Blood Transfusion Reactions: An overview
S. Suganya1*, B.Mahalakshmi2
1Infection Control Nurse, Kauvery Hospital, Tennur, India
2Nursing Superintendent, Kauvery Hospital, Tennur, India
Abstract
Blood transfusions are a relatively common medical procedure. While usually safe, complications are possible that need to be recognized and treated. Transfusion reactions are adverse events associated with the transfusion of whole blood or one of its components. They range in severity from minor to life-threatening. When they occur during a transfusion, they are termed acute transfusion reactions; when occurring days or days to weeks later, they are termed delayed transfusion reactions. This paper reviews the evaluation and management of transfusion reactions and highlights ‘Why blood culture is necessary for investigating any transfusion reaction’
Background
Transfusion reactions are defined as adverse events associated with the transfusion of whole blood or one of its components. These may range in severity from minor to life-threatening. Reactions can occur during the transfusion (acute transfusion reactions) or days to weeks later (delayed transfusion reactions) and may be immunologic or non-immunologic. A reaction may be difficult to diagnose as it can present with non-specific, often overlapping symptoms. The most common signs and symptoms include fever, chills, urticaria (hives), and itching. Some symptoms resolve with little or no treatment. However, respiratory distress, high fever, hypotension (low blood pressure), and red urine (hemoglobinuria) can indicate a more serious reaction.
Types of transfusion reactions
- Acute hemolytic
- Delayed hemolytic
- Febrile non-hemolytic
- Anaphylactic
- Simple allergic
- Septic (bacterial contamination)
- Transfusion-related acute lung injury (TRALI) and
- Transfusion-associated circulatory overload (TACO).
Etiology
- Immune-mediated transfusion reactions typically occur due to mismatch or incompatibility of the transfused product and the recipient. They include naturally occurring antibodies in the blood recipient (such as anti-A, anti-B which are typically responsible for acute hemolytic transfusion reactions) as well as antibodies made in response to foreign antigens (alloantibodies).
- These alloantibodies account for many reactions including mild allergic, febrile non-hemolytic, acute hemolytic and anaphylactic.
- Antibodies present in the blood donor can also cause reactions and are thought to be involved in transfusion-associated lung injury
- Non-immunologic reactions are usually caused by the physical effects of blood components or the transmission of disease caused by bacterial and endotoxin contamination of a blood product.
- Inadequate blood donor arm disinfection, the presence of bacteria in the donor’s circulation at the time of collection or due to improper product handling after collection.
Acute Transfusion Reactions
Mildly allergic: Attributed to hypersensitivity to a foreign protein in the donor product.
Anaphylactic: Similar to above in mechanism, but resulting in a more severe reaction. Sometimes this can occur in a patient with IgA deficiency who makes alloantibodies against IgA and then receives blood products containing IgA.
Febrile non-hemolytic: Generally thought to be caused by cytokines released from blood donor leukocytes (white blood cells).
Septic: Caused by bacteria or bacterial byproducts (such as endotoxin) which may contaminate blood.
Acute hemolytic transfusion reactions
- Can result in intravascular or extravascular hemolysis, depending on the specific etiology.
- Immune-mediated reactions are often a result of recipient antibodies present to blood donor antigens.
- Non-immune reactions are possible, and occur when red blood cells are damaged before transfusion (e.g., by heat or incorrect osmotic conditions).
Transfusion-associated circulatory overload (TACO)
Occurs when the volume of the transfused component causes hypervolemia (volume overload).
Transfusion-related acute lung injury
- Acute lung injury is due to antibodies in the donor product (human leukocyte antigen or human neutrophil antigen) reacting with antigens in the recipient.
- The recipient’s immune system responds and causes the release of mediators that lead to pulmonary edema.
- Possibly contributing to this are clinical conditions that predispose the patient including infection, recent surgery or inflammation.
Delayed Transfusion Reactions
Delayed hemolytic transfusion reaction
Typically caused by an anamnestic response to a foreign antigen that the patient was previously exposed to (generally by prior transfusion or pregnancy).
Transfusion-associated graft-versus-host disease
- Results from engraftment of donor lymphocytes (commonly found in cellular blood products) into an immunocompromised recipient’s bone marrow.
- The donor lymphocytes recognize the patient as foreign and react against the recipient’s body.
- The patient’s immune system is unable to clear the foreign lymphocytes. This is rare but often fatal.
History and Physical
- A thorough understanding of the patient’s medical history and state of health is needed before the transfusion is started.
- Vital signs are monitored and typically recorded at 15-minute intervals.
- The bedside nurse should be extra vigilant in monitoring for a reaction.
- Monitor Abnormal responses include hives, itching, fever greater than 1 C above the temperature at the start of transfusion, chills, hypotension and dyspnea.
Evaluation
Diagnosis of acute transfusion reactions begins by recognition of the signs and symptoms by the bedside. Common signs and symptoms and differential diagnosis are listed below.
Urticaria/Itching
Urticaria (hives) or itching can be the presenting sign of a mild allergic reaction, but can also be associated with the onset of a life-threatening anaphylactic reaction. The transfusion should be stopped, and the patient should be carefully monitored for progression of symptoms.
