Yamini Prakash
Chief Dietician, Department of Clinical Nutrition and Dietetics, Kauvery Hospital, Chennai
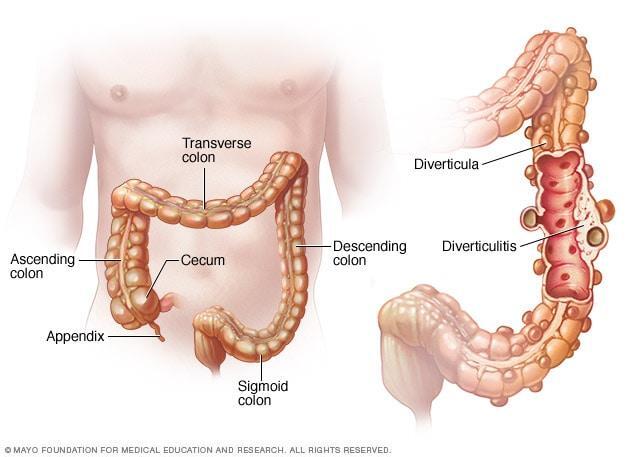
Nutrition care process for Sigmoid Diverticulitis
Background
Diverticulitis (inflammation) develops when bacteria or other irritants are trapped in the pouches, causing spasm and pain in the lower left side of the abdomen, as well as distention, nausea, vomiting, constipation or diarrhea, chills, and fever. Bowel cancer has been associated with the presence of diverticular disease.
Symptoms and signs
The signs and symptoms of diverticulitis include:
- Pain – which may be constant and persist for several days. The lower left side of the abdomen is the usual site of the pain. Sometimes, the pain may occur on the right side of the abdomen.
- Nausea and vomiting.
- Fever
- Abdominal tenderness.
- Constipation or, less commonly, diarrhea.
Risk Factors
Several factors may increase the risk of developing diverticulitis;
- Aging; the incidence of diverticulitis increases with age
- Obesity: Being seriously over weight increases the odds of developing diverticulitis
- Smoking: people who smoke cigarettes are more likely than non-smokers to experience diverticulitis.
- Lack of exercise; vigorous exercise appears to lower the risk of diverticulitis.
- Diet high in animal fat and low in fibre. A low fibre diet in combination with a high intake of animal fat seems to increase risk.
- Several drugs are associated with an increased risk of diverticulitis, including steroids and opioids.
Case Presentation
A 62 year old male with k/c/o sigmoid diverticulitis, post Hartmann’s procedure for sigmoid diverticulitis, post polypectomy on pedunculated polyp in sigmoid colon, had been admitted for further management.
Past History
The patient was known to a have Hypertension and history of CAD and Stroke.
Surgical Management
Colonoscopy was planned, the patient had already undergone Laparotomy, Anastomosis, Re- laparotomy and Tracheostomy.
Nutrition Care Process
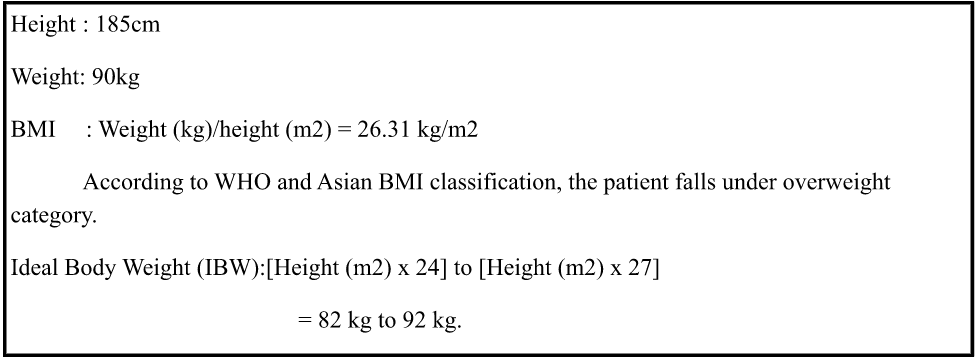
1. Anthropometric Data
2. Biochemical Data
| DAYS | DATE | Urea | Creatinine | Na | K+ | Cl2 | HCo3 | Sr. Uric acid | |
| DOA | 12/6/2021 | ||||||||
| Day 1 | 12/7/2021 | 141 | 4.1 | ||||||
| Day 2 | 12/8/2021 | ||||||||
| Day 3 | 12/9/2021 | 32.4 | 1.22 | 140 | 4.4 | 104 | 20.6 | ||
| Day 4 | 12/10/2021 | 39.7 | 1.08 | 139 | 4.5 | 105 | 22.6 | 5.69 | |
| Day 5 | 12/11/2021 | ||||||||
| Day 6 | 12/12/2021 | ||||||||
| Day 7 | 12/13/2021 | 37.4 | 0.85 | 138 | 4.2 | 103 | 21.7 | ||
| Day 8 | 12/14/2021 | 49.4 | 0.86 | 142 | 4 | 105 | 19.3 | 4.93 | |
| Day 9 | 12/15/2021 | 78.9 | 1.63 | 142 | 4.6 | 107 | 17.4 | 7.17 | |
| Day 10 | 12/16/2021 | 75.2 | 1.32 | 144 | 4.5 | 108 | 17.1 | 7.54 | |
