Open stab injury by a Bull
Poornima P1, Mercy Ezhil Rani*2
1Emergency care Technician, Kauvery Hospital, Hosur
2Clinical Educator, Kauvery Hospital, Hosur
Background
Bull gore injuries are not uncommon in regions where bulls are commonly used for agriculture or as part of sporting culture. Most bull gore injuries occur in the trunk and extremities. Cervical bull gore injury might be due to penetrating or blunt trauma. In the neck, it may injure vital structures such as the trachea, esophagus, and carotid artery. Traumatic cervical esophageal injury is a rare entity. Prompt diagnosis and early intervention are essential for better outcomes. Delayed diagnosis (>24 hr) is associated with a mortality of 40–66%.
History
A 70 years aged male was brought to the ER with an alleged history of having an injury inflicted below the Right ear, below the lobe, from a stab by a bull, around 10.00 am, on 04/08/2024
No known allergies, h/o hypertension, on anti-hypertensive drugs
On Examination (Systemic)
Airway – Patent
Breathing – Respiration Rate-30 b/m, SpO2-60% RA
Circulation – Pulse rate-130b/m, BP-Not recordable
Disability – GCS-E3-V1-M4 = 8/15, Pupils-B/L 2mm, both pupils are equally reacting to light.
Local Examination
- Stab injury in the right ,below auricular region, size 4x3x2 cm, with active bleeding.
- Right ear lobe 3cm wound was sutured outside
Investigation Study
- ABG – Metabolic acidosis
- PH – 7.28, HCO3 – 20.2 mmol/L, PCO2 – 43 mmHg, PO2 – 55 mmHg
Carotid Doppler
- Bilateral Common Carotid Artery (CCA) showed mild minimal thickening
- Both carotids showed normal flow with no demonstrable hemodynamic abnormality
- Both the vertebral arteries showed normal flow pattern with no demonstrable hemodynamic abnormality.
CT Chest
- Sub-segmental collapse noted in right lower lobe due to aspiration
- Focal fibrosis noted in right upper lobe.
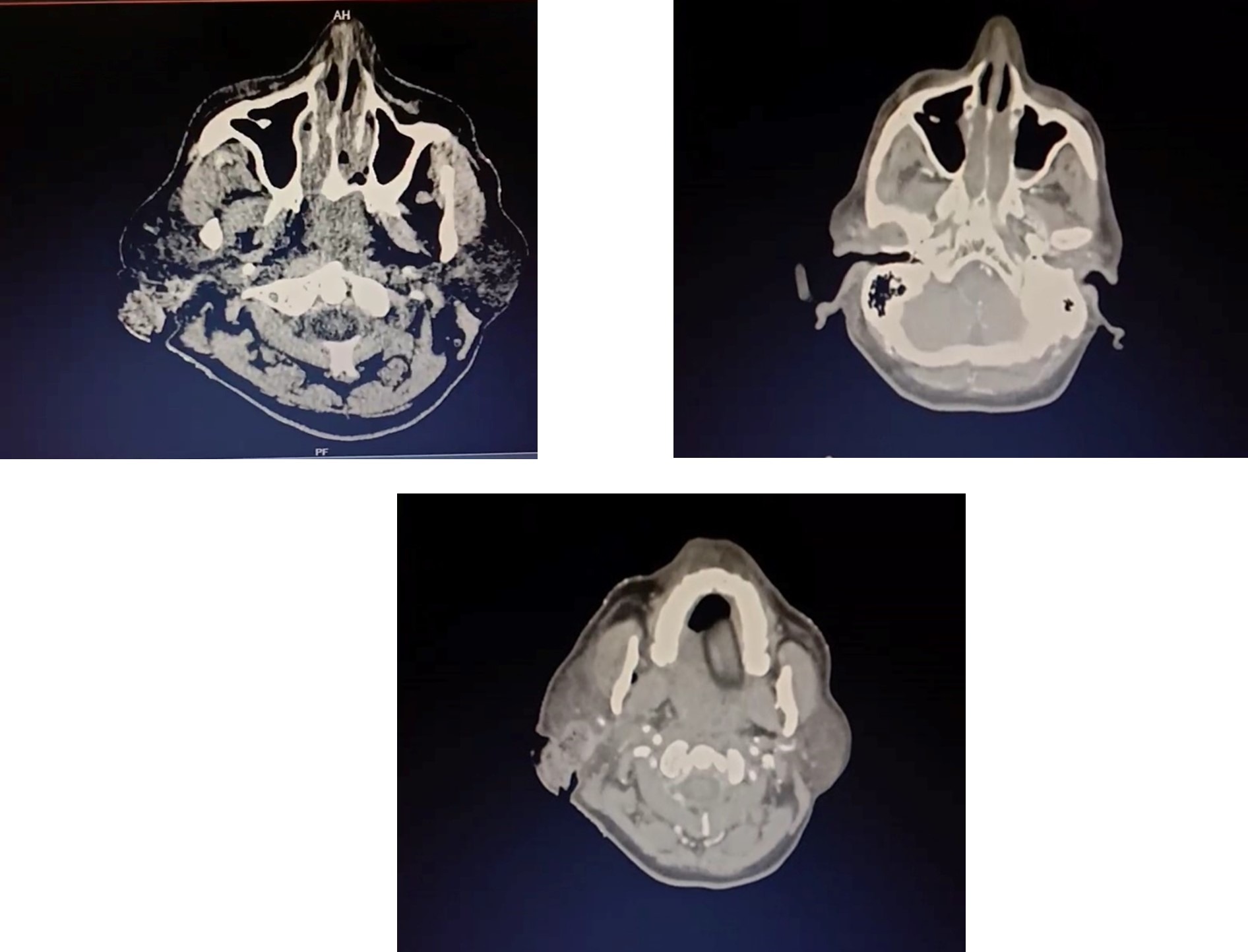
CECT Neck
- Edema noted in intramuscular plane in right parotid, right carotid, masticator space
- Focal non-visualization of right internal jugular vein – likely due to compression
CECT Whole Spine
- Multifocal anterior & posterior osteophyte changes noted in cervical vertebral
- No fractures noted.
CT Chest

CT – Neck
Chest X ray

Echo Cardiogram
- Poor ECHO window.
- No regional wall motion abnormality.
- Good LV EF – 60%.
- Grade 1 diastolic dysfunction.
Emergency Management
By intubating
On examination, patient suddenly went to bradycardia 30 b/m, followed by absent carotid pulse. CPR started as per protocols Inj. Atropine 0.6 mg and Inj. Adrenaline 1 mg IV stat given. Return of spontaneous circulation attained with 1 cycle of CPR.
Post Intubation Vital Signs
At 12.15 pm
- BP – 70/50mmhg with Inj. Noradrenalline 5ml/hr
- HR – 110 b/m,
- SpO2-99% on CMV with FIO2-100%
- Chest – B/L creps present.
Intravenous medications and colloids (Expovian and Haemaccel) bolus given. Patient was stabilized with inotropes and mechanical ventilation. CECT neck done, after that the vitals were,
- BP – 130/80 WITH Inj. Noradrenaline support
- SpO2 – 100% with 60% fio2.
At 5 pm
- Patient BP dropped again BP-80/60 with Inj. Noradrenaline support
- SpO2 – 100% with 60% fio2.
- Due to severe bleeding 1 unit of PRBC and 2 units of FFP were transfused, IV haemoccel 500ml bolus, IV normal saline 1000ml bolus given.
At 5.30 pm
- Patient had bradycardia followed by cardiac arrest, CPR initiated, ACLS protocol followed. After 1 cycle of CPR – return of spontaneous circulation attained.
- HR-110 b/m, SpO2–100% with FIO2-60%
- ABG taken, Inj.Bicarbonate correction given. Fluids given to treat hypovolemic shock.
