Infective Endocarditis
Vijayalakshmi G 1,* , Suriya2 ,
1 Non Critical Ward Incharge, Kauvery Heartcity, Trichy, India
2 Non Critical Ward Senior Staff Nurse, Kauvery Heartcity, Trichy, India
Background
Infective Endocarditic is an infection of the endocardial surfaces of the heart, usually of one or more cardiac valves, and to a lesser degree of the mural endocardium or a septal defect.
Endocarditis was first described by Sir William Osler in 1885. It is an inflammatory process that affects the endocardium and may have an infective or non-infective (e.g. systemic luples erythematosus) origin. It is uncommon in the Western world (22 cases million) but more prevalent in developing countries.
Infective endocarditis is a rare, and life-threatening disease, that has long-lasting effects even among patients who survive and are cured. Infective endocarditis disproportionately affects those with underlying structural heart disease and is increasingly associated with healthcare contact, particularly in patients who have intravascular prosthetic material. In the setting of bacteraemia with a pathogenic organism, infected vegetation may form as the end result of complex interactions between invading micro-organisms and the host immune system. Once established infective endocarditis can involve almost any organ system in the body.
The diagnosis of infective Endocarditic may be difficult to establish. A strategy that combines clinical, microbiological and echocardiography data has been codified in the modified Duke criteria, in cases of blood culture – negative, infective endocarditis. The diagnosis may be especially challenging and novel microbiological and imaging techniques have been developed to establish its presence. Once diagnosed infective endocarditic is best managed by a multidisciplinary team with expertise in infectious diseases, cardiology and cardiac surgery.
Antibiotic prophylaxis for the prevention of infective endocarditis is available but its faith full following remains suspect. Efforts to develop a vaccine that targets common bacterial causes of infective endocarditic are ongoing, but have not yet yielded a commercially available product.
Infective Endocarditis
Infective endocarditis is characterized by lesions known as vegetations, which is a mass of platelets, fibrin, micro colonies of microorganisms and scant inflammatory cells. In the subacute form of infective endocarditic, the vegetation may also include a centre of granulomatous tissue which may fibrosis or calcify.
Infective Endocarditis: Symptoms
- Aching joints and muscles.
- Chest pain on breathing.
- Fatigue.
- Flu- like symptoms such as fever and chills.
- Night sweats.
- Shortness of breath
- Swelling in the feet legs or belly.
- A new or changed murmur in the heart .
- Skin rash.
- White patches in mouth or on tongue.
- Nausea, vomiting or diarrhea.
Causes
Most of the times a bacterial infection may lead to endocarditis. Dental procedures (particularly tooth extractions) and endoscopic examinations and can cause bacteria to get into blood. Sometimes bacteria from mouth, skin, intestines and respiratory system or urinary tract may be able to get into bloodstream when eating, brushing or flossing teeth. The bacteria rapidly form colonies, grow vegetations and produce enzymes, and destroying the surrounding tissue. Normal heart valves are very resistant to infection; however, bacteria can attach to defects on the surface of diseased valves. Replacement heart valves are more prone to infection than normal valves.
Diagnostic Tests
Blood Culture
: Blood cultures, taken over time, allow a laboratory to isolate the specfic bacteria that are causing the infection. To secure a diagnosis the lab must take blood culture before taking antibiotics (3 to 5 set of blood cultures over 24hrs, 3 sets may be drawn over 30min with separate venipuncture).
Complete Blood Count
may show an unusually high number of white blood cells, indicating an infection.
ESR
(Erythrocyte Sedimentation Rate)
Blood Tests
for Cc – reactive protein can indicate infection and inflammation.
ECHO Cardiogram:
may show growth (vegetations on the valve) new reurgititation (leaking) or stenosis (narrowing), or an infected artificial heart valve. Trans Esophageal Echo can harvest more informative images than Transthoracic Echo ( TTE).
Culture or heart valve tissue culture
to find out the bacterial species and to determine its antibiotic sensitivity .
Positron emission tomography (PET) or Nuclear Medicine Scans
to create images using radioactive material than can show an infection’s location.
Treatment
The type of medication depends on what’s causing the endocarditis . High doses of IV antibiotics are used to treat endocarditic caused by bacteria and are continued till infection is controlled
Antibiotics are usually taken for several weeks.
If endocarditis is caused by fungal infection antigungal medication is givben. Some people need lifelong antifungal pills to prevent endocarditic from returning.
Surgery or other procedures
Heart valve surgery may be needed to treat persistent endocarditic infections or to replace a damaged valve. Surgery is sometimes needed to treat endocarditis that’s caused by a fungal infection.
Depending on the specific condition, heart valve repair or replacement may be required .
Nursing Management
Nursing management includes the following aspects.
- The nurse monitors the patient’s temperature.
- Heart sounds assessed (a new or worsening murmur may indicate dehiscence of a prosthetic valve, rupture of an abscess or injury to valve leaflet).
- The nurse monitors for signs and symptoms of systemic embolization.
