ASD Surgical Closure
S. Estharrani1, M. Cesilipriya2, Sathya3
1Nursing Superintendent, Kauvery Heartcity, Trichy, India
2Critical Ward Incharge, Kauvery Heartcity, Trichy, India
3Critical Ward Staff Nurse, Kauvery Heartcity, Trichy, India
Abstract
A young 7-year-old child with Atrial Septal Defect, a congenital heart disease (CHD), came to our cardiac department; she was identified at our regular out-reach cardiac camp. She had an elevated heart rate during our evaluation and had no specific cardiac symptoms. After the diagnosis of a CHD, the child was treated with ASD closure using a Minimal Invasive cardiac surgery (MICS) employing an autologous pericardial patch. Quick recognition of the disease and immediate and effective treatment saved the child’s life.
Abbreviations: Atrial septal defect (ASD), Minimal Invasive cardiac surgery (MICS)
Background
In foetal circulation, blood from the right side of the heart does not flow to the lung as the lungs are not functional, they are not aerated. So, a ‘Patent Foramen Ovale” exists between the right and left atria. This closes soon after birth, as the child cries and lungs begin to function
Atrial septal defect (ASD) is a hole in the atrial septum, which is the wall that separates the two upper chambers (atria) of the heart. ASD is a congenital heart defect that occurs when the septum does not form properly. It is also called “hole in the heart”. ASD allows for an abnormal shunt, which means abnormal blood flow that shouldn’t be happening. Normally, oxygen-rich blood flows from the upper chamber, left atrium, down into the lower chamber, the left ventricle and then flows out through the Aorta to deliver oxygen to the body. ASD causes part of the blood to flow in another direction, from the left atrium to the right atrium. The right atrium contains deoxygenated blood that must circulate through the lungs. The right atrium now has extra blood that will eventually go to the lungs. This leakage in the wrong direction can be small (for eg: Patent Foramen Ovale) and may cause no problems for a long time, in which case the ASD can be left alone without treatment. Other times, it can cause problems with the heart or lungs. The larger the ASD, the more likely it is to cause symptoms and require treatment.
Types of ASD:
There are four main types of atrial septal defects. They are defined by their location in the atrial septum.
- Secundum ASDsare in the middle of the atrial septum. This is the most common type of ASD (80% of all ASDs).
- Primary ASDsare at the base of the atrial septum. Babies with primary ASD may also have other heart defects. These include endocardial cushion defects, atrioventricular septal defects, tricuspid valve defects, and mitral valve defects. Primary ASDs are usually associated with Down syndrome.
- Sinus-venosus ASDsare located in the upper or lower back of atrial septum. This type is associated with damage to the right pulmonary vein or the large veins of the heart called the superior or inferior vena cava.
- Uncovered coronary sinusis the rarest type of ASD (less than 1% of all ASDs). It involves a missing or incomplete wall between the coronary sinus (group of veins connected to the heart) and the left atrium.It is more often associated with other complex congenital heart disease.
Case Presentation
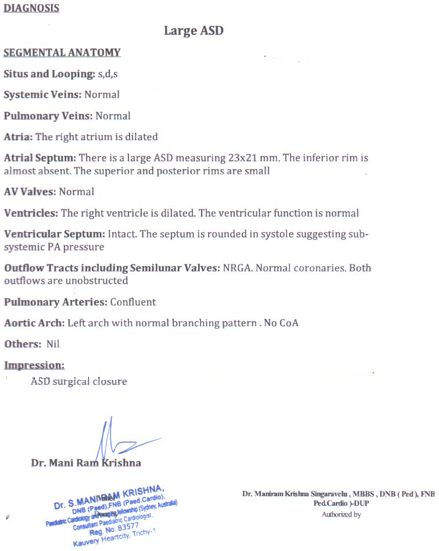
A 7-years-old girl was diagnosed three months back with Acyanotic congenital heart disease, large ostium secundum ASD, and got admitted on 13.3.23 in the cardiac unit for further treatment.
On admission, the child was conscious and oriented. The treatment plan was ASD closure.
The child underwent successful surgical ASD closure using (MICS) autologous pericardial patch on 15.03.2023 with good results.
