Infective Endocarditis (IE)
Emalda Mary. A1*, Lamya begum2
1Nursing Incharge, Kauvery Hospital, Tennur
2Staff Nurse, Kauvery Hospital, Tennur
Abstract
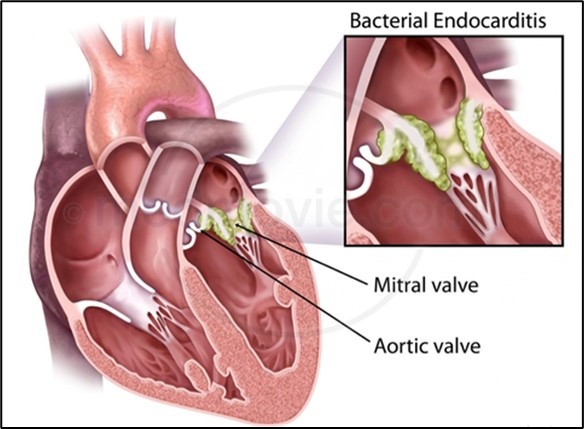
Infective Endocarditis (IE) is the term that denotes a bacterial, viral or fungal infection of the endocardial surfaces of the heart—usually those of one or more cardiac valves, to a lesser degree the mural endocardium or a septal defect. Such may produce severe valvular insufficiency, intractable congestive heart failure, myocardial abscesses, infected and sterile emboli, and initiate a variety of immunological processes.
Infective endocarditis (IE) is a life-threatening cardiac infection and is predisposed to occur in some individuals with multiple cardiac valve conditions. Infective endocarditis affects 14.5 cases per 100000 patient-years in India, which is very high compared to the western incidence, which is around 1.7 – 6.2, cases per 100000 patient-years. Incidence rate increases progressively with ageing, from 50 years of age.
Case Presentation
A 35 years aged gentleman was admitted with a notable past history of intermittent fever and polyarthralgia. He consulted a Rheumatologist and was started on steroids.
He had DM since Feb 2023, was on regular treatment.
He was admitted with complaints of severe joint pain all over the body and intermittent fever at night for two days. Subsequently, the patient also reported persistent fever and bilateral pain in the knee joints.
On examination, the patient was conscious and oriented. GCS-15/15, PR-120 beats/min, BP – 130/70 mm Hg, Spo2 92% in room air, RR 22 breath/min.
The patient underwent a complete blood count (CBC) examination, which indicated the presence of leukopenia with severe neutropenia and a reduction in platelet count. A hematologist opinion was obtained.
A blood culture was sent and it revealed the presence of streptococcus mutants. Treatment was initiated with Inj. Ceftriaxone and Inj. Gentamycin for a duration of 14 days. 1 unit PRBC was transfused
Our team diligently observed important indicators, including heart rate and blood pressure.
Patient developed signs of heart failure and pulmonary edema, patient had desaturation and tachypnea (RR – 48/min). Diuretics were administered and Inj. Targocid was included in the treatment plan.
Echo was done and it revealed:
- Sub-acute infective endocarditis of bicuspid aortic valve.
- Both leaflets were thickened, vegetation was noted attached to aortic valve (12cm), non-dilated arch of aorta
- Severe eccentric Aortic Regurgitation (AR).
The patient required urgent surgery and was transferred to Heart City for further surgical treatment. Surgical Management where the patient later underwent a significant surgical procedure known as open heart surgery to replace the aortic valve with a mechanical valve.
The patient was admitted to the Intensive Care Unit.
Transesophageal Echocardiogram (TEE) was done which showed severe AR and large mobile vegetation in aortic valve.
Repeat blood culture was sent. It was sterile.
In light of the persistent fever, Inj. Vancomycin was initiated and AV replacement was recommended once the active infection has been resolved. The patient received a five-day course of antibiotics before undergoing Aortic valve replacement surgery. Aortic valve replacement surgery was performed on September 1, 2023.
We ensured that fluid intake was carefully monitored to prevent the risk of fluid overload. Patient was stable vitals are normal and discharged with stable conditions.
Nurses’ Responsibilities
Monitor Vital Sigs
Our team will carefully monitor vital signs, such as heart rate and BP. They may hook you up to several machines so the nurses can check these more easily.
- Universal precaution for infection control to prevent endocarditis and decrease rheumatic fever
- Symptom management
- Monitor signs and symptoms of deep vein thrombosis
- Elevate legs above the heart
- Monitor fluid intake to avoid fluid overload
- Assess ECG
- Monitor INR
- Listen to the lungs as pulmonary edema is common
- Listen to the heart-MS presents with a loud S1
- Encourage diet (Failure to thrive is common
- Educate patients on the disease and surgery
Monitor INR
Patients who undergo mechanical heart valve replacement need lifelong anticoagulation therapy and INR was regularly measured to adjust the anticoagulation strength. After mitral valve replacement the INR was 2.0-2.5.
Monitoring I/O
Fluid restriction is used as a way to avoid over loading of heart. More fluid in the blood stream makes it harder for heart to pump.
Monitoring hourly urine output to evaluate for responses to pharmacologic interventions. Patient recovered to a urine output of 1000 – 2000 ml/24 hrs.
Oxygen administration
Achieved spo2 valve of at least 94%. Provided supplemental oxygen to maintain adequate oxygenation and to prevent any respiratory acidosis or improve oxygenation.
Administering Medication
Used antibiotics to treat bacterial infection (endocarditis).
Health education
Dressing
We instructed the attendant to change the dressing every three times per week. The wound was kept dry, and antiseptic cream was not applied under the dressing.
Breathing Exercise
We instructed the patient to focus on breathing exercises at home during the first two weeks after discharge. Advised that ambulation and other activities should gradually progress from slow walking and range of motion (ROM) exercises to include activities of daily living.
Diet
We have instructed to eat healthy foods; to include foods that were low in salt, fat or cholesterol. Healthy options include fruits, vegetables, whole grain breads, low-fat dairy products, beans, lean meats and fish.
Medication
We instructed the patient and attendants to take antibiotics and anticoagulants to help prevent blood clots.
We instructed the patient to call the doctor if they experience,
- If a patient experiences chest pain or persistent shortness of breath that does not improve with rest after open heart surgery for mitral valve replacement with a mechanical valve
- If the pain around your surgical incision doesn’t improve as expected or worsens over time, despite home care.
- A pulse that is very slow (fewer than 60 beats per minute) or very fast (over 100 to 120 beats per minute) should be evaluated.
- You have cough swelling coughing up with blood or yellow or green mucus.
- If you’re having trouble taking any medications prescribed for your heart condition, this needs attention to ensure proper treatment.
- Watch for signs such as increased redness, swelling, opening of the wound, or drainage from it, as these could indicate infection.
- A fever over 101°F accompanied by chills could suggest an infection, which needs prompt evaluation and treatment.
Conclusion
Bacteria, fungi or other germs get into the bloodstream and attach to damaged areas in the heart. Things that make one more likely to get endocarditis are artificial heart valves, damaged heart valves or other heart defects. Without quick treatment, endocarditis can damage or destroy the heart valves and are life- threatening.
Certain precautions can be taken in order to prevent this disease.