| Day 11 | 12/17/2021 | 93.1 | 1.3 | 147 | 4.4 | 109 | 18.6 | 7.91 | |
| Day 12 | 12/18/2021 | 109.2 | 1.19 | 150 | 4 | 113 | 17 | 8.45 | |
| Day 13 | 12/19/2021 | 93.3 | 1.14 | 155 | 4.4 | 116 | 17.7 | 6.88 | |
| Day 14 | 12/20/2021 | 85.7 | 1.11 | 158 | 4.1 | 120 | 19.8 | 6.11 | |
| Day 15 | 12/21/2021 | 72.6 | 0.95 | 159 | 3.7 | 121 | 19.8 | 4.55 | |
| Day 16 | 12/22/2021 | 145.9 | 2.64 | 158 | 6.1 | 121 | 17.5 | 7.38 | |
| Day 17 | 12/23/2021 | 198.7 | 4 | 154 | 4.6 | 119 | 16 | 7.99 | |
| 226.9 | 4.57 | 153 | 3.7 | ||||||
| Day 18 | 12/24/2021 | 159.2 | 3.53 | 147 | 3.6 | 113 | 14.8 | 5.24 | |
| Day 19 | 12/25/2021 | 126.5 | 3.26 | 139 | 3.6 | 104 | 15.7 | 4.12 | |
| Day 20 | 12/26/2021 | 166.3 | 4.56 | 138 | 3.9 | 105 | 20 | 5.55 | |
| Day 21 | 12/27/2021 | 129.9 | 3.97 | 137 | 4.1 | 105 | 19.3 | 4.72 | |
| Day 23 | 12/29/2021 | 131 | 4.18 | 140 | 4 | 105 | 18.1 | 5.07 | |
| Day 24 | 12/30/2021 | 190.1 | 6 | 137 | 4.1 | 105 | 18.3 | 7.95 | |
| Day 25 | 12/31/2021 | 115 | 4.11 | 139 | 3.2 | 104 | 20.9 | ||
| Day 26 | 1/1/2022 | ||||||||
| Day 27 | 1/2/2022 | 97.3 | 4.03 | 138 | 4.2 | 105 | 19.8 | 5.4 | |
| Day 28 | 1/3/2022 | 142.5 | 5.65 | 138 | 3.9 | 105 | 15 | 7.9 | |
| Day 30 | 1/5/2022 | 142.5 | 5.65 | 138 | 3.9 | 105 | 15 | 7.9 | |
| Day 31 | 1/6/2022 | 70.5 | 3.79 | 138 | 3.5 | 104 | 21.8 | 4.04 | |
| Day 32 | 1/7/2022 | ||||||||
| Day 34 | 1/9/2022 | ||||||||
| Day 35 | 1/10/2022 | 166.2 | 5.73 | 136 | 3.4 | 104 | 15.6 | 6.57 | |
| Day 37 | 1/12/2022 | 145.2 | 5.15 | 3.3 | |||||
| Day 42 | 1/17/2022 | 121.9 | 3.71 | 135 | 5.1 | 110 | 14.7 | 6.35 | |
| Day 45 | 1/20/2022 | 117.6 | 2.41 | 136 | 4.6 | 108 | 17.7 | 6.34 | |
| Day 47 | 1/22/2022 | 98.5 | 1.6 | 133 | 4.3 | 106 | 6.65 | ||
| Day 48 | 1/23/2022 | ||||||||
| Discharge | 1/24/2022 | ||||||||
| Date | Bilirubin-T | Bilirubin-D | Bilirubin-I | SGOT (AST) | SGPT | T.Protein | Albumin | Globulin | Sr.Al Phosphatase |
| 12/15/2021 | 2.9 | 2.02 | 0.88 | 48.4 | 22.6 | 5.34 | 2.7 | 2.64 | |
| 12/17/2021 | |||||||||
| 12/18/2021 | 5.22 | 3.92 | 1.3 | 118.9 | 37.8 | 5.73 | 3.07 | 2.66 | 40.9 |
| 12/25/2021 | 2.73 | 2.07 | 0.66 | 115 | 60.5 | 4.27 | 1.97 | 2.3 | |
| 1/6/2022 | 1.47 | 0.99 | 0.48 | 58.9 | 33.4 | 6.8 | 2.43 | 4.37 | 210.1 |
Clinical Data
| Chief Complaints | Sigmoid Diverticulitis with Post Hartmann’s Procedure and Pedunculated Polyp in Sigmoid Colon |
| Diagnosis | Sigmoid diverticulitis |
| History of past illness | HTN, stroke, CAD |
| Plan of treatment | Surgical management
Post hartmann’s surgery, laparotomy- anastomosis, relaparotomy, tracheostomy. |
| Clinical appearance | Eyes, hair, nails, skin, mouth, lips and extremities – normal |
