Effectiveness of Cardio Pulmonary Resuscitation (CPR) and its Outcome
Ramesh*1, Komathi2
1Staff Nurse, Emergency Department, Kauvery Hospital, Hosur,
2Nursing Incharge, Emergency Department, Kauvery Hospital, Hosur
Introduction
CPR is indicated for any person who is unresponsive, with no breathing or breathing only in occasional agonal gasps. It is most likely that the person is cardiac arrest.
If a person still has a pulse but is not breathing (respiratory arrest), artificial ventilations may be more appropriate.
But, lay people shall have difficulty in accurately assessing the presence or absence of a pulse, CPR guidelines therefore recommend that lay persons should not be instructed to check the pulse. But healthcare professionals have the option to check for a pulse. CPR is often futile in those with cardiac arrest due to severe trauma futile but still recommended. Correcting the underlying cause such as a tension pneumothorax or pericardial tamponade may help.
Incidence and Prevalence
In-hospital cardiac arrest (IHCA) or out-of-hospital cardiac arrest (OHCA) remains a significant and leading cause of mortality and morbidity worldwide, despite advanced technology and diagnosis. The incidence rate of cardiac arrest varies widely among hospitals, communities, and countries. In one study, an approximately 200,000 IHCAs were reported each year in the United States with <20% of the patients surviving to discharge.
The American Heart Association guidelines say that survival rates below 1% suggest futility, but most groups have better survival than that. Even among very sick patients, at least 10% survive: A study of CPR in a sample of US hospitals from 2001 to 2010, where overall survival was 19%, found 10% survival among cancer patients, 12% among dialysis patients, 14% over age 80, 15% among blacks, 17% for patients who lived in nursing homes, 19% for patients with heart failure, and 25% for patients with heart monitoring outside the ICU. Another study, of advanced cancer patients, found the same 10% survival mentioned above. A study of Swedish patients in 2007–2015 with ECG monitors found 40% survived at least 30 days after CPR at ages 70–79, 29% at ages 80–89, and 27% above age 90.
India’s bystander CPR rate sits between 1.3 percent and 9.8 percent, a rate that appears even more disconcerting when compared internationally. Countries with higher intervention rates owe much of their success to mandatory public Basic Life Support (BLS) training, where CPR is emphasized as a core public health skill. This becomes important as urban lifestyle factors—such as stressful environments, a lack of physical activity, and dietary changes—exacerbate the incidence of cardiac arrest. With less than 2 percent of India’s population formally trained in CPR, expanding public knowledge about CPR can save thousands of lives each year by increasing the likelihood of a bystander stepping in before medical help arrives.
Case presentation
A 49-year- aged woman with no co morbidities was brought to ER, at about 11 am,with giddiness, vomiting and pain over chest region and shoulder.
She was initially treated at an outside clinic and then came here for further management. On arrival patient was drowsy and went to bradycardia – followed by cardiac arrest.
History
Newly Diagnosed type -2 diabetes mellitus.
On examination
Systemic
- Airway – Patent
- Breathing – Respiratory rate; 38b/m, SpO2;84% on RA
- Circulation- Pulse; 60b/m, BP; 100/60 mm/hg
- Disability – GCS – 15/15Pupils 2mm , both are equally reacting to light
Physical: Patient was restless and disoriented.
On Admission
Around 11.30 am patient was still drowsy, and suddenly went into bradycardia followed by a cardiac arrest, CPR initiated as per ACLS protocol, after one cycle of CPR reverted spontaneous circulation.
Post cardiac arrest vital
HR – 72b/m
SPO2 – 90%on O2 support
BP – 80/60 mm/hg with Inj. Noradrenaline support
After half an hour around at 12.00pm patient again went to bradycardia, HR – 24b/m with absence of central pulse. CPR restarted as per ACLS protocol Inj. Atropine 1cc and Inj Adrenaline 1cc given IV stat. Patient reverted back. Emergency intubation done and connected to Mechanical Ventilator.
