S. Kanimozhi
Nurse Educator, Department of Nursing, Kauvery Hospital, Hosur.
Quality improvement project to reduce the incidence of ventilator-associated pneumonia
Background
During the month of March-May, 2021, we observed that persistently one or other attendee in Intensive Care Unit expressed dissatisfaction regarding patient’s prolonged stay in ICU due to setbacks in the patient’s health condition. ICU team were overwhelmed by the negative responses and work-related stress.
Hence, 360° audit was done. The results indicated many non-compliances in ICU related to hospital protocols.
The project was done in the month of June 2021. Brainstorming was done, keeping the data dank and the existing problems in ICU were listed out. Amongst all the problems identified, incidence of “Increasing Ventilator-Associated Pneumonia” was selected as the most crucial problem to be addressed based on Ranking Method.
Problem Definition
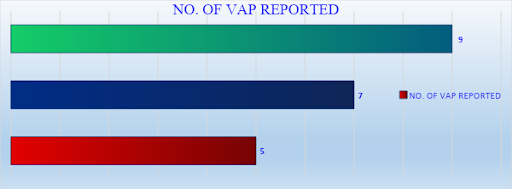
Five cases were reported in the month of March, 7 cases were reported in the month of April and 9 cases were reported in the month of May.
IMPACT OF VAP
The mortality rate of VAP ranges from 25-50%, depending on the individual’s comorbidities and the pathogens involved.
VAP increases ICU length of stay up to 6.1 days and hospital length of stay up to 10.5 days. (Average length of stay in ICU: 3.3 days; Hospital: 4.5 days)
Each VAP adds to an estimated cost of around Rs. 3 lakhs to the patient bill.
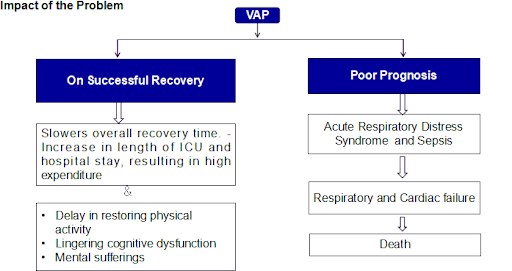
Impact on the Institution
Patients and attenders will lose confidence over the treatment provided in the institute. Further, they may not visit again and also will not refer their colleagues/relatives to our institution.
The top management may not have a good impression about the ICU Team.
May affect our organisation’s brand image.
May affect the target of quality indicators.
May fail to achieve our business objectives.
Process Sequence
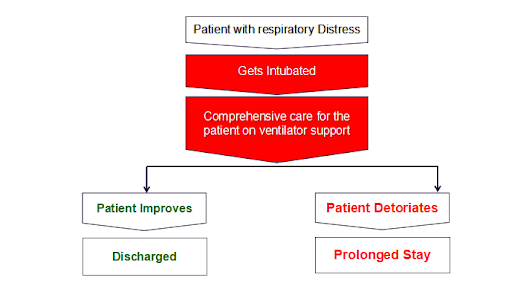
Process sequence was listed and found that the problem occurs in the stage of intubation and care.
Problem analysis was done in the month of July 2021 and found that on an average 16% of the patients were affected with VAP.
| PARTICULARS | MARCH | APRIL | MAY | JUNE | JULY |
| No. of patients on ventilator support | 48 | 42 | 60 | 52 | 38 |
| No. of VAP reported | 5 | 7 | 9 | 8 | 6 |
Goal was set to reduce the incidence of VAP from 16% to Nil.
Probable causes were listed down and depicted in Ishikawa Diagram under the header Man, Material, Method and Machine.
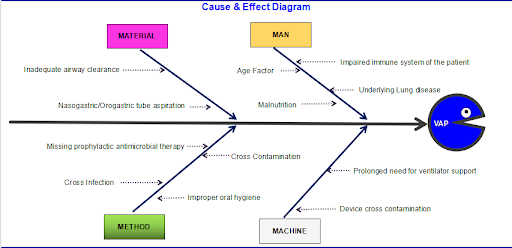
Validation was done for all the probable causes and significant causes were identified through verification. 4 significant causes were found out.
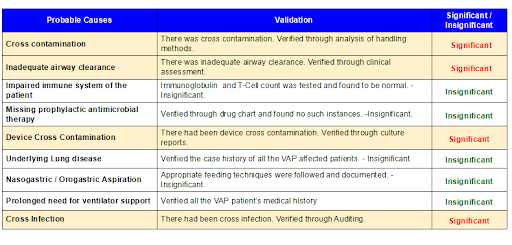
How analysis was done for all the 4 valid causes and root cause was identified.
Usage of open method of suctioning – 1st root cause
Using normal cuffed ET tube without subglottic suction – 2nd root cause
Using vaccum jars and oxygen humidifiers after disinfecting only with hot water – 3rd root cause
HIC practice non-compliances- 4th root cause
Data analysis was done in the month of September for each of the valid causes and solutions were developed.
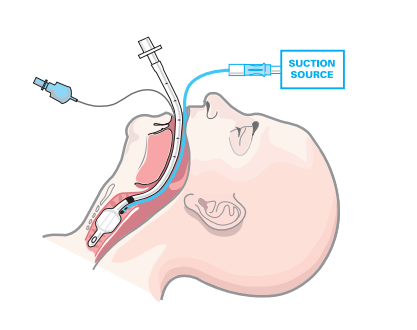
Data Analysis – 1: A single-use catheter is inserted into the Endotracheal tube by disconnecting the ventilator tubing for suctioning. Frequent open suctioning introduces microbes from the external environment into the airway.
Solution 1
Using closed suction system. Closed suction system minimizes respiratory pollution, which reduces pulmonary infections.


