An adult with an atrial septal defect presenting with a brain abscess
G. Rengaraj
Physician Assistant – Neurology, Kauvery Hospital, Cantonment Trichy
Case Presentation
A 31-year-old woman with history of congenital heart disease diagnosed at three years of age, and later diagnosed to have hypothyroidism, presented with a headache and fever followed by difficulty in moving right upper and lower limbs. She was disoriented and in intermittent confusion. GCS was E4V4 M6, with right supranuclear facial paresis associated with right hemiparesis with grade 3/5 power, both proximal and distal, and minimal dysphasia.
There was no history of vomiting, ear discharge, dental caries or otitis media.
The patient initially consulted an obstetrician-gynecologist (OBG) for fertility concerns. During evaluation, an SpO2 level of 88% was noted, with no shortness of breath, and the patient was referred to a cardiologist, where the congenital heart defects were diagnosed.
On examination, she was febrile, high grade, without clubbing of the fingers of both hands. There was no cyanosis. Respiratory examination revealed desaturation with Spo2 87% without Oxygen support. Bilateral air entry was present,
Investigations revealed polycythemia with a packed cell volume of 50%.
MRI brain plain and contrast done showed:
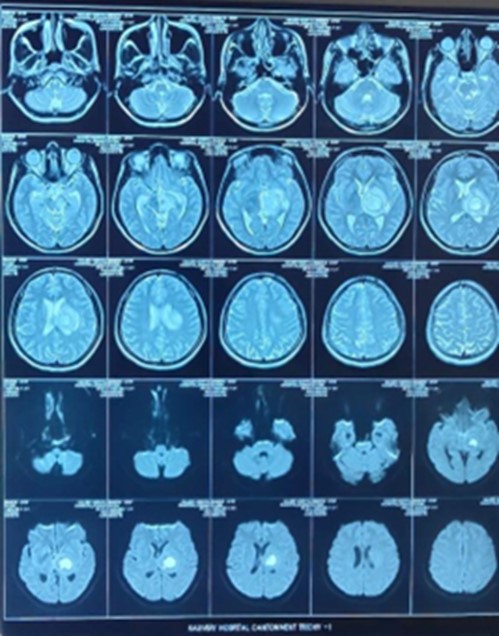
Thick-walled cystic lesions measuring 2.5 × 2.6 cm present in the thalamus region with peripheral contrast enhancement, Central necrotic areas were present. Lesions showed significant diffusion restriction, surrounding white matter edema was present, edema also present involving the brain stem, compression of third ventricle outflow, and asymmetric dilatation of lateral ventricle.
USG abdomen was done which showed no significant abnormality.
Blood cultures were sent and empirical antibiotic therapy was started with ceftriaxone, and vancomycin. However, after starting the treatment, the patient developed an allergic reaction to vancomycin. Consequently, the vancomycin injection was discontinued.
Precordial echocardiogram showed (24mm) ostium primum ASD & (12mm) inlet VSD bidirectional shunt in situ, AV canal defeat, RA/RV dilated, no RWMA, fair LV dysfunction, mild TR, severe PAH, no pericardial effusion/clot.
Gynecologist opinion obtained for fertility, General physician opinion was obtained in view of hypothyroidism, for which she was already on thyroxine reoplacement
Left temporo- parietal craniotomy (Keen’s point approach )and excision of the abscess were done. The abscess was thick-walled in the transcortical region extending deeper and posteriorly. At the posterior part, the abscess cavity was left deliberately to protect the motor cortex. Gentamicin sulfate wash given followed by intravenous administration.
The culture of the aspirated pus was done, keeping in view Streptococcus. AFB, fungal, Gram stains were negative. As per the sensitivity ceftriaxone was continued for two weeks along with Gentamicin. Postoperatively, oxygen support was tapered and weaned off.
A repeat CT scan of the head revealed acute intra parenchymal haematoma in the left ganglio capsular region and parietal lobe, and acute SDH in left parietal convexity, Postoperatively mass effect with midline shift to right side and mid obstructive hydrocephalus were noted Patient was treated with anticonvulsants and other supportive measure. Aggressive physiotherapy was given. Swallow assessment was done after which oral feed was initiated.
Dysphasia, right UMN facial palsy and right hemiparesis improved, and hence discharged

Discussion
Brain abscesses have become a relatively rare entity and are mostly encountered in children between the age of four to ten years. It is frequently encountered in children with uncorrected or partially corrected cyanotic congenital heart diseases. The right-to-left shunting present in cyanotic heart diseases allows bacteria colonizing the airway to pass through the cerebral circulation . These patients develop polycythaemia which further results in tissue hypoxia and ischaemia creating a suitable environment for the growth of bacteria. It is still a serious and potentially fatal entity leading to mortality and morbidity if not managed properly. Multiple and recurrent abscesses have a poorer prognosis. However, the emergence of newer neurosurgical techniques like stereotactic biopsy and aspiration and the availability of newer generations of antibiotics and modern neuroimaging techniques have contributed to better outcomes for brain abscesses.
The success of treatment lies in timely management with targeted antimicrobial therapy and early diagnosis of abscess and surgical drainage . Factors associated with poor prognosis with high mortality rates include delayed administration of antibiotics at the time of admission, multiple and recurrent abscesses, younger age, meningitis, lesions large in size or near the ventricles, and if surgical aspiration is not implemented. In the case of a surgically treated abscess, antibiotics for four to six weeks are recommended and in the case of large multiple abscesses or an abscess treated solely medically, six to eight weeks of antimicrobial therapy is recommended. Three to 12 months of antibiotic treatment is required for immunocompromised. A broad-spectrum antibiotic that can readily cross the blood-brain barrier or blood-CSF barrier should be used. Third-generation cephalosporins and metronidazole are commonly used. Metronidazole readily penetrates brain abscesses and has good bactericidal activity against anaerobes. Small abscesses less than 2.5 cm or multiple abscesses may be treated medically with follow-up scans to ensure a decrease in abscess size. Surgical excision of abscess is not routinely performed and is rarely needed as this is associated with greater morbidity compared to aspiration and is associated with the risk of rupture of abscess into the ventricular system. Aspiration of brain abscess has become the preferred method of drainage providing rapid relief from symptoms of raised intracranial pressure. It is considered easy to perform but has its own disadvantages being the requirement of repeated procedures.
Comparing the efficacy of aspiration versus the excision of the abscess, more residual/recurrence cases occur in the aspiration group who need a second aspiration. No residual/recurrence was observed in the excision group. Duration of hospital stay was comparatively less in the excision group than in the aspiration group.
In our patient, surgical excision of the abscess was successfully performed with the patient showing good results in the form of gain of power in the limbs and no further seizure episodes eventually over a period of four weeks. The posterior part of the cavity was left to protect the motor cortex.
Excision of abscesses carries a risk of rupture of the abscess into the ventricular cavity.Rupture of the abscess was a strong risk factor for poor outcomes . In our patient, the abscess was located far from the ventricles and measured 3.5 cm in diameter. The abscess was successfully excised without any long-term neurological sequelae in the patient.
Reported factors for poorer outcomes in a child with a brain abscess are age younger than five years, and Glasgow Coma Scale (GCS) score <8 at the time of admission.
The reason for the good outcome in our patient may be attributed to the timely and prompt initiation of antibiotics, good GCS at the time of admission, and the non-development of meningitis
Conclusions
In conclusion, a 31-year-old woman, with complex congenital heart disease, developed a brain abscess. She was managed successfully, with good neurological outcomes, due to the timely initiation of antibiotics and excision.

