Functional short gut syndrome: A case capsule
Yamini Prakash1, Renuka Devi.K2, Kamali4, Nalini Sivakumar5
Lead clinical dietician, Department of Clinical Dietetics, Alwarpet unit, Chennai
Senior clinical dietician, Department of Clinical Dietetics, Alwarpet unit, Chennai
Clinical dietician, Department of Clinical Dietetics, Alwarpet unit, Chennai
Clinical dietician, Department of Clinical Dietetics, Alwarpet unit, Chennai
Background
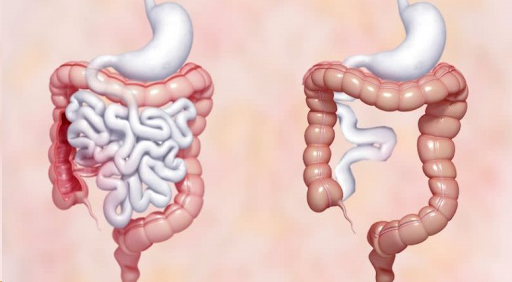
Functional Short gut syndrome is a group of problems related to poor absorption of nutrients. Short gut syndrome cannot absorb enough water vitamins, minerals, protein, fat, calories and other nutrients from food. Short gut (bowel) syndrome typically occurs in people who have
- Had at least half of their small intestine removed and sometimes all or part their large intestine removed.
- Significant damage of the small intestine.
- Poor motility, or movement, inside the intestines.
Short bowel syndrome may be mild, moderate or severe depending on how well the small intestine is working.
Expected signs and symptoms
- Bloating
- Cramping
- Fatigue, or feeling tired
- Foul smelling stools
- Heart burn
- Too much gas
- Vomiting
- Weakness
Case presentation
Admission 1
D.O.A: 24/11/2022; D.O.D: 26/11/2022
A 41 years male, with the complaints of recurrent vomiting with abdomen distention diagnosed- small bowel obstruction with perforation peritonitis on 3/11/2022, underwent laparotomy with small bowel resection and ileostomy on 4/11/2022 in outside hospital, now came here for further management.
Patient came with the complaint of history of weight loss, vomiting, nausea, loose stools, and dysuria and also had complaints of weakness, fatigue, tiredness and the patient had a huge volume of output in via ileostomy.
The provisional diagnosis
Post Laparotomy status Small Bowel Resection with End of Illeostomy (Short Bowel Syndrome)
Admission 2
D.O.A: 3/1/2023; D.OD:6/1/2023
Patient came with the complaint of history of giddiness and fall sustained injury in right frontal region, swelling for 2 days back and also had a history of decreased urine output since 4 weeks.
No other complaints like vomiting, nausea, seizures. As diagnosed syncope 2nd degree postural hypotension and AKI. Treatment Plan: Electrocardiogram was taken which is normal and colonoscopy was planned.
Admission 3
D.O.A: 12/1/2023; D.O.D:24/1/2023
Patient came with the complaint of fever on and off for 2 days, he is a known case of crohn’s disease – S/P ileostomy. Patient was on Home TPN since 1 week. Patient admitted for ileostomy reanastomosis. He is a known case of functional gut syndrome and s/p crohn’s ileostomy bag in November 2022. Patient doesn’t have any other gastric symptoms; necessary investigations were done TPN line was removed. Surgical gastroenterologist opinion obtained and planned for reanastomosis.