Drugs given during intubation
| S. No | Drugs | Dose |
|---|---|---|
| 1 | Inj. Midazolam | 2mg |
| 2 | Inj. Rocuronium | 100mg |
| 3 | Inj. Fentanyl | 100mcg |
| 4 | Inj Propofol | 3mg IV stat given. |
Post intubation vitals
BP – 100/60 mm of Hg with Inj.Noradrenaline support
PR – 102 beats per minute
SpO2 – 97% with Continuous Mechanical Ventilator mode of FiO2 100%.
At 12.45 pm
Again patient went to bradycardia . With multiple cycle of CPR and DC shock 100J given as per ACLS protocol, return of spontaneous circulation was attained.
Investigation
ECG – Showed atrial fibrillation with wide QRS and tail T wave
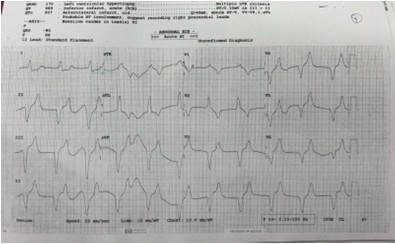
ABG – Showed severe metabolic and lactic acidosis
- PH – 6.93 mm/hg
- PCO2 – 16.5 mm/hg
- PO2 – 22.3 mm/hg
- HCO3 -5 mmol
- Lactate – 15.71
Echo cardiogram:
- CAD-RWMA (+)
- LV EF – 45%
- IVC – 1.8 cm
- Diastolic dysfunction grade 1
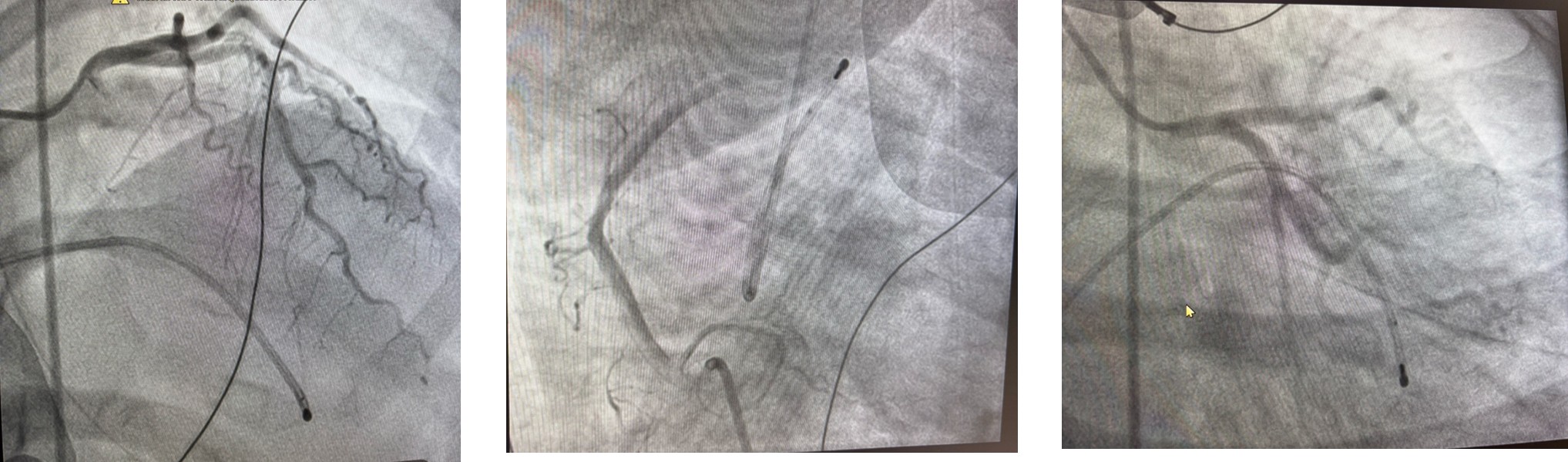
Discussed with cardiologist and planned for emergency TPI and CAG followed by dialysis for hyperkalemia and acidosis correction, Patient was shifted to cathlab and underwent emergency TPI through right femoral vein access and ventricular pacing done.
CAG done which revealed
- CAD – Branch vessel disease
- LAD – Type 3 vessel
- Mid LAD – Showed 30 – 40 % stenosis
- Diagonal – Medium sized vessel, normal
- LCX – Non dominant
- RCA – Dominant
- OM – Good sized vessel
The procedure was uneventful. After the procedure patient was shifted to ICU with IV fluids, Inotropic infusions with a mechanical ventilation support.
