Rapid Review of CNE – Enhancing Nursing Practice in Arrhythmia Management: Evidence Based Strategies
Esthar Rani S1, Revathy2
1Nursing Superintendent, Kauvery Heartcity, Trichy, India
2Emergency Ward Nursing Incharge, Kauvery Heartcity, Trichy, India
Background
Understanding cardiac arrhythmias and the interventions to achieve their abolition, control and prevention
The CNE program discussed recognition of cardiac arrhythmias , some anatomical aspects relevant to the understanding of causation of arrhythmias, general mechanisms of arrhythmias, mechanisms of some specific arrhythmias and non-pharmacological forms of therapy.
History of Arrhythmia
Following the construction of the string galvanometer by Einthoven in 1901, which allowed high-fidelity recording of the body surface electrocardiogram, the study of arrhythmias developed in an explosive way. Papers from McWilliam (1887), Garrey (1914) and Mines (1913, 1914), in which neither mechanical nor electrical activity was recorded , provided crucial insights into re-entry as a mechanism for atrial and ventricular fibrillation, atrioventricular nodal re-entry and atrioventricular re-entrant tachycardia in hearts with an accessory atrioventricular connection. For many decades, mapping of the spread of activation during an arrhythmia was performed with a “roving” electrode that was subsequently placed on different sites on the cardiac surface with a simultaneous recording of another signal as time reference. This method could only provide reliable information if the arrhythmia was strictly regular. When multiplexing systems became available in the late 1970s, and optical mapping in the 1980s, simultaneous registrations could be made from many sites. The analysis of atrial and ventricular fibrillation then became much more precise. Successful surgery in the 1980s, the development of external and implantable defibrillators in the 1960s and 1980s, and finally catheter ablation at the end of the previous century, with success rates that approach 99% for supraventricular tachycardia.
Arrhythmia and the related interventions:
1. Understanding Electrocardiography fundamentals and interpretation:
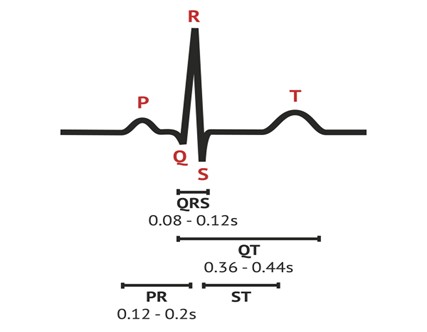
ECG Paper Grid
- One small box = 0.04 seconds
- One large box = 0.2 seconds
- 5 large boxes = 1 second
Measuring Heart Rate
- Method 1: Count the number of R-R intervals in 6 seconds, then multiply by 10.
- Method 2: Count the number of large squares between two consecutive R-waves and divide by 300.
2. The science behind Arrhythmias: pathophysiology and etiology

Arrhythmias can significantly affect cardiovascular health, ranging from benign to life-threatening conditions. Early recognition of signs, understanding pathophysiology, and identifying underlying causes are crucial for effective management and prevention. Healthcare professionals, especially nurses, play a vital role in continuous monitoring and educating patients about arrhythmia to improve outcomes and reduce complications.

3. Arrhythmia identification and differentiation
Irregular heart rhythms, either in rate (fast or slow) or in rhythm (irregular beats).

Early identification of arrhythmias is crucial for appropriate treatment. ECG interpretation is vital for distinguishing between different arrhythmias. Effective management can prevent complications such as stroke, sudden death, and heart failure.
4. Pharmacological management of Arrhythmias
Antiarrhythmic drugs are often classified according to the Vaughan-Williams system:

- Class I – sodium (Na+) channel blockers.
- Class II – beta blockers.
- Class III – potassium (K+) channel blockers.
- Class IV – calcium channel blockers.
- Class V – Other agents.
5. Non Pharmacological management of Arrhythmias:
Techniques and interventions used to manage arrhythmias without relying on medications. Some arrhythmias are difficult to control with drugs, while others may require non-invasive or surgical intervention to prevent complications like stroke or heart failure.