Nutrition Care Process
Anthropometric Data
Height |
175cms |
Weight |
56.2kgs(24/11/2022) |
BMI |
18.3kgm2 According to WHO BMI classification patient falls under underweight category. |
Ideal Body Weight |
58kgs-73kgs |
Biochemical Data: Admission 1
Vitals |
24-11-2022 |
24-11-20222 |
24-11-2022 |
| HB | 11.6 | ||
| PCV | 36.7 | ||
| WBC | 13500 | ||
| Platelets | 4,47,000 | ||
| Neutrophils | 94.7 | ||
| Lymphocytes | 2 | ||
| Monocytes | 2.6 | ||
| Basophils | 0.4 | ||
| Urea | 26.9 | ||
| Creatinine | 0.79 | ||
| Sodium | 137.6 | ||
| Potassium |
6.7 |
5.2 |
5.98 |
| Chloride | 105.2 | ||
| Bicarbonate | 20.2 | ||
| T. Bilirubin | 1.15 | ||
| D. Bilirubin | 0.58 | ||
| I. Bilirubin | 0.57 | ||
| SGOT (AST) | 88.6 | ||
| SGPT | 184.7 | ||
| T. Protein | 7.27 | ||
| Albumin | 4.07 | ||
| CRP | 16.08 | ||
| Magnesium | 1.9 |
Biochemical Data: Admission 2
Vitals
|
03-01-2023 |
04-01-2023 |
| HB | 12.9 | |
| PCV | 38.6 | 38.7 |
| WBC | 7100 | |
| Platelets | 1,86,000 | |
| Neutrophils | 79 | |
| Lymphocytes | 6.9 | |
| Monocytes | 11 | |
| Basophils | 0.3 | |
| Urea | 33.1 | |
| Creatinine |
1.66 |
1.2 |
| Sodium | 133 | 137.4 |
| Potassium | 4.92 |
3.66 |
| Chloride | 84 | 64.3 |
| Bicarbonate | 38.6 | 28.2 |
| T. Cholesterol | 126 | |
| TGL | 225.9 | |
| LDL | 52.1 | |
| VLDL | 45.2 | |
| CHOL/HDL | 3.6 | |
| T. Protein | 7.99 | |
| Albumin | 5.17 | |
| Globulin | 2.82 | |
| Ferritin | 34.95 | |
| CRP | 8.71 |
Biochemical Data: Admission 3
Vitals |
12-01-2023 |
15-01-2023 |
17-01-2023 |
23-01-2023 |
| HB | 8.8 | 8.4 | ||
| PCV | 25.8 | 24.3 | ||
| WBC | 5000 | |||
| Platelets | 85,300 | 414000 | ||
| Neutrophils | 84 | |||
| Lymphocytes | 4.3 | 6.2 | ||
| Monocytes | 9.4 | 6.6 | ||
| Basophils | 0.8 | 0.2 | ||
| Urea | 14.5 | 12 | ||
| Creatinine | 0.76 | 0.67 | ||
| Sodium | 143 | 144 | ||
| Potassium | 3.5 | 3.13 | ||
| Chloride | 111.1 | 107.2 | ||
| Bicarbonate | 23.2 | 29.4 | ||
| T.Bilirubin | 0.47 | |||
| D.Bilirubin | 0.24 | |||
| I.Bilirubin | 0.23 | |||
| SGOT (AST) | 38.8 | |||
| SGPT | 30.6 | |||
| T. Protein | 5.48 | |||
| Albumin | 2.88 | |||
| Globulin | 2.6 | |||
| S. Uric Acid | 3.88 | |||
| S. Phosphorus | 4.15 | 2.93 | ||
| S. Calcium | 7.91 | |||
| SAP | 67.6 | |||
| PTT | 13 | |||
| INR | 1.14 | |||
| C | 11.4 | |||
| RBC | 2.95 | |||
| MCH | 28.5 | |||
| MCV | 82.2 | |||
| MHC | 34.7 | |||
| Dengue IgG | POSITIVE | |||
| CRP | 50.7 |
Clinical Data- first two admissions
Chief Complaints |
Drastic weight loss, loose stools, nausea, vomiting, fatigue, tiredness and weakness. |
Diagnosis |
Post Laparotomy status small bowel resection with end of ileostomy short bowel syndrome. |
History of Past Illness |
Laparotomy with small bowel resection and ileostomy on 4/11/2022. |
Plan of Treatment |
Medical Management Peripheral TPN @ 30ml/ hourly adequate oral soft high protein diet |
Vitals: Admission 1
| BP | 90/60mg | |||
| Pulse | 104bpm | |||
| RespirationRate | 18b/min | |||
| Spo2 | 97% | |||
| Temperature | 98.1F | |||
| CBG | 106mg/dl | |||
| GCS | E4 V5 M6 | |||
Vitals |
03-01-2023 |
04-01-2023 |
05-01-2023 |
06-01-2023 |
| BP | 80/60 | 105/60 | 100/60 | 100/60 |
| Pulse | 78/bpm | 80/bpm | 68/bpm | 68/bpm |
| RR | 20b/min | 20b/min | 20b/min | 20b/min |
| Temperature | 98.1F | 98.1F | 98.1F | 98.1F |
| SPO2 | 100% | 98% | 100% | 100% |
| CBG | 125mg/dl | |||
| GCS | 15/15 |
Vitals: Admission -2
Vitals |
12/1 |
13/1 |
14/1 |
15/1 |
16/1 |
17/1 |
18/1 |
19/1 |
20/1 |
21/1 |
22/1 |
23/1 |
| BP | 110/80 | 100/70 | 100/70 | 110/70 | 125/80 | 130/80 | 130/80 | 130/80 | 120/80 | 130/80 | 130/80 | |
