Case report on Gouty Arthritis
Cecily Ruba
Nurse Educator, Kauvery Hospital, Trichy, Cantonment, Tamil Nadu, India
Abstract
This case report discusses the presentation, diagnosis, and management of acute gouty arthritis in a 22-year-old IT professional presenting with severe pain and swelling in the right knee. Gout, a form of inflammatory Arthritis, typically affects older individuals, but its occurrence in younger populations, including individuals with sedentary occupations such as IT employees, underscores the importance of lifestyle factors and dietary habit in its pathogenesis. This report highlights the challenges in diagnosing and managing gout in younger individuals and emphasizes the need for comprehensive patient education and lifestyle modifications alongside pharmacological interventions.
Background
Gout is a type of inflammatory Arthritis characterized by the deposition of monosodium urate (MSU) crystals in joints and surrounding tissues. The pathophysiology of gout involves a complex interplay of genetic predisposition, dietary factors, altered purine metabolism, and immune responses.
Hyperuricemia: The underlying cause of gout is elevated levels of serum uric acid, known as hyperuricemia. Uric acid is a byproduct of purine metabolism, and its elevated levels can result from increased production or decreased excretion. In gout, hyperuricemia leads to the precipitation of MSU crystals, which serve as the nidus for inflammatory responses within the joints.
Formation of Monosodium Urate Crystals: Under conditions of hyperuricemia, urate crystals can form in the synovial fluid of joints, tendons, and surrounding tissues. These crystals are typically needle-shaped and negatively birefringent when viewed under polarized light microscopy. The deposition of MSU crystals triggers an inflammatory cascade, leading to acute gouty arthritis.
Inflammatory Response: The presence of MSU crystals within the joint space initiates an inflammatory response mediated by the innate immune system. This response involves the activation of resident macrophages and the release of pro-inflammatory cytokines, such as interleukin-1β (IL-1β) and tumor necrosis factor-alpha (TNF-α). These cytokines stimulate the recruitment of neutrophils and other immune cells, amplifying the inflammatory process.
Activation of the NLRP3 Inflammasome: MSU crystals are recognized as danger signals by the NOD-like receptor family pyrin domain-containing 3 (NLRP3) inflammasome, a multiprotein complex involved in innate immune responses. Activation of the NLRP3 inflammasome leads to the cleavage of pro-IL-1β into its active form, IL-1β, which contributes to the inflammatory cascade and amplifies the local immune response.
Tissue Damage and Symptomatology: The inflammatory response initiated by MSU crystals results in tissue damage, characterized by synovitis, cartilage erosion, and bone resorption within the affected joint. This process manifests clinically as the classic symptoms of acute gouty arthritis, including severe pain, swelling, redness, and warmth in the affected joint. If left untreated, recurrent gout attacks can lead to chronic joint damage and deformity.
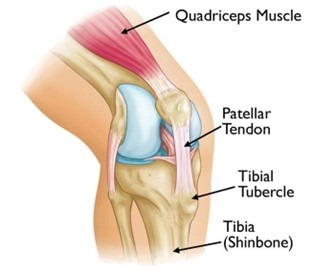
The Knee Joint
Case Presentation
Chief Complaint
A 22 years old male patient working as a IT staff, who presented to the emergency department with severe pain and swelling in his right knee. He reported sudden onset of symptoms that worsened over the past 24 hours, limiting his ability to walk or bear weight on the affected leg. There was no history of any recent trauma or strenuous activity.
Social History
Despite working in a sedentary occupation as an IT professional, the patient maintains a balanced approach to physical activity, incorporating regular exercise routines outside of work hr. Dietary habits are notable for their moderation, with an emphasis on a diverse range of nutritious foods and minimal consumption of high-purine or processed items. No bad habits of alcohol and smoking intake. The patient enjoys strong social support from family and friends, fostering a supportive environment conducive to maintaining optimal health. Overall, the patient’s social history reflects a commitment to wellness and prevention, contributing to a reduced likelihood of gout-related complications.
Allergies
No known medicine or environmental allergies.
Past Medical History
There is no significant past medical history
Past Surgical history
No known surgical history.
Physical Examinations
Vital signs
BP 120/80mm Hg; Pulse 100 per min; RR: 20 per min; Temp: 99°F; Spo2 99%.
Right Knee
His right knee was erythematous, warm to touch, and markedly swollen with limited range of motion due to pain.
Laboratory Investigations
Serum uric acid: 8.5 mg/dL(reference range 3.4-7.0 mg/dL)
CRP – 5.2
WBC – 13,700
ESR – 13
No synovial aspiration done.
Plain radiographs of the knee showed soft tissue swelling without evidence of joint space narrowing or erosions.
Treatment
Based on clinical presentation and laboratory findings, a diagnosis of acute gouty arthritis affecting the right knee was made.
