Bilateral internal thoracic artery grafting for CABG
P. Pushpa1, V. Yuvasri2
1OT Incharge, Kauvery Heartcity, Trichy, India
2OT Senior Staff Nurse, Kauvery Heartcity, Trichy, India
Abstract
Coronary artery bypass graft surgery is the mainstay cardiac operation for the treatment of severe atherosclerotic coronary disease. The surgery is founded on harvesting vascular conduits from select anatomic sites in the arterial and venous circulation to serve as bypass grafts. Coronary artery bypass grafting (CABG) is a major surgical operation where atheromatous blockages in a patient’s coronary arteries are bypassed with harvested venous or arterial conduits. The bypass restores blood flow to the ischemic myocardium which, in turn, restores function, viability, and relieves angina symptoms. Almost 400,000 CABG surgeries are performed each year making it the most commonly performed major surgical procedure, but surgical trends have decreased as the use of alternative options such as medical treatment and percutaneous coronary intervention (PCI) have increased. In general, on-pump and off-pump are the 2 types of CABG surgical procedures with the difference being the use of a cardiopulmonary bypass circuit and an arrested heart to operate during an on-pump CABG. The conduits used as bypass grafts are routinely the left internal mammary artery (LIMA) and the saphenous vein grafts (SVG) out of the lower extremities. Other conduits that may be grafted include the right internal mammary artery (RIMA), the radial artery, and the gastroepiploic artery. The type and location of the grafts depend on the patient’s anatomy and the location of the arteries that occluded. Typically, the LIMA grafted to the left anterior descending (LAD) artery, and the other conduits used for the other occluded arteries.
Background
Coronary artery bypass grafting (CABG) remains the Gold standard for excessive coronary artery disease involving three vessels or the left main stem. CABG is more durable than percutaneous coronary intervention, especially when using arterial grafts only. There is abundant literature regarding risks of elderly patients undergoing cardiac surgery. However, reports about younger patients undergoing CABG are sparse. D’Errigo et al. recently reported the multicenter data concerning patients below 50 years of age receiving CABG with a mortality rate of 0.9% overall. However, no details about the used grafts were given in that study. A low postoperative mortality rate has also been reported by Khawaja et al. in patients aged <50 years treated by percutaneous coronary intervention (0.86%). However, percutaneous coronary interventions were performed in 41% of cases in patients with single vessel coronary artery disease, which is significantly different from surgical series.
Patients who would benefit most from prolonged patency of total artery revascularization are the young patients. In this study we therefore sought to further evaluate patients under the age of 50 years receiving coronary artery bypass grafting.
Coronary artery bypass grafting (CABG) has become an integral component of the coronary artery disease (CAD) treatment algorithm. Various conduits for CABG have subsequently been the subject of extensive investigation. Despite experimentation with arterial grafts during the infancy of CABG, the prevailing strategy in coronary surgery continues to be mixed venous and arterial grafting, most commonly a single arterial graft via the gold-standard left internal mammary (LIMA) to left anterior descending (LAD) anastomosis supplemented by saphenous vein grafts (SVG). With anatomical and physiologic characteristics that promote excellent hemodynamics, the LIMA has demonstrated exceptional long-term patency and outcomes, cementing its role in CABG.
Outcome of bilateral mammary artery grafting
As a result of the pioneering work by Drs. Arthur Vineburg, Robert H. Goetz, Vladimir P. Demikhov, Gordon Murray, and Vasilii I. Kolesov in the 1950–60s, coronary artery bypass grafting (CABG) has become an integral component of the coronary artery disease (CAD) treatment algorithm. Various conduits for CABG have subsequently been the subject of extensive investigation. Despite experimentation with arterial grafts during the infancy of CABG, the prevailing strategy in coronary surgery continues to be mixed venous and arterial grafting, most commonly a single arterial graft via the gold-standard left internal mammary (LIMA) to left anterior descending (LAD) anastomosis supplemented by saphenous vein grafts (SVG). With anatomical and physiologic characteristics that promote excellent hemodynamics, the LIMA has demonstrated exceptional long-term patency and outcomes, cementing its role in CABG.
In light of contemporary evidence, multi- and total-arterial grafting is now gaining momentum. In a meta-analysis of 37 randomized controlled trials or propensity-matched retrospective studies, Saraiva et al. reported reduced rates of early mortality, late mortality, and major adverse cardiovascular and cerebrovascular events (MACCE) with increased rates of SWI when comparing multi- to single-arterial grafting. As arterial conduit options, the radial artery and right internal mammary artery (RIMA) have both been investigated. Given its physiologic similarities to the LIMA, the RIMA has been the subject of particular interest. However, contrary to the extensive literature on the LIMA demonstrating a concrete benefit, there has been inconsistent randomized controlled and high-powered data on RIMA patency and late mortality.