On Examination
HR – 117b/m , SAO2 – 99% RA, RR – 26bm, Temp – 98.4°F
CVS – S1 S2, RS – BAE (+),BP – 110/, D/ A – Soft, CNS – NFND
Provisional Diagnosis
Acyanotic CHD, Normal LV function
Investigation
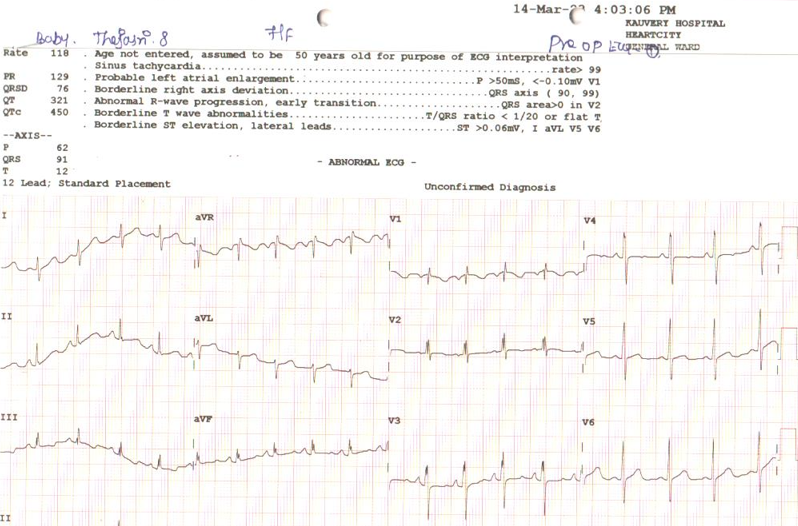
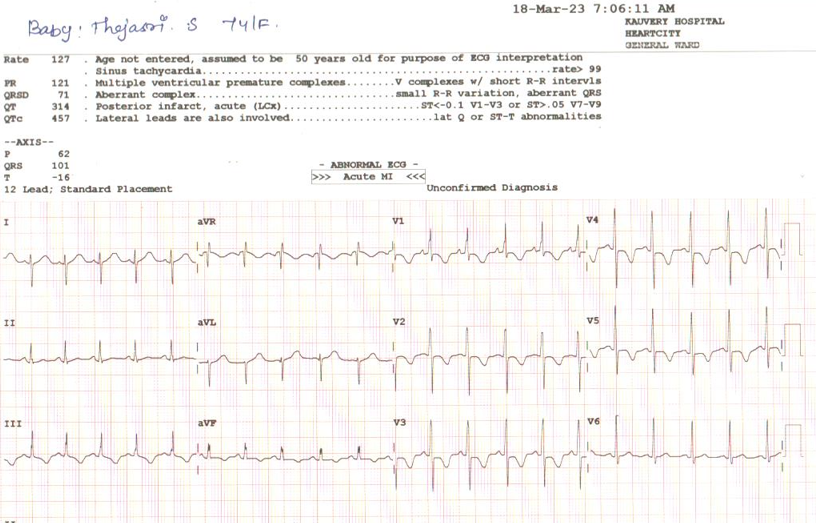
ECG
ECG before surgery:
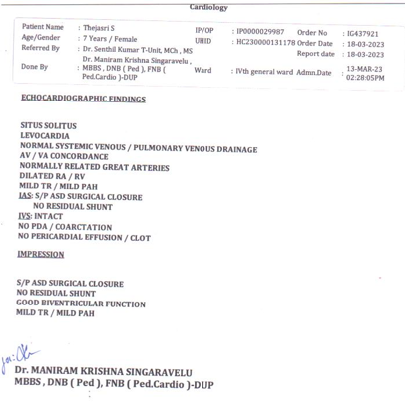
ECHO:
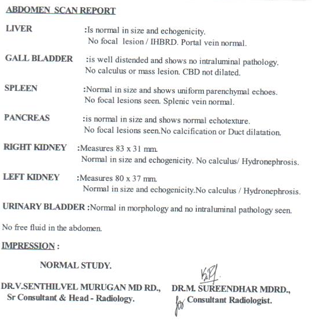
USG Abdomen Report:
Treatment
On the
“0” POD, we administered
- Inj. Supacef – 750 mg
- Inj. Pantocid – 20 mg
- Inj. Kabimol – 500 mg
On the “1” POD, we administered
- Inj. Supacef – 750 mg
- Inj. Pantocid – 20 mg
Discharge Medication Advised:
- Tab.Paracetamol – 250mg
- Tab.Ceftum – 250mg
- Tab.Ivasrad – 5mg
Surgery or other procedure techniques:
Many cardiologists recommend surgery to repair a moderate or large atrial septal defect diagnosed in childhood or adulthood to prevent future complications. In adults and children, surgery to repair atrial septal defects involves closing a hole in the heart. This can be done in two ways:
-
- Catheter-based repair:A thin, flexible tube (catheter) is inserted into a blood vessel, usually in the groin, and guided to the heart using imaging technology. A piece of mesh or plug is passed through the catheter and used to close the hole. Heart tissue grows around the seal and closes the hole permanently. Catheter-based repair is only used to treatsecundum-typelesions of the atrial septum. However, some large atrial septal defects may require open heart surgery.
- Open heart surgery:This type of atrial septal defect repair surgery involves making an incision in the chest to access the heart directly. Surgeons use casts to close the hole. This open heart repair surgery is the only way to repair defects in the atrial primum, sinuses and coronary sinuses. Sometimes, atrial septal defects can be repaired throughsmall incisions (minimally invasive surgery)
Nursing Diagnosis
- 1 Risk for decreased cardiac output related to the defect structure.
- 2. Activity intolerance related to disruption of oxygen transport system
Nursing Management:
- The patient was transferred from the OT to the CTICU for continuous cardiac monitoring under anesthesia.
- Nurses maintained vital signs every 15 minutes, blood pressure was stabilized with inotropes and IV fluids.
- Nurses trained in intravenous infusion and blood sampling techniques (phlebotomy) collected samples for blood count, CBC, ABG, RFT, electrolytes, etc. using sterile technique to prevent thrombophlebitis.
- The doctors explained the patient’s condition to the nurses, the nurses obtained consent for the clinical procedure after proper counseling.
- Responded immediately to the cry or other expressions of distress.
- Implemented play activity measures to reduce anxiety of the child.
- We avoided extreme temperature environments due to hyperthermia or hypothermia increases oxygen demand.
- Nurses used AIDET recognition, introduction, duration, explanation, and praise techniques when interacting with patients and caregivers to reassure them and improve satisfaction.
- The patient stabilized and was transferred to the ward on March 18, 2023 as directed by the physician.
Lifestyle and home care
The child had an atrial septal defect, surgically closed. we recommended certain lifestyle changes to keep the heart healthy and prevent complications.
Exercise and heavy activities:
Exercise is generally safe for patients with ASD. But after ASD repair we a advised to avoid certain activities for few more days.
Outcome
The child was discharged with stable hemodynamical status. W
e advised them to spend their remaining days full of happiness in a healthy way.