Fever/Chills
Fever and/or chills are most commonly associated with a febrile, non-hemolytic reaction, however; they can also be the first sign of a more serious acute hemolytic reaction, TRALI, or septic transfusion reaction. If the temperature rises 1 C or higher from the temperature at the start of transfusion, the transfusion should be stopped. Acute hemolytic reaction or bacterial contamination should be suspected if there is a greater rise in temperature, or more serious symptoms (e.g., rigors).
Respiratory Distress/Dyspnea
Dyspnea, or shortness of breath, is a concerning sign that can often be seen with more severe reactions including anaphylaxis, TRALI, and TACO. It can also be seen by itself without accompanying symptoms.
Hypotension
Hypotension can be seen with an acute hemolytic reaction, septic transfusion reactions, anaphylaxis, and TRALI. They have also been reported without the presence of any other associated transfusion reaction.
Hypothermia
Hypothermia can be seen with large volume transfusions of refrigerated products. The only intervention needed is warming the patient and/or blood product.
Treatment/Management
When a transfusion reaction is suspected,
- The transfusion should be immediately stopped
- The intravenous line should be kept open using appropriate fluids (usually 0.9% saline).
- A clerical check should be performed by examining the product bag and confirming the patient’s identification.
- The patient’s vital signs should be monitored and recorded at 15-minute intervals.
- A post-transfusion blood sample should be drawn and sent to the lab in addition to sending the bag and tubing if possible.
- The blood bank generally completes additional testing and clerical checks to rule out an incompatible transfusion.
- Treatment of specific transfusion reactions is most often supportive. For example, antihistamines (such as diphenhydramine) can be given for a mild allergic reaction, or an antipyretic can be given for a non-hemolytic febrile transfusion reaction.
Laboratory Investigation
When a transfusion reaction is suspected it has to be reported using the ‘Report of a Suspected Adverse Transfusion Reaction/Event’ form WRH-BT-HF-006.
This outlines sample requirements and patient transfusion details required for the investigation to be carried out in the laboratory including
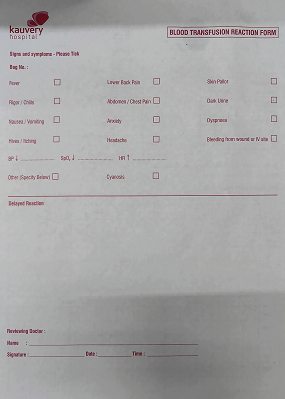
Blood Transfusion Monitoring Record

Blood Transfusion Reaction Form
- Implicated Unit with attached giving set
- Repeat Group and X-match sample
- Blood Cultures on the patient if Temperature rise ≥ 1.5ºC above the baseline temperature together with chills or rigors
- Blood Culture from implicated treatment pack as per instructions below if high likelihood of bacterial contamination
- Full Blood Count
- Renal Profile
- MSU.
Procedure for Blood Culturing of implicated Red Cell Pack/Blood component
Blood cultures from the patient and transfusion sample should be drawn to assess for infection and sepsis.
In delayed transfusion reactions, antibodies should be retested in the patient sample and compared with the patient’s pre-transfusion sample to evaluate for new autoantibodies.
Carry out this procedure at the patient’s bedside using an aseptic technique. Ensure that both the patient and the implicated unit of blood are cultured at the same time and that both sets of bottles are clearly differentiated.
- Withdraw approx. 20mls of blood into a syringe maintaining asepsis.
- Place 8 – 10mls of blood into each blood culture bottle.
- Label blood culture bottles with patient’s labels and write: ‘Blood from blood pack and Donor Unit No.’
- Complete the Microbiology Request Form with the following details
Requisition for Microbiological Examination Form
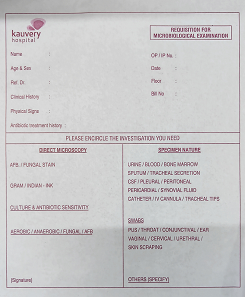
- Patient’s Addressograph label plus name of Consultant Hematologist and address for reporting.
- Fill in Specimen as ‘Blood culture X 2. Peripheral blood + Blood from pack’
- Fill in Clinical details as ‘Transfusion reaction. Donor Unit No: XXXXXX’. Send bottles and accompanying request form immediately to the Microbiology Department in a bio-hazard bag.
- Fill in Tests Required as ‘C/S
- Send bottles and accompanying request form immediately to the Microbiology department in a biohazard bag.
- Dispose of sharps in the correct manner and wash hands.
- Ensure Blood Cultures are taken from the patient as Blood Cultures from a blood pack cannot be processed unless both sets arrive in lab with details on the one form.
Conclusion
Blood transfusion is a life saving measure for many patients, it should be restricted to patients who are in real need for blood replacement. Blood cultures from the patient and transfusion sample should be drawn to assess for infection and sepsis. Blood transfusion is safer today than it previously was due to the measures practiced to improve the quality of blood supply and to reduce the risk of transfusion-transmitted diseases.