While discrepancies between studies have clouded the evidence for graft selection for CABG, the meta-analysis by Stefil and colleagues has demonstrated a long-term mortality benefit with BIMA grafting in patients with diabetes at the expense of an increase in perioperative SWI. While the mortality outcomes are promising, these differences must be considered in the context of the previous literature when applied to clinical practice. The addition of a RIMA graft during CABG requires careful consideration of patient anatomy and comorbidities. An individualized approach to conduit selection is critical. Younger patients and those with diabetes may benefit from an additional RIMA graft and the improved durability it may potentially provide. The patient’s coronary anatomy is of the utmost importance. Target location and stenosis, as well as harvesting technique and proximal location influence graft patency and its potential application. Finally, intraoperative and perioperative strategies should be utilized to mitigate SWI risk to minimize postoperative morbidity following BIMA grafting in suitable patients.
Significance
The LIMA, both in clinical practice and clinical trials, is near-universally considered the first-line graft for the LAD anastomosis. Consequently, the RIMA is most commonly grafted to either the right coronary artery (RCA) or the left circumflex system.
Case presentation
A 39 years old man had complaints of chest burning sensation for 1 week.
He had a previous admission to another hospital with the same complaints and had further management.
There was no significant past history like TB, Asthma, HTN, DM.
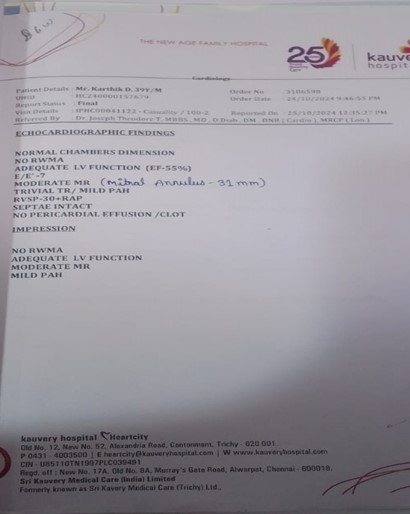
He was admitted in Kauvery Hospital. Through investigations such as ECG and ECHO that revealed good LV function, he was diagnosed to have CAD- ACS-NSTEMI.
CAG showed DVD. From above findings, patient was planned for CABG.
On examination
ECG
Pre OP

Post OP

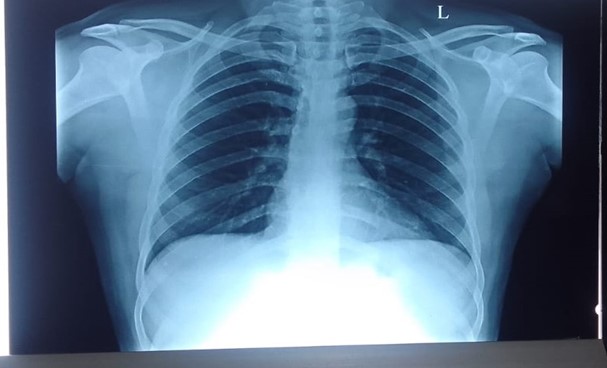
X-Ray
Pre OP X-Ray
Post OP X-ray

ECHO findings
CAG report
- LMCA: Short Normal.
- LAD: Type3, calcified and mild ecstatic vessel. Proximal LAD has 30% stenosis. Mid LAD has 100% occlusion (? Acute on CTO). Distal LAD faintly filled by homo and hetero coronary collaterals.
- Diagonals: D1: Small sized vessel. Ostia proximal 80 to 90% stenosis.
- Other diagonals: Faintly visualized
- LCX: Non – Dominant. Proximal LCX has mild plaquing. Mid LCX has 90 to 95 % stenosis which involving ostium of OM2 (MEDINA 1-1-1). Distal LCX small sized vessel. Mild plaquing.
- OM1 – Small sized vessel. Mild plaquing.
- RCA – Dominant, proximal RCA has 50-60%stenosis.