| Personal diet history | Non – smoker, non-alcoholic, high consumption of bakery products |
| Diet habit
Food allergy |
Non – vegetarian
nil |
| Subjective global assessment | Well-nourished but at risk & well built |
PES STATEMENT
| Problem | Etiology | Symptoms | ||
| Inadequate fibre intake | Related to | High consumption of bakery products | As evidenced by | Patients diet history and diverticula found in colon |
| Altered biochemical parameters | Medical condition of the patient | Elevated renal parameters
( urea, creatinine, sodium) |
||
| Altered GI functions | diverticulitis | Abdominal pain& bloating |
Medical Nutrition Therapy:
- Energy: To provide adequate calories to maintain optimal body weight.
- Carbohydrate: To provide moderate carbohydrate to prevent protein catabolism.
- Protein: To provide high protein in order to aid in tissue repair and growth.
- Fat: To provide moderate fat to aid in optimal growth.
- Fibre: Limit the intake of fibre; fibre intake can be increased gradually to promote satiety.
- Fluids: To provide liberal fluids to maintain hydration status
- Probiotics: Adequate probiotics are effective in the management of this disorder
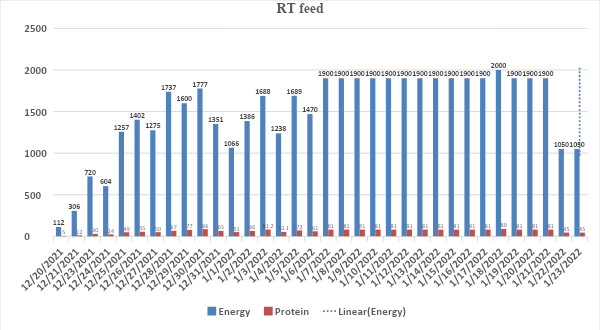
Nutrition Care Process
| DOA: 06-12-2021 @ 11.50 PM | |||||
| DAYS | DATE | TYPE OF DIET | ENERGY(kcal) | PROTEIN(g) | REMARKS |
| Day 2 | 12/7/2021 | NPO | 0 | 0 | Pre-operative |
| Day 3 | 12/8/2021 | NPO | 0 | 0 | Procedure done -Laprotomy colorectal; Anastomosis |
| Day 4 | 12/9/2021 | NPO | 0 | 0 | Post-operative (Day-1) |
| Day 5 | 12/10/2021 | NPO | 0 | 0 | Post-operative (Day-2) |
| Day 6 | 12/11/2021 | NPO | 0 | 0 | Post-operative (Day-3) |
| Day 7 | 12/12/2021 | Oral Clear liquid diet @ 30ml/hr | 120 | 8 | |
| Day 8 | 12/13/2021 | Oral Clear liquid diet | 150 | 9 | |
| Day 9 | 12/14/2021 | Oral Clear liquid diet | 150 | 9 | |
| Day 10 | 12/15/2021 | NPO | 0 | 0 | Procedure done-Relaprotomy |
| Day 11 | 12/16/2021 | NPO | 0 | 0 | Post-operative (Day-1) |
| Day 12 | 12/17/2021 | NPO | 0 | 0 | Post-operative (Day-2) |
| Day 13 | 12/18/2021 | NPO | 0 | 0 | Post operative (Day-3); Suggested TPN @ 50ml/day |
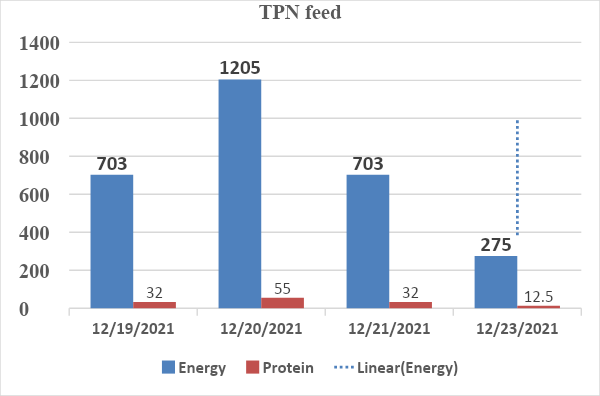
| Day 14 | 12/19/2021 | TPN @ 45ml/hr; Total volume: 630ml | 703 | 32 | TPN initiated |
| Day 15 | 12/20/2021 | TPN @ 45ml/hr ; Total volume:1080ml | 1205 | 55 | |
| RT feed @ 10ml/hr; Total volume: 110ml | 112 | 5 | RT feed initiated | ||
| TOTAL | 1317 | 60 | |||
| Day 16 | 12/21/2021 | TPN @ 45ml/hr; Total volume: 630ml | 703 | 32 | C/O RT Aspiration – 1000ml; Stopped TPN and RT feed |
| RT feed @ 20ml/hr; Total volume: 300ml | 306 | 12 | |||
| TOTAL | 1009 | 44 | |||
| Day 17 | 12/22/2021 | NPO due to RT aspiration | 0 | 0 | RT feed stopped – 250ml RT aspiration |