- Pressure dressing done to control bleeding.
- Patient shifted to emergency OT after obtaining Neuro and Ortho opinion. Wound debridement and suturing done under general anesthesia.
Operative Notes
Open wound examined, parotid gland found in two halves, facial artery and retro-mandibular vein severed.
- Artery and vein ligated
- Facial nerve status not assessed
- Adequate homeostasis achieved
- Drain in situ
- Closure done.
Intra operative blood loss less than 500ml
Intra operative 1 unit PRBC and 2 units FFP transfused
Patient shifted to ICU with a ventilator support.
Diagnosis
- Assault, open stab injury by a bull
- Right auricular injury with lacerated wound in the neck
- Hypovolemic shock
- Hypotension
- Post cardiac arrest (2 cycle of CPR)
Intensive Care Unit
Day-1
- Patient on MV. GCS – E4VTM6
- Periodic monitoring of CBC, RFT, ABG, serum electrolytes and monitoring BP.
- 3 Pint PRBC,4 pint FFP administered
- Ionotropic infusion continuously monitored
- Metabolic acidosis correction given accordingly. patient on sedation.
- Dressing on the surgical site. CVP monitoring continued.
- Continuous RT aspiration.
Day-2
- On sedation, propped up position
- Patient stable, no bleeding noted on both intra oral and extra oral cavity.
- Throat pack removed
- Inotropes, NaHco3, Fentanyl infusions on flow. RT feed 200ml/hour
- No oozing on the surgical site.
- DVT stocking applied to prevent Deep Vein Thrombosis.
Day-3
- Patient was arousable, and obeying commands
- Plan for bronchoscopy (Pulmonologist opinion) on examination of respiratory system-there was decreased air entry over left side.
- Under aseptic precautions, Bronchoscopy done and left side mucus plug removed.
- Intravenous medications continued
- Chest physiotherapy given,1 pint PRBC, 1 pint FFP transfused
- ET care followed
- RT feed administration
- Nephrologist opinion sought for AKI, advised for renal protective diuretics
- Ortho opinion sought, advised nil interventions.
Day-4
- T-Piece trial given, Patient tolerated well.
- Patient was extubated and connected to NIV support
Post Extubation
BP – 130/70mmhg
HR- 63 b/m
SPO2 – 99%, FIO2-50% with NIV support PEEP – 5.
- BAL culture showed B/L Klebsiclla Pneumonia
- IV antibiotics continued.
- Encourage oral feeds and Spirometry.
- Patient on propped up position.
Day-5
- Patient on propped up position.
- Intake and output monitoring
- Encouraged, oral soft diet/chest physiotherapy
- Spirometry given, ambulation initiated.
- O2 support /NIV support (sos)
- IV medication continued
- Central line cannulation removed.
Day-6
- Patient stable with O2 on nasal prongs.
- Oral feeds tolerated well.
- IV medications antibiotics,fluids continued
- Shifted to ward.
Ward
- Chest physio, Active movement encouraged.
- Breathing exercise given.
- Intensive spirometry given.
- Mobilization done with support.
- Then, patient had intermittent episodes of productive cough, managed with broncho dilators.
- Diuretics and other supportive measures.
- With regular exercise, saturation improved but not maintaining in room air.
- Hence advised for Long Term Oxygen Therapy (LTOT) at home.
- Patient symptomatically better, hence discharge with LTOT.
Condition on Discharge
Patient conscious, oriented, afebrile, tolerated oral feed.
Vital stable
BP – 150/80mmHg,
PR – 78 b/m,
SPO2 – 92 % LTOT
Health Education
- Explained discharge advice medications and follow up
- Education on wound care
- Educated about diet plan
- Monitoring of SPo2
- Handling of LTOT equipment
- Emergency reporting regarding breathing difficult, desaturation
- ROM exercise
- Spirometry
- Chest physiotherapy