| Pulse | 128/BPM | 84/BPM | 82/BPM | 82/BPM | 82/BPM | 81/BPM | 82/BPM | 82/BPM | 82/BPM | 85/BPM | 74/BPM | 74/BPM |
| RR | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM | 20/BPM |
| Temp | 104.3F | 98.4F | 98.4F | 98.4F | 98.4F | 98.4F | 98.4F | 98.4F | 99.2 | 98.4F | 98.4F | 98.4F |
| SPO2 | 98% | 98% | 98% | 98% | 98% | 98% | 98% | 98% | 97% | 97% | 97% | 97% |
| CBG | 112mg/dl | 104mg/dl | 98mg/dl | |||||||||
| GCS | 15/15 |
Vitals: Admission – 3
Dietary Assessment
| Diet Habits |
|
| Food Allergies | Nil |
| Energy | 2000kcals(30kcals/kgIdealbodyweight) |
| Protein | 87g(1.2g/kgIdealbodyweight) |
| Carbohydrate | 60%ofTotalCalories |
| Fat | 25%ofTotalCalories |
| Fluids | Liberal |
| Salt | 6grams/day |
| Micronutrients | AsperRDA |
Patient was following normal diet due to frequent output in ileostomy bag was high. Patient family was feeding him every 30 minutes like chocolates, beverages, and juices etc.
Medical Nutrition Therapy
SubjectiveGlobalAssessment
|
Severely Malnourished
(complaints of weight loss 8kgs in past 1 week) |
Nutrition Prescription
Diet Compliance: Oral Nutrition Supplement and Total Parenteral Nutrition was initiated as a part of nutrition prescription Oral soft bland diet plan was initiated and educated to patient and family.
PES Statement
| Problem | Etiology | Symptom | ||
| Altered
GI Function |
Relatedto | Short
Bowel Syndrome |
as
evidenced by |
Weight Loss,
tired Ness, loose Stools, fatigue and weakness |
Hospital Diet History – Admission 1
| Day | Date | TypeofDiet | Energy
(kcals) |
Protein(g) | Remarks |
| 1 | 24-11-2022 | TPN@30ml/hrlyinitiatedwithONS-2timesaday+oralsoft blanddiet
Totalvolume:660ml(TPN Oraldiet |
1064kcals | 35g | Bowelopeningassoonasfoodintake.Bowelrestwassuggested |
| 2 | 25-11-2022 | TPN @60ml/hr increased + ONS – 2 times a day + soft bland dietTotal volume: 1340ml (TPN)
Oral diet |
1838kcals | 64g | Only2ndhourlyoralfeedssuggested |
| 3 | 26-11-2022 | TPN@40ml/hrlymodified+ONS-2timesaday+softblanddiet | 1845kcals | 70g | StoppedTPN,oralsoftsolidhighproteinMCTRichDietwaseducatedondischarge |
Hospital Diet History – Admission 2
Days |
Date |
Typeofdiet |
Energy |
Protein |
Remarks |
| 1 | 03-01-2023 | NPO | For colonoscopy | ||
| 2 | 04-01-2023 | High protein diet + ons thrice a day | 1300kcal | 44gms | TPN initiated with high protein diet |
| 3 | 05-01-2023 | High protein diet + tpn initiated + ons thrice a day | 1759kcal | 70gms | Intake was fair
No GI symptoms |
| 4 | 06-01-2023 | High protein diet + tpn initiated + ons thrice a day | 2010kcal | 84gms | Suggested to follow home tpn for next 7 days and suggested follow low fat high protein mct based diet |
Days |
Diet |
Energy(Kcals) |
Protein(G) |
| DAY1 | Tpn+oralhighproteinsoftsoliddiet
1100kcals+500kcal/50g+25g |
1600kcals | 75g |
| DAY2 | Tpn+oralhighproteinsoftsoliddiet
1100kcals+750kcal/50g+35g |
1850kcals | 85g |
| DAY3 | Tpn+oralhighproteinsoftsoliddiet
1100kcals+700kcal/50g+38g |
1800kcals | 88g |
| DAY4 | Tpn+oralhighproteinsoftsoliddiet
1100kcals+800kcal/50g+40g |
1900kcals | 90g |
| DAY5 | Tpn+oralhighproteinsoftsoliddiet
1100kcals+900kcal/50g+45g |
2000kcals | 95g |
| DAY6 | Tpn+oralhighproteinsoftsoliddiet
1100kcals+900kcal/50g+40g |
2000kcals | 90g |
| DAY7 | Tpn+oralhighproteinsoftsoliddiet
1100kcals+1000kcal/50g+55g |
2100kcals | 105g |
Home Care Nutrition
Advised TPN (total parental nutrition) – 1
Hospital Diet History: Admission – 3
| Days | Date | TypeofDiet | Energy | Protein | Remarks |
| 1 | 13-1-2023 | HighProteinDiet+ONS | 1847Kcal | 72g | Intakewasgood |