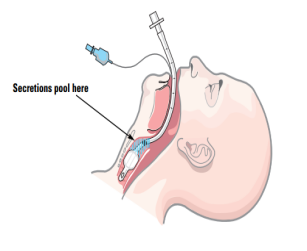
Data Analysis – 2: The endotracheal tube prevents glottic closure. As a result, the patient is unable to cough and remove secretions in a natural way. Hence, accumulation or pooling of oropharyngeal secretions above the endotracheal tube cuff occurs and it facilitates colonization of bacteria posing risk of VAP.
Solution 2
Using ET tube with subglottic suctioning. subglottic suctioning removes secretions from above the cuff of the endotracheal tube and thus prevents pooling of secretions.
Data Analysis – 3: Culture samples were sent from oxygen humidifiers and vaccum jars that were washed with hot water. Reports showed Growth of Microbes.
Solution 3
Using vaccum jars and oxygen humidifiers after ETO method of disinfection. ETO method of disinfection has higher efficiency and it destroys microorganisms, including resistant spores.


Data Analysis – 4: Hand Hygiene non compliances were found from hand hygiene audit – Percentage of adherence – 60%. The patients who are infected and those who are not infected are kept in the same cabin, without cohorting. This lead to cross-infection.
Solution 4
Strengthening hand hygiene practices through regular audits & strict isolation of infective cases.


Dedicated training sessions were conducted on the proposed solutions, One Point Lesson on hand washing steps, moments and isolation criteria were displayed. Possible points of resistance were discussed and solutions to overcome the resistances were developed. Glow Gel Solution and UV – Torch Audit Methodology was followed to ensure maximum adherence of hand hygiene. Further, Announcement Audio played once in an hour to remind staff to wash hands. Trial implementation was done in the month of October 2021.
Changes were perceived post-trial (VAP Incidence in the month of October – 1) and hence, regular implementation was done in the month of November 2021 and the incidence of VAP was found to be reduced to Nil.
Standardization
A need-based checklist was created and SOP was updated based on the implemented solutions after obtaining approval from Deputy Medical Administratoror
Outcome
The incidence of VAP remained at 0% on follow-up and review which was in the month of December 2021.
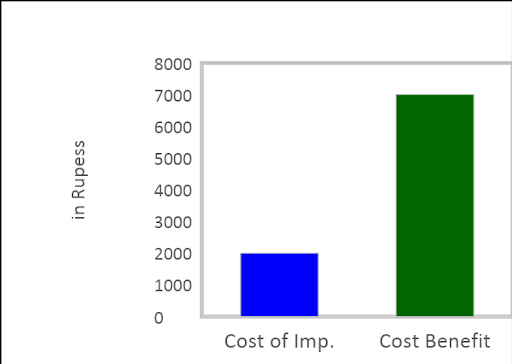
Tangible Benefits
For the Institution:
| COST OF IMPLEMENTATION | BENEFIT |
| ETO Charges – Nil
Alloting HDU unit for infected cases – Nil |
Due to prolonged stay of infected patients, ICU census increases.
Staffs do double duty. Costs around Rs.1000(Approx) -Per staff/day |
| Hand Hygiene Moment Chart – Rs.1000 (Approx) | Increase in Referrals from the patients.
1 OP Referral Patient – Rs.500 (Approx) 1 IP Referral Patient – Rs.5,000 (Approx) |
| VAP Bundle Checklist (1000 sheets) – Rs.1000/- | Chances of patient’s revisit increases,
due to satisfaction. 1 OP Revisit – Rs.500 (Approx) |
| Total Cost of Updation : Rs.2,000/- | Total Earnings : Rs.7000/-(Approx Per Patient/Day) |
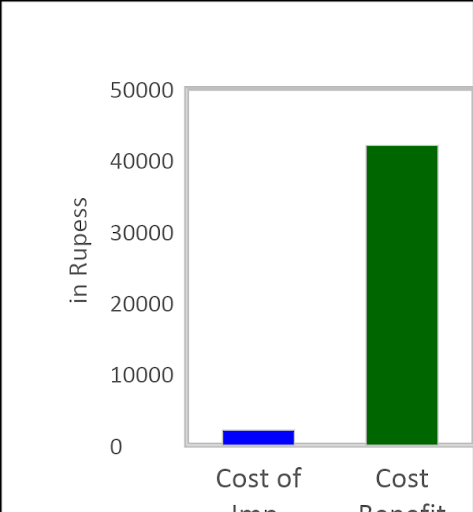
For the Patient:
| COST OF UPDATION | BENEFIT |
| ET tube without sub glottic suction vs ET tube with sub glottic suction – Rs. 600 extra | Reduces Stay in ICU.
1 day stay in ICU – Rs. 35,000 (Approx) |
| Open vs Closed Suction Catheter – Rs. 1000/- extra | Reduces cost of Antibiotics.
3 dose costs – Rs. 2000 (Approx) |
| PPE Cost – Rs. 500/- (Approx) | Reduces over all stay in the hospital.
1 day stay in Ward – Rs. 5000 (Approx) |
| Investment Cost of the Project: Rs.2,100/- (Approx.) | Overall Savings: Rs. 42,000/- (Approx./day) |
Intangible Benefits
For the Patient:
- Speedy recovery
- Psychological well being
For the Institution:
- Improved quality of care
- Good brand image
- Quality Indicators within bench mark
- Increased customer satisfaction
For the Staff
- Stress free work place
- Increases confidence
- Team gains good impression from the top management
Recognition for the Project:
- Won State Level CII – QC Competition;
- Selected among Top 10 in Regional Level CII – QC Competition and got entry into National Level Competition.
Discussion
VAP is a preventable Hospital Acquired Infection, provided the care given and precaution taken are appropriate.

