals | Results |
|---|---|
| PR | 118/min |
| BP | 80/60 mmHg |
| SpO2 | 94% on Room air |
| GRBS | 123mg/dl |
Investigations
Echo – Good LV systolic function (EF-60%)
Pus culture – Citrobacter species
Blood and Urine Culture – No growth
CVC tip culture – Klebsiella pneumoniae
USG Abdomen and Pelvis
- Grade I fatty liver.
- Mild splenomegaly.
- Multifocal hyper echoic collection in the right iliac fossa, Left parabolic gutter and perihepatic region.
CT abdomen and pelvis
- Acute Pancreatitis.
- Large thin-walled pseudo cysts communicating with the proximal body segment of pancreatic duct.
- Moderate ascites.
- Left mild pleural effusion.
- Pancreas appears bulky with <30% necrosis noted near neck of pancreas.


| Investigation Parameters | Patient Value |
|---|---|
| Hb | 13.2 g/dl |
| Platelet | 162200lakhs/cumm |
| TC | 10450cells/cumm |
| Amylase | 376U/L |
| Lipase | 994 U/L |
| Creatinine | 1.02 mg/dl |
| Urea | 30.0 mg/dl |
| Potassium | 3.9 mEq/L |
| Sodium | 136 mmol/LL |
| Bilirubin total | 4.2 mg/dL |
| Procalcitonin | 2.55ng/ml |
| Blood Group | B positive |
| SGOT | 142 U/L |
| SGPT | 118 U/L |
| ALP | 62 U/L |
We received the patient with severe pain abdomen, at our ER. On arrival patient was dehydrated and hypotensive; so he was hydrated with IV fluids and admitted in ICU for further management. After stabilising him we sent his blood sample for investigation. It was found that his LFT was abnormal, along with elevated Sr.amylase and lipase levels. USG and CT abdomen and pelvis revealed features of Acute pancreatitis. Hence, we came to a provisional diagnosis of Acute Pancreatitis as patient has history of alcoholism. Patient was started on IV fentanyl infusion, Inj. Thiamine, vitamin K and other supportive measures. We strictly monitored his vitals and I/O.
Patient gradually developed abdomen distention and tachypnea. He was immediately managed with nasal oxygen and Ryes Tube (RT) aspiration. Meanwhile patient also developed delirium, hence benzodiazepines and dextomed infusion were also started. As delirium worsened overtime patient became restless & agitated, hence patient was intubated on his day 2 of hospital stay.
Patient had intermittent fever spikes. Blood, urine, and central line catheter tip were sent for culture & sensitivity. Started on IV antibiotics (Piptaz & Levofloxacin). Regular chest and limb physiotherapy and incentive spirometry were given to avoid improve his respiratory distress. Serial monitoring of ABG, CBC, Sr.electrolytes were done. Electrolyte changes were corrected accordingly. As bibasal air entry was reduced, chest X-ray and USG chest were done which showed features of bilateral pleural effusion and was treated for the same with nebulization. While blood, urine C&S was Sterile , CVC tip culture showed Klebsiella pneumoniae.
Later he was extubated, we continued with O2 support, and RT feeds. Next day patient had increased pain abdomen with intermittent fever spikes. CECT abdomen suggested necrotic collection at head of pancreas with mild free fluid and bilateral pleural effusion L>R. So, our consultants, after planning and discussion, inserted USG guided pig tail catheter for pelvic collection
But unfortunately Hb dropped to 6 g/dl. We immediately transfused 2 units of ‘ B ‘ positive PRBC. Unexpectedly ARDS worsened so re-intubation was done. Post pulmonologist opinion, Left ICD was inserted and pleural fluid sent for analysis. As it did not improve ,Tracheostomy was done. Periodic review was done by Pulmonologist and ENT surgeon.
Pus culture sensitivity showed Growth of Citrobacter species, started on sensitive antibiotic (Inj. Amikacin).
Thoughout this period, we were constantly informing the patient relatives about the patient ‘s condition and line of treatment .
Medications
| Drug | Dose | Frequency |
|---|---|---|
| Inj. Amikacin | 750mg | OD |
| Tab. Esoz | 40 mg | OD |
| Tab. Ketoflam P | (100/325mg) | BD |
| Tab. Lupase | 25000 | TDS |
| Tab. shelcal | 10 mg | HS |
| Tab. Thyronorm | 500mg | BD |
| Hinex HP powder | 4 scoops | 1-1-1-1 |
| Syp. Zincovit | 10ml | BD |
| Syp. Dexorange | 10ml | BD |
Nursing management
We managed the patient with antibiotics, opioid analgesics and anti-depressants and provided symptomatic treatments according to his condition and symptoms. He was treated with ventilatory support and ICD. Our team provided continuous care and psychological support to the patient and their family. Slowly he improved and discharged after few days.
Patients with ARDS are bed-bound; frequent position changes are highly recommended to prevent bedsores and deep venous thrombosis. One can minimize the sedation in alert patients and make them sit in a chair. Nursing tips for long stay ICU patients are as follows:
- Explain to the patient and the family members, with reassurance, that they will be safe and obtain consent.
- Close the eyes and protect with gel or pad.
- Place the patient’s palms against their thighs, thumbs upwards, elbows straight and shoulders neutral.
- Slide the patient to the edge using a sliding sheet.
- Roll the patient into the lateral position using the underneath sheet.
- Roll the patient into prone.
- Place two pillows under each shin to prevent peroneal nerve stretch, positioning them to avoid knee and toe pressure from mattress.
Nutritional Support
Most patients with ARDS have difficulty eating, and muscle wasting is very common. These patients are either given enteral or parenteral feeding, depending on the condition of the gastrointestinal tract. We educated the patient to take a low-carbohydrate, high-fat diet as it has anti-inflammatory and vasodilating effects. Explained to the patient and the family members about prevention of aspiration by keeping the head of the bed elevated before feeding.
Nurse as a good counselor
Patient’s condition was explained to her family members. Our nursing team gave emotional and psychological support to the patient and family members and provided the best communication and coordination with other team members. So, the patient and family members were sustained the patient health improved and attained positive outcomes.
Psychological support
Recreation therapies were explained like music- hearing; communication with family members, and reading books. After that patient psychologically improved
Outcome of the patient
General condition was good, vitals were stable, hence Discharged with pigtail and follow- up medical advice. Patient family was educated about the pigtail and its care.