| Day 18 | 12/23/2021 | TPN @ 50ml/hr; Total volume: 250ml | 275 | 12.5 | TPN stopped and RTH initiated |
| RTH feed @ 30ml/hr; Total volume: 480ml | 720 | 30 | SLED x 6 hour | ||
| TOTAL | 995 | 42.5 | |||
| Day 19 | 12/24/2021 | NPO | 0 | 0 | Procedure done-Tracheostomy; SLED x 6 hour |
| RT feed @ 40ml/hr followed by 50ml/hr; Total volume: 710ml | 604 | 24 | RT feed initiated [4pm] | ||
| Day 20 | 12/25/2021 | RT feed @ 50ml/hr followed by 70ml/hr; Total volume: 1380ml | 1257 | 49 | |
| Day 21 | 12/26/2021 | RT feed @ 70ml/hr; Total volume: 1540ml | 1402 | 55 | Hemodialysis |
| Day 22 | 12/27/2021 | RT feed @ 70ml/hr; Total volume: 1400ml | 1275 | 50 | |
| Day 23 | 12/28/2021 | RT feed @ 70ml/hr followed by 100ml/hr; Total volume: 1670ml | 1737 | 67 | Hemodialysis |
| Day 24 | 12/29/2021 | RT feed @ 100ml/hr followed by 50ml/hr; Total volume: 1600ml | 1600 | 77 | |
| Day 25 | 12/30/2021 | RT feed @ 50ml/hr; Total volume: 1000ml | 1777 | 86 | Hemodialysis |
| Day 26 | 12/31/2021 | RT feed @ 50ml/hr; Total volume: 760ml | 1351 | 65 | |
| Day 27 | 1/1/2022 | RT feed @ 30ml/hr; Total volume: 600ml | 1066 | 51 | Hemodialysis |
| Day 28 | 1/2/2022 | RT feed @ 30ml/hr followed by 50ml/hr; Total volume: 780ml | 1386 | 66 | |
| Day 29 | 1/3/2022 | RT feed @ 50ml/hr; Total volume: 950ml | 1688 | 81.2 | Hemodialysis |
| Day 30 | 1/4/2022 | RT feed @ 50ml/hr followed by 70ml/hr; Total volume: 1100ml | 1238 | 53.1 | |
| Day 31 | 1/5/2022 | RT feed @ 70ml/hr followed by 100ml/2nd hrly ; Total volume:1200ml | 1689 | 72 | Shifted from ICU to 511 |
| Day 32 | 1/6/2022 | RT feed @ 100ml/2nd /hrly; Total volume: 700ml | 1470 | 61 | |
| Day 33 | 1/7/2022 | RT feed @ 100ml/2nd/ hrly; Total volume: 900ml | 1900 | 81 | Hemodialysis |
| Day 34 | 1/8/2022 | RT feed @ 120ml/2nd / hrly; Total volume: 1080ml | 1900 | 81 | |
| Day 35 | 1/9/2022 | RT feed @ 120ml/hr; Total volume: 1080ml + oral trials | 1900 | 81 | |
| Day 36 | 1/10/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral trial liquids | 1900 | 81 | Hemodialysis |
| Day 37 | 1/11/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral trial liquids | 1900 | 81 | Hemodialysis |
| Day 38 | 1/12/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral trial semi solids | 1900 | 81 | Hemodialysis |
| Day 39 | 1/13/2022 | RT feed @ 150ml/hr; Total volume: 1350ml+ oral trial semi solids | 1900 | 81 | |
| Day 40 | 1/14/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral trial semi solids | 1900 | 81 | Hemodialysis |
| Day 41 | 1/15/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral trial semi solids | 1900 | 81 | |
| Day 42 | 1/16/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral trial semi solids | 1900 | 81 | |
| Day 43 | 1/17/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral trial semi solids | 1900 | 81 | Hemodialysis |
| Day 44 | 1/18/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral semi solids | 2000 | 89 | Oral semi solids was improved |
| Day 45 | 1/19/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral semi solids | 1900 | 81 | Oral intake was fair |
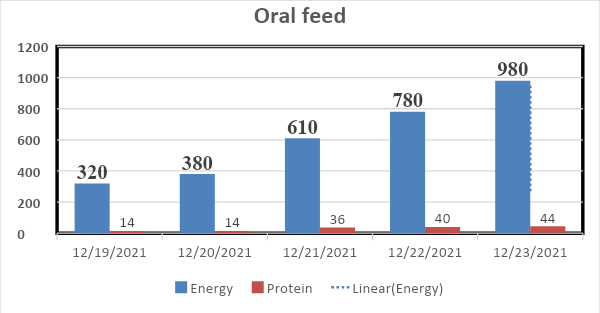
| Oral semi solids | 320 | 14 | Oral soft solid diet modified | ||
| TOTAL | 2220 | 95 | |||
| Day 46 | 1/20/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral soft solids | 1900 | 81 | Intake was improved |
| Oral soft solids | 380 | 14 | |||
| TOTAL | 2446 | 116 | |||
| Day 47 | 1/21/2022 | RT feed @ 150ml/hr; Total volume: 1350ml + oral soft solids | 1900 | 81 | Diet modifications done |
| Oral soft solids | 610 | 36 | |||
| TOTAL | 2510 | 117 | |||
| Day 48 | 1/22/2022 | RT feed @ 120ml/hr; Total volume: 750ml | 1050 | 45 | RT Feed modified to 5 feeds since intake was improved |
| Oral soft solids | 780 | 40 | |||
| TOTAL | 1830 | 85 | |||
| Day 49 | 1/23/2022 | RT feed @ 120ml/hr; Total volume: 750ml | 1050 | 45 | |
| Oral soft solids | 980 | 44 | ORAL INTAKE WAS GOOD | ||
| TOTAL | 2030 | 89 | |||
| discharge | 1/24/2022 | DISCHARGE ADVICE GIVEN ON RT FEEDS AND ORAL VITAMIN K RESTRICTED DIET | WEIGHT :77kgs | ||
Conclusion
A 62-year-old male with k/c/o sigmoid diverticulitis, post Hartmann’s procedure for sigmoid diverticulitis, pedunculated polyp in sigmoid colon with post polypectomy, had been admitted for tfurther management. The patient had past history of Hypertension, CAD, Stroke. Surgical management – colonoscopy was planned and the patient had undergone Laparotomy, Anastomosis, Relaparotomy and Tracheostomy. The patient also had abnormal renal parameters (insufficient renal function) and had undergone series of dialyses. During the hospital stay the nutritional management was planned according to the health condition of the patient. Total Parenteral Nutrition was provided for 4 days followed by Enteral Nutrition. At the beginning of EN (RT feed) semi elemental formula was prescribed since it is a peptide based and easily digestible; later the EN feed was modified to disease specific formula based on patient’s health and medical condition. As the patient’s condition improved oral semi solid diet was initiated along with RT feed until discharge. The patient’s discharge weight was 78.4kg. Two weeks soft solids along with oral nutritional supplement were given, and NG FEEDS stopped. Weight was monitored. High protein and vitamin K restricted diet was prescribed at the time of discharge as the patient is on acitrom medication.