Source of the devices used
- Electrophysiological Study + RFA Cardiac frequency ablation
- Implantable Cardioverter – Defibrillators
- Cardiac Resynchronization Therapy
- Single chamber pacemaker
- Double Chamber Pacemaker
- Biventricular Pacemaker
6. Pediatric Arrhythmias: Diagnosis and management in children
Many pediatric arrhythmias are associated with congenital heart conditions such as atrial or ventricular septal defects or hypertrophic cardiomyopathy.

7. Nursing Care of patient with Arrhythmia in various scenario – Non-critical area, Critical area:
Nursing care for patients with arrhythmia varies significantly depending on whether the patient is in Non-Critical Areas – e.g: General Ward OPD. Critical Areas – e.g: CCU and Emergency Dept., The approach is based on the severity of the arrhythmia, the patient’s hemodynamic stability and the risk of complication.
- Atrial Fibrillation
- Atrial flutter
- Atrial tachycardia
- Bradycardia
- Tachy brady syndrome
- Sick sinus syndrome
- Heart Block
Atrial Fibrillation

Atrial flutter

Atrial tachycardia

Bradycardia

Tachy Brady Syndrome
Sick Sinus Syndrome:

Heart Block

Supraventricular Tachycardia

Ventricular Tachycardia

8. Hands on training – accurately interpret basic and advance ECG rhythms:
The three main types of electrocardiograms (ECGs) are resting, stress, and ambulatory.
Resting ECG
- You lie down and breathe normally while the ECG is recorded
- This type of ECG usually takes a few minutes
Stress or exercise ECG
- You exercise on a treadmill or stationary exercise bike while the ECG is recorded
- This type of ECG shows how your heart handles stress
Ambulatory ECG
- You wear a portable recording device for at least 24 hours
- This type of ECG is also called a Holter monitor an ECG can help diagnose conditions such as:
- Arrhythmia (abnormal heart rhythm)
- Poor blood flow to the heart muscle (ischemia)
- Heart valve issues
- Congenital heart disease
- Heart attack
- Enlarged heart chambers
- Heart damage or heart failure
9. Hands on training – ECG strip analysis in various clinical area
Rate
· Tachycardia or bradycardia?
- Normal rate is 60-100/min.
Pattern of QRS complexes
· Regular or irregular?
- If irregular is it regularly irregular or irregularly irregular?
QRS morphology
- Narrow complex: sinus, atrial or junctional origin.
- Wide complex: ventricular origin, or supraventricular with aberrant conduction.
P waves
- Absent: sinus arrest, atrial fibrillation
- Present: morphology and PR interval may suggest sinus, atrial, junctional or even retrograde from the ventricles.
Relationship between P waves and QRS complexes
AV association (may be difficult to distinguish from isorhythmic dissociation)
- Complete: atrial and ventricular activity is always independent.
- Incomplete:intermittent capture.
Onset and termination
- Abrupt: suggests re-entrant process.
- Gradual: suggests increased automaticity.
Response to vagal maneuvers
- Sinus tachycardia, ectopic atrial tachydysrhythmia: gradual slowing during the vagal maneuvers, but resumes on cessation.
- AVNRTor AVRT: Abrupt termination or no response.
- Atrial fibrillationand atrial flutter: Gradual slowing during the maneuver.
- VT: No response.
10. Hands on training – With device programming and troubleshooting:
Cardiac implantable electronic devices, including
- Pacemakers
- Implantable cardioverter defibrillator (ICD)
- Biventricular pacemakers
- Cardiac loop recorders,
are designed to help control or monitor irregular heartbeats in people with certain heart rhythm disorders and heart failure.

| Last Year Procedure Report - 2024 | ||
|---|---|---|
| S N | Procedure | Qnt |
| 1 | Total no of EP Study | 131 |
| 2 | Total no of RFA | 121 |
| 3 | Total no of SVT | 121 |
| 4 | Total no of AVRT | 27 |
| 5 | Total no of Heart Block | 103 |
| 6 | Total no of PPI | 101 |
Conclusion
One of the best skills is learning. I hope this succinct overview of the programme helps you think better. Understanding cardiac science is quite broad. I hope you now have a basic understanding of Management of Arrhythmias. To maintain the rhythm of the heart.
Here is the glimpse of the program:



