Coronary Artery Disease and Carotid Stenosis: A dual threat
Vijayalakshmi1, Sangeetha2
1Non Critical Ward Incharge, Kauvery Heartcity, Trichy, India
2Non Critical Ward Senior Staff Nurse, Kauvery Heartcity, Trichy, India
Definition
Carotid artery stenosis happens when the carotid artery becomes blocked or narrow. This is from a build-up of plaque that blocks blood flow to the brain.
Risk Factors
Modifiable risk factors
- Hypertension: High blood pressure accelerates atherosclerosis.
- Hyperlipidemia: High level of LDL cholesterol contributes to atherosclerosis.
- Diabetes Mellitus: Insulin resistance and hyperglycemia promote atherosclerosis.
- Smoking: Smoking damages the endothelium and promotes atherosclerosis.
- Obesity: Excess weight increases the risk of developing carotid stenosis.
- Physical inactivity: A sedentary lifestyle contributes to atherosclerosis.
- Unhealthy diet: Consuming a diet high in saturated fats, cholesterol and sodium increase the risk.
Non-Modifiable risk factors
- Age: Risk increase with age, especially after 65years
- Family history: genetic predisposition to atherosclerosis
- Male Sex: Men are more likely to develop carotid stenosis than women
- Previous Stroke or TIA: History of stroke or TIA increase the risk.
Carotid Endarterectomy
Carotid Endarterectomy is a prophylactic operation designed to reduce the risk of subsequent stroke and stroke related morbidity. As such the effectiveness of prophylaxis is directly related to the perioperative risk of operation.
Anatomy
The Internal Carotid Artery
The Internal Carotid Artery is located with the carotid triangle under and deep to the Stylohyoid muscle and the posterior belly of the Digastric muscle.
The internal carotid arteries are direct branches of the common carotids, superior to the origin of the external carotid artery at the level of the superior border of the thyroid cartilage. The internal carotid has no branches in the neck, its supply is limited to intracranial structures. It is crossed laterally by the hypoglossal nerve.
The External Carotid Artery
The external carotid artery begins at the bifurcation of the common carotid artery at C4. It continues upward to a point at the neck of the mandible (approximately 1.5cm below the zygomatic arch) where it bifurcates to from the maxillary and superficial temporal arteries.
The eight variable branches of the external carotid are:
- Maxillary
- Superficial Temporal
- Lingual
- Facial
- Ascending Pharyngeal
- Occipital
- Posterior Auricular Arteries
Symptoms
- Weakness or tingling: Weakness, tingling or altered sensations on one side of the face or body.
- Vision Changes: Sudden double vision in one or both eyes.
- Speech Problems: Sudden trouble talking or slurred speech.
- Headache: Sudden severe headache.
- Dizziness: Dizziness, vertigo or light-headedness.
- Passing out: loss of consciousness.
- Carotid artery disease can lead to a transient ischemic attack or stroke. A TIA is similar to a stroke but doesn’t cause permanent brain damage.
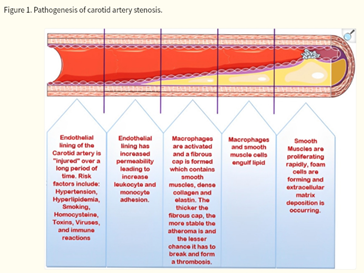
Pathogenesis of Carotid Artery Stenosis
Presenting complaints and History
A 54 years old male had complaints of cough, cold, fever and breathlessness for 3 days. He initially went to outside Hospital, CAG done showed triple vessel disease and PCI to LCX was done and was referred here for further management. Preoperative investigations were done.
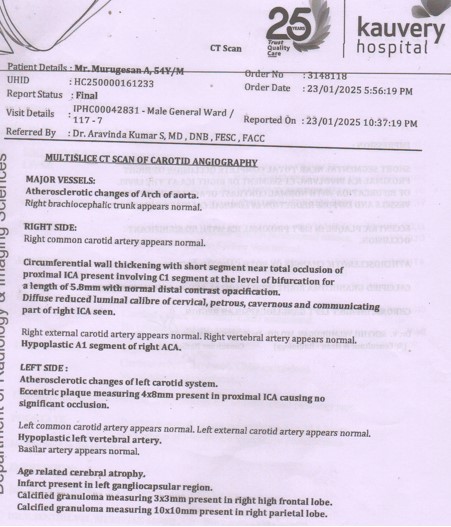
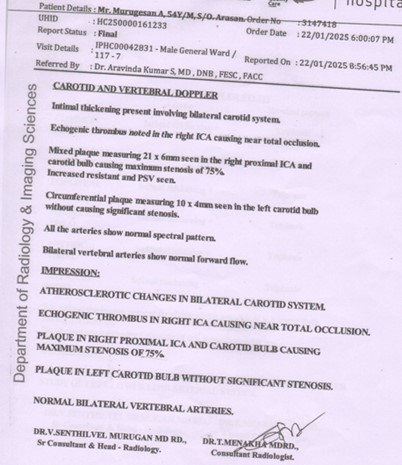
After medical optimization planned for CABG. During preoperative assessment Carotid Doppler showed ight proximal ICA and carotid bulb showing maximum stenosis of 75%. Further CT Angiogram revealed short segmental, near total/ complete occlusion of right proximal ICA. Involving C1 segment of right ICA at the level of bifurcation with normal contrast opacification of distal vessels and diffuse reduction in caliber of right ICA.
Diagnosis
Recent IWMI, S/P CAG – TVD, S/P PCI – LCX- , moderate LV Dysfunction, CAG – TVD – (22/01/25), and Right internal carotid occlusion,
Plan: Right internal carotid endarterectomy.
Course of Stay in Hospital
A 54-year-old male, he was diagnosed Coronary artery disease, Acute IWMI with moderate LV dysfunction. His Coronary Angiogram showed Triple Vessel disease and S/P PTCA to LCX 05/01/2025, & history of CHB, was treated and then referred here for further management.
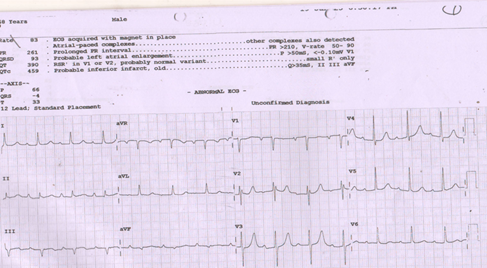
His ECG showed IW/PW MI, Echo showed IW/PW /IW hyperkinesia with moderate LV dysfunction, was advised planned for Re Angiogram.
Coronary Angiogram was done on 22/01/2025 that showed aneurysm in LCx stent segment and was planned for CABG.
His perioperative workups were initiated. Neurologist opinion was obtained for right ICA near total occlusion, right proximal ICA, Carotid bulb plaque causing 75% stenosis in CV Doppler and was advised CT angio of ICA.
Review was obtained from Neurologist and the risk of stroke in the perioperative period was explained to the patient and his attenders. Neuro surgeon opinion was obtained and was planned for Right internal carotid endarterectomy.
His preoperative workups were done and fitness attained for surgery.
The patient underwent successful CABG × 2 Grafts off pump (LIMA – LAD & SVG – LPDA) + Right internal carotid endarterectomy on 30/01/2025.
His postoperative hospital stay was uneventful. During the postoperative period, he was managed with necessary supportive measures. The patient’s condition improved and was prepared for discharge in a stable hemodynamic status.
ECG Report

Carotid Angiography
Doppler Report
CAG Report

Pre OP Nursing Management
- Patient for continuous cardiac monitoring.
- Nurses maintained every hourly vital signs and intake /Output and assessed neurologically.
- Blood sampling done for pre Op investigation under aseptic technique to prevent thrombophlebitis that is CBC< B/G, Serum electrolytes, RFT, Serology USG abdomen and carotid Doppler.
- Doctors explained about risk and benefits of procedure to the attender and informed consent obtained.
- Skin preparation was done and patient was given a povidone bath to minimize the risk of infection.
- NPO instructions were explained to the patient and maintained to ensure an empty stomach.
- Nurses were provided psychological support.
- Patient was shifted to OT for CABG + carotid endarterectomy.