| 2 | 14-1-2023 | HighProteinDiet+ONS | 2609Kcal | 85g | |
| 3 | 15-1-2023 | HighProteinDiet+ONS | 2062Kcal | 70g | |
| 4 | 16-1-2023 | NPOforsurgery | nil | nil | PostedforIleostomyclosure |
| 5 | 17-1-2023 | NPOpostoperatively | nil | nil | |
| 6 | 18-1-2023 | NPOpostoperatively | nil | nil | |
| 7 | 19-1-2023 | NPOpostoperatively | nil | nil | |
| 8 | 20-1-2023 | Oralclearliquiddietstartedat30ml/hourly | 100Kcal | 2g | |
| 9 | 21-1-2023 | OralClearLiquiddiet | 250Kcal | 10g | oralliquidsprogressed |
| 10 | 22-1-2023 | OralLiquiddiet | 440Kcal | 19g | Oralsoftdietmodified |
| 11 | 23-1-2023 | Highproteinsoftdietmodified | 500Kcal | 26g | StartedONSThriceaDay |
| 12 | 24-1-2023 | Highproteinsoftdietmodified | 1000Kcal | 55g | Educatedpatientandfamilyabouthighproteindietondischarge |
Nutrition Intervention Goals
Short Term Goals
- To improve oral intake and to prevent nutrition deficiencies.
- To control inflammatory markers.
- To use high protein diet, Tpn and other oral semi elemental supplementation. If needed.
Long Term Goals
- To facilitate nutrition well-being of the patient.
- To promote quality life of the patient.
Anthropometric Data
Height |
175 cms |
Weight |
62kgs(13/1/2023) |
BMI |
20.2 kg/m2
According to WHO BMI classification patient falls under Normal weight category |
Ideal Body Weight |
58kgs to 73 kgs |
Summary
A X 41 years male underwent laparotomy with small bowel resection and ileostomy on 4/11/2022 in outside hospital, now came with the complaint of history of weight loss, vomiting, nausea, loose stools, dysuria and also had complaints of weakness, fatigue, tiredness and the patient said that whatever he takes orally and output in the ileostomy bag was high.
Patient was following normal diet due to frequent output in ileostomy bag was high. Patient family was feeding him every 30 minutes like chocolates, beverages, and juices. But his SGA was Severely Malnourished, Had complaints of weight loss 8 kgs in past 1 week, as a part of nutrition plan Oral Nutrition Supplement and Total Parenteral Nutrition was initiated with
Oral soft bland diet with small frequent meals High protein Mct rich diet was educated to family and patient on discharge.
On 2nd admission, patient complaints of giddiness and fall sustained injury in right frontal region, swelling for 2 days back and also had a history of decreased urine output since 4 weeks. No other complaints like vomiting, nausea or seizures. Diagnosed as syncope 2nd degree postural hypotension and AKI. Electrocardiogram was normal and Colonoscopy finding was Diversion Colitis, Crohn’s, S/P Ileostomy.
There is increase in the weight and his ileostomy output was reduced when compare to previous admission. Patient diet initiated with TPN and oral high protein Mct rich diet. while discharge patient and family educated on same and Prescribed Home parenteral nutrition for 1 week and recall of High Protein Diet was recorded and followed up at home.
On 3rd admission, patient complaints of fever on and off for 2 days, he is a known case of crohn’s disease S/P ileostomy was on TPN. Patient admitted for ileostomy re anastomosis. He is a known case of functional gut syndrome and s/p crohns ileostomy bag in November 2022. Necessary investigations revealed that elevated CRP and Dengue IgG was positive. TPN line was removed patient underwent re anastomosis post procedure was uneventful. Pre and post procedure oral intake was monitored regularly and patient tolerated the feeds well, patient improved clinically and symptomatically hence discharged with High protein Diet.
KCH Clinical Dietician Team.