Impression
- CAD-DVD
- Recommendations & Plan – CABG
Pre-Operative Medications
- Ecosprin 75mg OD
- Tonact 40mg OD
- Pantocid 40mg OD
- Thyroxin 12.5mg OD
Pre OP Investigation
| Hb | 11.4 gm/dL |
| Pcv | 33.5 % |
| Plt | 358000 Cells/Cumm |
| Tc | 12120 Cells/Cumm |
| Urea | 21.40 mg/dL |
| Creat | 0.77 mg/dL |
| Sodium | 138 mmol/L |
| Potassium | 4.0 mmol/L |
Intra Operative findings
- Aorta healthy
- PA soft
- LV contractility fair
- LIMA- 2mm, good caliber
- RIMA-2 mm, good caliber
Procedure
- LAD artery was 1.5 mm, deep intra myocardial, fair runoff, cut across plaque
- OM artery was 1.5mm, fair runoff.
- Median sternotomy, pericardiotomy, systemic heparinization
- RIMA – Free RIMA harvested.
- LIMA – RIMA – at the level of PA dissection using 8-0 prolene continuous sutures.
- Distal anastomosis done with 8-0 prolene continuous sutures.
- Hemostasis achieved.
- Routine chest closure done with 1 Right pleural, 1 Left pleural drains,1 RV pacing wire in situ.
Shifted to CT-ICU with stable hemodynamics for elective ventilation.

Benefits of LIMA RIMA Y bypass graft surgery
- The pain sensation is comparatively less during the healing or recovery process.
- Shorter recovery time and fewer follow-up procedures.
- Lower risk of infection and improved blood flow to the heart.
- The LIMA and RIMA graftsshow the best long-term results
- They are arteries and thus Lima and Rima are most accustomed to forceful blood flow than saphenous vein.
- Veins carry blood from the body back to the heart, and aren’t under much pressure.
- This gives you a long-term advantage and higher durability.
- Mammary Arteries are attached to main artery, this mean that only its other end must be disconnected and grafted onto the diseased coronary artery. This gives advantage of natural inflow.
Post-Operative
‘O’ POD
- Patient received from HCOT with Ambu Ventilation then connected Mechanical ventilator.
- Patient vitals were stable.
- He was managed with necessary supports Inj.Adrenaline – 0.1 ml
- Total ICD drain – 290 ml.
- Extubation was done and patient was in stable condition, after 2 h patient’s PCO2 level increased and she was again intubated and supports were added Inj. Noradrenaline – 1 ml.
- Patient’s condition was stable.
- Antibiotic Inj. Supracef 1.5 gm Administered.
- Every 4 h patient was given back care and ET suctioning.
- Continuous close monitoring of the patient and the ICD drain was done.
- ABG was checked.
- Antibiotic Inj. Supracef 1.5 g administered.
‘I’ POD
- Patient vitals were stable.
- Extubated done.
- Supports Inj.Adrenaline was weaned and stopped.
- Early morning patient was given mouth care and combing done.
- Every 4 h once back care and ET suctioning was done.
- Total ICD drain –
- Patient conscious and oriented.
‘II’ POD
- Patient vitals were stable.
- Patient conscious and oriented.
- Early morning mouth care and nebulization were given.
- Every 2 h back care was given and position was changed.
- Chest physio and Spiro exercise were given.
‘III’ POD
- Patient vitals were stable.
- Every 2 h back care was given and position was changed.
- Early morning mouth care and nebulization were given.
- ICD, Arterial Line and CBD were removed.
- Chest physio and Spiro exercise given.
‘IV’ POD
- Patient vitals were stable.
- Every 2 h back care was given and position was changed.
- Early morning mouth care and nebulization were given.
- Chest physio and Spiro exercise given.
- Patient was mobilized.
- Patient had self diet started.
- CVC line was removed.
- Patient was shifted to ward.
Investigations:
| S. No | Name of the Investigation | O-POD | I-POD | II-POD | III-POD |
|---|---|---|---|---|---|
| 1 | HB | 14.2 gm/dL | 11.4 gm/dL | 10.6 gm/dL | 11.3 gm/dL |
| 2 | PCV | 42.8 | - | - | - |
| 3 | Urea | 23.54 | - | - | - |
| 4 | Creatinine | 0.86 | - | - | - |
| 5 | Sodium | 139 | - | - | - |
| 6 | Potassium | 4.1 | - | - | - |
Nursing management
- Continuously monitor Arterial BP during Acute phase to evaluate the patient’s response to therapy.
- Monitor hourly urine output because a drop in output may indicate renal artery dissection or a decrease in arterial blood flow.