Diagnosis
- CAD – ACS – ? IWMI
- Moderate LV Dysfunction
- High grade AV block with bradycardia
- LRTI, NKDA
- Severe metabolic and lactic acidosis
- Hyperkalemia
- Recurrent in- hospital cardiac arrest
- Severe anemia of iron deficiency
- Bronchial asthma
Day – 1
- Patient on mechanical ventilator, GCS shown E4VTM6
- Periodic monitoring of ABG, RFT, Electrolytes and monitoring BP
- Inotropic infusion continued. Metabolic and lactic acidosis + hyperglycemia given accordingly.
- Emergency dialysis and 1 unit of PRBC transfusion done on date-01/01/2025.
- Antiplatelet and anti-coagulant medications continued.
Day-2
- As per cardiologist advice orders were followed
- Patient conscious and afebrile
- BP improved on Nor-adrenaline 2 ml/hr. BP-120/80 mmhg
- ABG improved
- HB improved from 6.5 to 8.9
- Output adequate
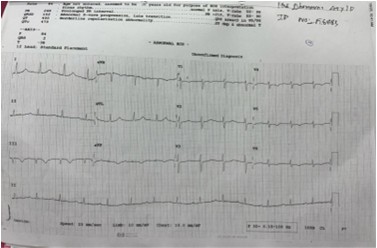
- On ventilation CPAP FiO2 40% spo2 maintained ECG shows 1:1 AV conduction
- Patient planned for extubation remove TPI after extubation
- Post extubation vitals stable, TPI removed
- Antibiotics continued.
Day-3
- Patient was obeying commands
- Improve spirometry
- IV medications and antibiotics and anti-platelets continued
- Nephrologist opinion sought, advised to remove HD catheter.
Day- 4
- Patient is stable and consc vitals are recorded with O2 support
- IV medications, antiplatelets, antibiotics were continued
- Oral diet has been encouraged
- Incentive spirometry given
- Mobilize in to chair
- PLAN: To remove CVC catheter
- Shifted to ward
Day- 5
- Patient is conscious and oriented. vitals are monitored continuously
- Patient on propped up position with O2 support by O2 mask
- IV medications along with antibiotics, anti-platelet drugs continued
- Chest physio therapy and incentive spirometry
- CVC catheter removed, vitals are stable without oxygen support.
- B/L crepts and hemodynamically stable, hence planned for discharge next day.
Condition at Discharge
General condition: Patient conscious and oriented and vital were stable.
- PR – 84 bpm
- BP – 130/80 mm/hg
- SPO2 – 96 % on RA
- CVS: S1S2
- RS: NVBS
- P/A: Soft
Medical Management
- Painkiller – morphine
- Anti-emetic – metoclopramide
- Anti-thrombotic& statin – aspirin, ticagrelor, atorva.
- Nitrate
- Oxygen 4liters per min
- IVF NS 50ml per hour
- GRBS every 4 hourly
- Anticoagulant – low molecular weight heparin, fondaparinux
- Thrombolytic – streptokinase
- Percutaneous Coronary Intervention
Nursing Management
- Monitored vital signs, including rhythm
- Monitored intake and output – Fluids 2 lit / day, 85 to 100 ml urine output/hour
- Provided comfortable position and environment to the patient.
- Incentive Spirometry: Encouraging deep breathing exercises to prevent atelectasis and promote lung expansion.
- Administer IV and PO medications as ordered – Anti platelets, Loop Diuretics, Anti diabetic agents, Mucolytic agents
- Encourage Family Involvement: Family members should be educated on the course of the disease, expected recovery trajectory, and how they can help care for the patient.
PTCA Health Education
- Keep the area dry where the catheter was inserted.
- Advice the patient to follow the medications order as per doctors prescribed
- Low fat diet, low potassium diet and life style modification
- Avoid strenuous activities
- Advice the patient for regular checkup.
- Advice the patient to continue the ROM exercise, Chest Physiotherapy and Spirometry.