The patient was started on nonsteroidal anti- inflammatory drugs (NSAIDs) for pain relief and Colchicine for anti-inflammatory prophylaxis.
| Drug | Dose | Frequency |
|---|---|---|
| Tab. Goutinil (Colchicine) | 0.5mg 2 stat and 0.5mg | TDS for 2 weeks |
| Inj. Diclofenac sodium | 75mg | IM stat |
| Tab. Zyloric acid | 300mg stat and 100mg | BD for 2 weeks |
| Tab. Artane (Etoricoxib) | OR for pain SOS |
He was advised to adhere to a low-purine diet, increase fluid intake, and avoid alcohol consumption
Clinical Pharmacological aspects of Colchicine
Colchicine is a medication primarily used for the prevention and treatment of gout attacks and familial Mediterranean fever (FMF). Here are some key clinical pharmacology aspects of colchicine:
Mechanism of Action: Colchicine binds to tubulin, a protein involved in the assembly of microtubules. By binding to tubulin, colchicine disrupts microtubule polymerization and spindle formation during cell division, leading to anti-inflammatory effects. Colchicine also inhibits the migration of neutrophils to sites of inflammation.
Pharmacokinetics: Colchicine is readily absorbed from the gastrointestinal tract after oral administration, with peak plasma concentrations reached within 2-4 hours. It is metabolized primarily in the liver, and its metabolites are eliminated via biliary excretion and renal clearance. The half-life of colchicine is relatively short, approximately 9-10 hours, but its effects may last longer due to its tissue binding properties.
Indications: Colchicine is indicated for the treatment and prevention of acute gout flares and for the prophylaxis of gout attacks during initiation of urate-lowering therapy. It is also used for the treatment of FMF, a genetic auto inflammatory disorder characterized by recurrent fever and inflammation of serosal surfaces.
Adverse Effects: Common adverse effects of colchicine include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain. These effects are dose-related and can be mitigated by reducing the dose or taking colchicine with food. Severe toxicity can occur with overdose, leading to multi-organ failure, myelosuppression, and death.
Drug Interactions: Colchicine has a narrow therapeutic index and can interact with several medications, particularly those that inhibit its metabolism or renal excretion. Concomitant use of colchicine with strong CYP3A4 inhibitors (e.g., clarithromycin, erythromycin, ketoconazole) or P-glycoprotein inhibitors (e.g., cyclosporine, verapamil) can increase colchicine levels and risk of toxicity. Patients taking colchicine should be monitored closely for signs of toxicity when initiating or discontinuing interacting medications.
Special Populations: Caution is warranted when using colchicine in patients with renal or hepatic impairment, as dosage adjustments may be necessary to prevent toxicity. Colchicine is contraindicated in patients with severe renal or hepatic impairment. Additionally, it should be used with caution in elderly patients and those with cardiac disease, as colchicine overdose can precipitate myocardial toxicity and arrhythmias.
Pregnancy and Lactation: Colchicine should be used with caution during pregnancy, especially during the first trimester, as there is limited data on its safety. It is excreted in breast milk, and breastfeeding should be avoided while taking colchicine.
Monitoring: Patients taking colchicine should be monitored regularly for signs of toxicity, including gastrointestinal symptoms, myelosuppression, and neuromuscular effects. Renal function should be assessed periodically, and dosage adjustments may be necessary in patients with renal impairment.
Clinical Pharmacological aspects of Allopurinol
Allopurinol is a medication primarily used for the management of gout and certain other conditions associated with elevated uric acid levels. Here are some key clinical pharmacology aspects of Allopurinol:
Mechanism of Action: Allopurinol is a xanthine oxidase inhibitor. It works by inhibiting the enzyme xanthine oxidase, which is involved in the conversion of hypoxanthine and xanthine to uric acid. By blocking this enzyme, allopurinol reduces the production of uric acid, thereby lowering serum uric acid levels.
Pharmacokinetics: Allopurinol is well absorbed after oral administration, with peak plasma concentrations reached within 1-2 hours. It is metabolized in the liver to its active metabolite, oxypurinol (also known as alloxanthine), which is responsible for its pharmacological effects. Oxypurinol has a longer half-life than allopurinol, approximately 15-20 hours, allowing for once-daily dosing in most patients.
Indications: Allopurinol is indicated for the treatment and prevention of gout, a type of arthritis caused by the deposition of urate crystals in the joints. It is also used for the management of hyperuricemia associated with conditions such as kidney stones and certain types of cancer therapy.
Adverse Effects: Common adverse effects of allopurinol include gastrointestinal symptoms such as nausea, vomiting, and diarrhea. Skin rash is another common adverse effect and can range from mild to severe, including Stevens-Johnson syndrome and toxic epidermal necrolysis in rare cases. Hypersensitivity reactions, including fever, eosinophilia, and vasculitis, may also occur. Allopurinol can rarely cause hepatotoxicity and bone marrow suppression.
Drug Interactions: Allopurinol may interact with other medications, particularly those metabolized by the same hepatic enzymes or those that affect renal function. Concurrent use of allopurinol with azathioprine or mercaptopurine, which are metabolized by xanthine oxidase, can increase their toxicity and require dose adjustments. Allopurinol may also potentiate the effects of certain anticoagulants, such as warfarin.