Post OP Nursing Management
- The patient was transferred from the OT to CTICU for continuous cardiac monitoring and connected to ventilator.
- Nurses monitored and maintained vital sign every 15mins blood pressure stabilized with inotrope IV fluids.
- Nurses trained in intravenous infusion and blood sampling techniques, collected samples for CBC, ABG, RFT and electrolytes, etc.,
- Using sterile technique to prevent thrombophlebitis.
- The doctors explained the patient condition to attenders.
- Early upright position in and out of the bed as soon as possible after patient is woken up with endotracheal tube still in place.
- Inotropes tapered according to blood pressure.
- Early ambulation and mobilization done with the help of physiotherapist to prevent from deep vein thrombosis.
- All the bundles care followed properly to prevent from hospital acquired infection.
- Prior to discharge, off ventilator and encouraged the patient for deep breathing exercise by using respirometer.
- All the drains were removed and shifted to ward for further management on 5th POD and prepare for discharge.
- On 6th POD daily octenisan solution bath was given.
- On 8th POD patient condition improved and he was discharge in a stable hemodynamic status.
Conclusion
Coronary artery bypass grafting and carotid endarterectomy are both revascularization procedures aimed at reducing the risk of cardiovascular events. The focus should be on not only the immediate surgical intervention but also on long-term cardiovascular health and rehabilitation.
Recent Guideline and outcomes
Based on moderate quality evidence, the authors recommend carotid endarterectomy (CEA) in patients with ≥60–99% asymptomatic carotid stenosis considered to be at increased risk of stroke on best medical treatment (BMT) alone. They also recommend CEA for patients with ≥70–99% symptomatic stenosis, and they suggest CEA for patients with 50–69% symptomatic stenosis. Based on high quality evidence, CEA should be performed early, ideally within two weeks of the last retinal or cerebral ischemic event in patients with ≥50–99% symptomatic stenosis. Based on low quality evidence, carotid artery stenting (CAS) may be considered in patients < 70 years old with symptomatic ≥50–99% carotid stenosis. The results of another large trial comparing outcomes after CAS versus CEA in patients with asymptomatic stenosis are anticipated in the near future, that may influence treatment practices.
References
- Rerkasem A, Orrapin S, Howard DP, Rerkasem K. Carotid endarterectomy for symptomatic carotid stenosis. Cochrane Database Syst Rev. 2020 Sep 12;9(9):CD001081.
- Doonan RJ, Abdullah A, Steinmetz-Wood S, Mekhaiel S, Steinmetz OK, Obrand DI, Corriveau MM, Mackenzie KS, Gill HL. Carotid Endarterectomy Outcomes in the Elderly: A Canadian Institutional Experience. Ann Vasc Surg. 2019 Aug;59:16-20
- Morales MM, Anacleto A, Filho CM, Ledesma S, Aldrovani M, Wolosker N. Peak Systolic Velocity for Calcified Plaques Fails to Estimate Carotid Stenosis Degree. Ann Vasc Surg. 2019 Aug;59:1-4.
- Savardekar AR, Narayan V, Patra DP, Spetzler RF, Sun H. Timing of Carotid Endarterectomy for Symptomatic Carotid Stenosis: A Snapshot of Current Trends and Systematic Review of Literature on Changing Paradigm towards Early Surgery. 2019 Aug 01;85(2):E214-E225.
- Chang RW, Tucker LY, Rothenberg KA, Lancaster E, Faruqi RM, Kuang HC, Flint AC, Avins AL, Nguyen-Huynh MN. Incidence of Ischemic Stroke in Patients With Asymptomatic Severe Carotid Stenosis Without Surgical Intervention. 2022 May 24;327(20):1974-1982.
- Lal BK, Meschia JF, Brott TG, Jones M, Aronow HD, Lackey A, Howard G. Race Differences in High-Grade Carotid Artery Stenosis. 2021 Jun;52(6):2053-2059.
- Moore WS, Barnett HJ, Beebe HG, Bernstein EF, Brener BJ, Brott T, Caplan LR, Day A, Goldstone J, Hobson RW. Guidelines for carotid endarterectomy. A multidisciplinary consensus statement from the ad hoc Committee, American Heart Association. 1995 Jan;26(1):188-201.