- Continuously monitor ECG for Dysrhythmia formation, ST segment or T-wave changes, suggestions coronary sequelae or a decreases in arterial blood flow.
Nursing Care:
- ET and oral suction care was given.
- 4th hourly ABG was done.
- Hub care was given.
- 4th hourly catheter care was given.
- Provide Mild physio and Spiro given.
- Every morning chest dressing was change.
- 4th hourly back care was given.
- Early morning CVC dressing was given with using Aseptic technique.
Diet for CABG:
- Follow a low salt diet and avoid adding salt to your food.
- Emphasize fruits and vegetables.
- Eat healthy fats including low fat dairy products, healthy oils such as olive and canola oil, nuts and avocados; and flax seed.
- Include whole grains which provide fiber
Exercise
- Use the Incentive spirometer four to five times a day.
- Each session do to slow deep breaths.
- Take your time between breaths.
- Placing your hands (or cough pillow) over your chest incision, perform two or three strong coughs.
- BMC also offers breathing exercise classes.
Home Advice
- Avoid lifting weight for 3 month to continue chest physiotherapy followed the review to take proper diet.
Nursing Management
Nursing Diagnosis
- Acute pain related to surgical tissue Trauma
- Decreased Cardiac output related to
- Changes in intravascular volume.
- Increased Systemic vascular resistance.
- Third space fluid shift.
- Deficient knowledge regarding newly identified need for Aortic surgery.
- Ineffective breathing pattern related to
- Effects of general Anesthesia.
- Endotracheal Intubation.
- Presence of a Chest Incision.
Conclusion
Improved Blood Flow
The surgery enhances blood flow to the heart muscle by diverting it around blocked or narrowed arteries. This restoration of proper blood circulation helps prevent myocardial infarction (heart attack) and contributes to the patient’s overall cardiovascular health. A coronary artery bypass graft (CABG) is a surgical procedure used to treat coronary heart disease. It diverts blood around narrowed or clogged parts of the major arteries to improve blood flow and oxygen supply to the heart.
Reference
- Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381(9867):629–38.
- Kappetein AP, Feldman TE, Mack MJ, Morice MC, Holmes DR, Ståhle E, et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-Year follow-up of the SYNTAX trial. Eur Heart J. 2011;32:2125–34.
- D’Errigo P, Seccareccia F, Barone AP, Fusco D, Rosato S, Maraschini A, et al. Effectiveness of invasive reperfusion therapy and standard medical treatment in AMI. Acta Cardiol. 2010;65:645–52.
- Locker C, Schaff HV, Dearani JA, Joyce LD, Park SJ, Burkhart HM, et al. Multiple arterial grafts improve late survival of patients undergoing coronary artery bypass graft surgery: analysis of 8622 patients with multivessel disease. Circulation. 2012;126:1023–30.
- Buth KJ, Gainer RA, Legare JF, Hirsch GM. The changing face of cardiac surgery: practice patterns and outcomes 2001–2010. Can J Cardiol. 2014;30(2):224–30.
- Kurlansky P. Do octogenarians benefit from coronary artery bypass surgery: a question with a rapidly changing answer? Curr Opin Cardiol. 2012;27(6):611–9. doi: 10.1097/HCO.0b013e328358b072.
- Vasques F, Lucenteforte E, Paone R, Mugelli A, Biancari F. Outcome of patients aged ≥80 years undergoing combined aortic valve replacement and coronary artery bypass grafting: a systematic review and meta-analysis of 40 studies. Am Heart J. 2012;164(3):410–418.e1.
- D’Errigo P, Biancari F, Maraschini A, Rosato S, Badoni G, Seccareccia F. Thirty-day mortality after coronary artery bypass surgery in patients aged <50 years: results of a multicenter study and meta-analysis of the literature. J Card Surg. 2013;28(3):207–11.
- Weintraub WS, Grau-Sepulveda MV, Weiss JM, O’Brien SM, Peterson ED, Kolm P, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467–76. doi: 10.1056/NEJMoa1110717.
- Konstantinov I.E., Robert H. Goetz: The surgeon who performed the first successful clinical coronary artery bypass operation. Ann. Thorac. Surg. 2000;69(6):1966–1972. doi: 10.1016/s0003-4975(00)01264-9.
- Saraiva F.A., Leite-Moreira J.P., Barros A.S., et al. Multiple versus single arterial grafting in coronary artery bypass grafting: a meta-analysis of randomized controlled trials and propensity score studies. Int. J. Cardiol. 2020;320:55–63.