Special Populations: Allopurinol should be used with caution in patients with impaired renal function, as both allopurinol and its metabolites are excreted renally. Dosage adjustments may be necessary in patients with renal impairment to prevent accumulation of the drug and its metabolites. Allopurinol is generally considered safe for use in elderly patients, but lower starting doses may be warranted due to age-related changes in renal function.
Pregnancy and Lactation: The safety of allopurinol use during pregnancy is uncertain, and it should only be used if the potential benefits outweigh the risks to the fetus. Allopurinol is excreted in breast milk, but the amount transferred to the infant is usually low. Breastfeeding while taking Allopurinol is generally considered safe, but caution is advised.
Monitoring: Patients taking Allopurinol should be monitored regularly for signs of hypersensitivity reactions, including skin rash and fever. Liver function tests may be performed periodically to monitor for hepatotoxicity. Renal function should also be assessed regularly, especially in patients with pre-existing renal impairment or those receiving high doses of Allopurinol.
Newer drugs for Gout
- Febuxostat: A xanthine oxidase inhibitor used to lower uric acid levels in gout patients who can’t take allopurinol.
- Pegloticase: An IV enzyme treatment for severe, unresponsive gout that converts uric acid into a more soluble form for excretion.
- Lesinurad: This drug inhibits uric acid reabsorption in the kidneys, often used alongside xanthine oxidase inhibitors to enhance uric acid excretion.
- Arhalofenate: It’s a dual-action drug with urate-lowering and anti-inflammatory effects, studied for gout treatment but still under research for its efficacy and safety.
Follow-Up and Management
To repeat Uric acid after 2 weeks and to review in ortho OPD.
Skilled Nursing Care
Skilled nursing care plays a crucial role in managing acute gouty arthritis episodes and facilitating the recovery process for patients. Here’s an outline of skilled nursing care for a patient experiencing acute gouty arthritis:
Pain Management
- Assess the severity of pain using appropriate pain assessment tools.
- Administer prescribed analgesics promptly to alleviate pain and discomfort.
- Monitor the patient’s response to pain medication and adjust the dosage as needed.
- Utilize non-pharmacological pain management techniques such as positioning, cold therapy (ice packs), or distraction techniques to supplement pharmacological interventions.
- Educate the patient on the importance of adhering to the prescribed pain management regimen and reporting any changes in pain intensity or quality.
- Joint Protection and Positioning:
- Assist the patient in positioning the affected joint in a comfortable and supported position to minimize pain and reduce inflammation.
- Provide pillows or cushions to support the affected joint and promote proper alignment.
- Encourage the patient to avoid putting weight on the affected joint and to limit movement to prevent exacerbating pain and inflammation.
- Educate the patient on the importance of joint protection techniques and proper body mechanics to prevent further damage to the affected joint.
Mobility Assistance
- Assist the patient with activities of daily living (ADLs) such as bathing, dressing, and toileting, taking care to minimize strain on the affected joint.
- Provide mobility aids such as crutches or walkers to assist with ambulation if necessary, ensuring proper fit and instruction on safe use.
- Collaborate with physical therapy to develop a tailored exercise program focused on maintaining joint mobility, strengthening muscles, and improving overall function once the acute phase of gouty arthritis has resolved.
Monitoring and Assessment
- Conduct regular assessments of the affected joint, including monitoring for changes in swelling, redness, warmth, and range of motion.
- Document the patient’s response to treatment, including pain levels, medication administration, and any adverse reactions.
- Monitor vital signs and laboratory values, including serum uric acid levels, to evaluate the effectiveness of pharmacological interventions and guide treatment adjustments.
Patient Education and Support
- Provide comprehensive education to the patient and their family regarding the nature of gouty arthritis, triggers for acute attacks, and strategies for prevention and management.
- Discuss the importance of dietary modifications, hydration, weight management, and lifestyle changes in reducing the frequency and severity of gout flares.
- Offer emotional support and encouragement to the patient, addressing any concerns or anxiety related to their condition and treatment.
Collaboration and Communication
- Maintain open communication with the interdisciplinary healthcare team, including physicians, physical therapists, pharmacists, and other healthcare providers, to ensure coordinated care and optimal outcomes.
- Collaborate with the patient’s primary care provider to develop a comprehensive care plan tailored to the individual’s needs and preferences.
- Facilitate continuity of care by providing thorough documentation, including assessments, interventions, and patient responses, to ensure seamless transitions between care settings.
Conclusion
This case report highlights the occurrence of acute gouty arthritis in a young IT professional and underscores the importance of considering lifestyle factors and dietary habits in the pathogenesis of gout. Comprehensive management of gout should include pharmacological interventions for acute attacks and long-term urate-lowering therapy, along with patient education regarding lifestyle modifications to prevent recurrence. Healthcare providers should be vigilant for gout in younger individuals presenting with suggestive symptoms, particularly those with sedentary occupations and poor dietary habits.