- In addition the nurse assesses signs and symptoms of organ damage such as stroke (CVA) meningitis heart failure, myocardial infarction, glomerulonephritis and splenomegaly.
- All invasive lines and wounds must be assessed daily for redness and swelling.
- After discharge the nurse supervises and monitors IV antibiotic therapy delivered in the home setting and educates the patient and family about prevention and health promotion.
- The nurse provides the patient and family with emotional support and facilitates hoping strategy during the prolonged course of the infection and antibiotic treatment.
- To encourage practice good oral hygiene and dental hygiene.
Case Presentation
- A 39 years male patient had fever since 1 month.
- He had h/o Mitral valve prolapse, PML (P2 Segment Prolapse).
- Severe mitral regurgitation.
- Good LV function.
- Type II DM and SHT, 2 years’ regular treatment.
- Infective endocarditis of mitral valve.
Investigation
ECHO:
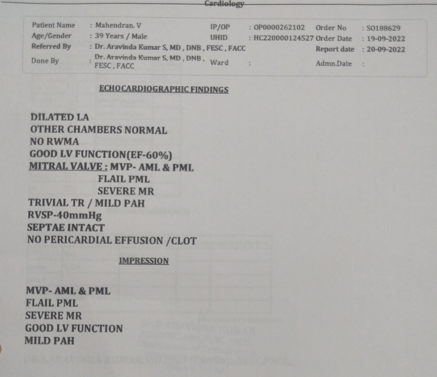
- Possible infective endocarditis of mitral valve.
- Mitral valve prolapsed – PML (P2 segment prolapse).
- Severe Mitral regurgitation.
- Good LV function.
- Mild pulmonary artery hypertension.
ECG:
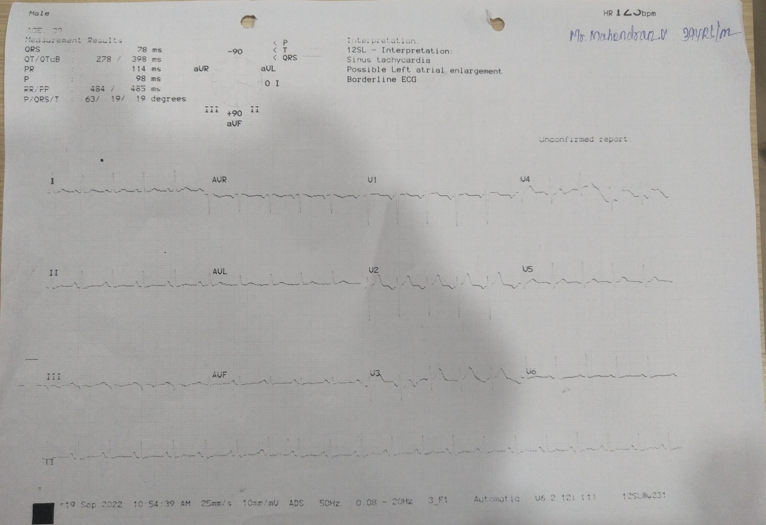
Normal sinus rhythm.
No significant – ST – T Changes.
TEE:
- Showed infective endocarditis of mitral valve AMP – PML
Blood Culture:
- Sterile for aerobic and anaerobic incubation.
Blood Investigation:
- Elevated CRP and elevated ESR.
USG Abdomen:
- Mild splenomegaly with tiny focal lesion.
Diagnosis
- Infective endocarditis of mitral valve
- Mitral valve prolapse (P2 segment Prolapse)
- Severe Mitral regurgitation.
- Good LV function.
- Normal sinus rhythm.
- Type II Diabetes mellitus.
- Systemic hypertension.
Vital Signs
BP:
120/80mmHg
HR:
72bpm
CVS:
murmur
Rs:
BAE Positive
P/A:
Soft
CNS:
Within Normal limits
Summary
A 39years old diabetic and hypertensive known case of MVP, PML had complaints of recurrent fever for 1 month for which he was initially evaluated at an outside hospital and then referred here for further management. On examination t,he patient was conscious, oriented and vitals were stable with no significant ST – T changes on ECG and ECHO revealed severe MR with Good LV function.
In view of above findings patient was advised admission for further management. TEE showed infective of mitral valve, AMP- PML (P2 segment prolapsed with Severe MR). His blood culture and sensitivity is sterile for aerobic and anerobic incubation.
His blood investigations revealed elevated CRP, elevated ESR. His USG abdomen revealed mild splenomegaly with tiny focal lesion. Patient was treated with antibiotics, beta blockers, hypoglycemic agents, PPI and other supportive measure. Patient condition is improved and is being discharged in a stable state.
Medications
Inj. Ceftriaxone 2 g IV OD 1-0-0 x 6 weeks
Tab. Concor 2.5 mg 1-0-1
Tab.Pantocid 40 mg 1-0-0 (B/F)
DM Advice
Inj. Novarnix 50/50 Units 8-0-0
Tab. Cetapinxr 500 mg 0-0-1 (A/F)
Conclusion
After a long stay in the hospital, the patient became stable with the efficient care of nurses and got discharged.

