Rare disease, desired outcome
Leema Rebakkal Rosy1,*, Prabhavathi2
1Assistant Nursing Superintendent, Kauvery Hospital, Tennur, India
2Senior staff Nurse, Kauvery Hospital, Tennur, India
Background
Nurses require excellent observational and assessment skills. Being knowledgeable about common diseases that often affect the population is essential; however, it is often more challenging to be informed about life-threatening conditions that rarely develop. Such is the case with mesenteric ischemia, a rare but complicated condition, which is difficult to diagnose, carries a degree of mortality of about 40-70%, and is more common in people older than 50 years. Mesenteric ischemia requires that nurses be aware of the different etiologies and presentations of this uncommon disease to alert physicians of changes in a patient’s condition and detect clues that may assist with an accurate and prompt diagnosis.
The main blood supply for the gastrointestinal system is the superior mesenteric artery (SMA), celiac artery or trunk (CA), and inferior mesenteric artery (IMA). These three together are called the mesenteric arteries. Ischemia occurs when blood cannot flow freely through these arteries to its target organs, the intestines and mesentery, resulting in compromised oxygen delivery. Predominate damage occurs to the small intestine, but the large intestine and stomach can also be affected. In addition, the ischemia produces severe abdominal pain, which is usually out of proportion to the physical findings; this is a main feature of the disease. Being educated about the diagnostic procedures, possible outcomes, and anticipated care and needs of patients affected by this medical complication is imperative to maintain the health status and well-being of these patients and their families
Case Presentation
A 46-years old man came with complaints of abdominal pain/distension on and off for 10 days, with increased severity since the previous day. There was the history of vomiting episodes, and of not having passed stool for 3 days. The patient was known to have diabetes mellitus, and to be habituated to smoking and alcohol.
An immediate assessment was done. A general clinical examination of the abdomen revealed distension, guarding and rigidity. He had no pallor, pedal edema or supraclavicular lymph node enlargement.
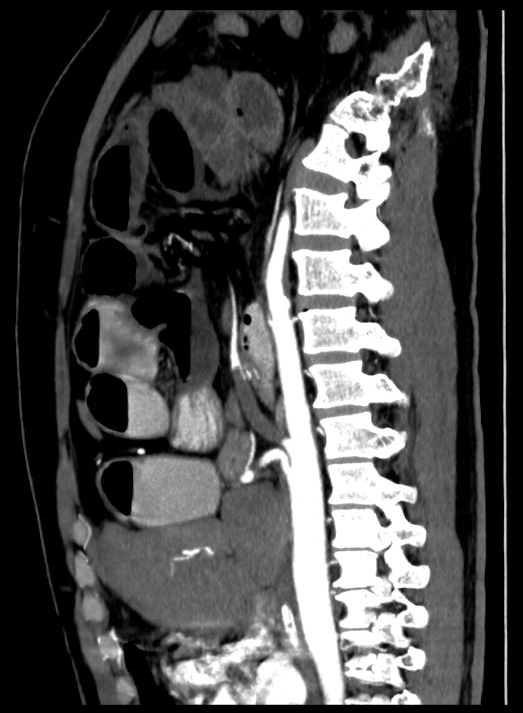
His CECT revealed :
1. Complete thrombotic occlusion proximal segment of SMA and dilated jejunal and ileal loops, with pneumatosis intestinal.
2. Signs of mesenteric ischemia with bowel infarction.
3. Minimal ascites, partial mural thrombosis infrarenal abdominal aorta.
4. Fatty liver changes
So, emergency surgery planned and discussed with team (general gastro surgeon and vascular surgeon, anesthetist). The patient underwent surgery on the same day of admission with high risk


Discussion prior to the surgery
Mesenteric ischemia is a rare condition with a high mortality rate. Survivors may need anticoagulants for life. This can complicate care or cause other comorbidities such as intestinal bleeding and anemia. Patients generally require multiple surgical procedures or procedures that increase the risk for bowel obstruction, other coagulopathy problems, persistent pain, or placement of a permanent colostomy, all of which can affect body image, self-esteem, desire to socialize, and overall quality of life. Management includes early mobilization. diet, and pain control. These interventions are meant to accelerate recovery and reduce the incidence of postoperative complications. In addition, the increased use of laparoscopic surgery as further decreased the length of hospital stay, blood loss, and medical expenses by being less invasive and thus accelerating the recovery process. This, needless to say, increases patient and family satisfaction. Our nurses, together with surgeons and anesthesiologists, play a vital part in implementing these clinical strategies pre-operatively, intraoperatively, and postoperatively.
Our patient underwent open surgery
Medical management
He started empirical antibiotics, PPI and other supportive measures.
Surgical management
After preoperative counselling and informed consent, he was operated under general Anesthesia
Emergency Laparotomy, Small Bowel Resection + SMA Thrombectomy + Vein Patch Closure done on 09.09.2022
Operative findings:
About 25 cm of ileum, ileo-caecal junction, caecum and proximal ascending colon was gangrenous. Another 10 cm of distal jejunum was also gangrenous. Rest of bowel (jejunum) 160 cm viable but partially ischemic. Purulent peritonitis.
Vascular Team:
SMA and branch isolated and looped
4000 units IV Heparin
Longitudinal arteriotomy – Fofartination – 4Fr / 3Fr
Proximal – Clot retrieved – Good forward bleed
Distal – Clot retrieved – Poor back bleed
Arteriotomy closed with vein patch
Posterior reperfusion – Bowel turned pink from cyanotic color
8ml (Heparin) + 32ml NS – 40ml at 1ml/ hr (1000 units / hr).
2. Re-Exploration, Jejunostomy with Mucus Fistula done on 12.09.2022
Previous incision opened
SMA pulse felt
Proximal jejunal segment (80cm) viable and healthy. In the isolated distal jejunal segment, about 15cm of distal most port ischemic and this was resected. As it would be high risk anastomosis and not safe, jejunostomy and mucus fistula planned. Colon viable. The proximal jejunal segment (80cm from DJ flexure) end brought out as stoma in RIF. The remaining isolated distal jejunal request (about 60cm), the proximal end of skin closed. Distal end of this brought as mucus fistula in lower end of wound. Saline lavage. DT kept. No-1 loop Ethilon closure. Skin – clips and Ethilon. Stoma constructed with 3-0 Vicryl.
Postoperative Discussion
The postoperative care is very important to ensure optimal recovery for our patient. Skilled and careful assessment is needed to prevent complications and restore the patient back to health. Post-surgery strategies include the removal of the nasogastric tube and indwelling urinary catheter as early as possible. We encourage clear liquid nutrition on the first operative day and, if the patient tolerates, advance to solid food the next day. We are also responsible for early mobilization of the patient, which can include getting out of bed and ambulating for short periods of time to prevent ileus, respiratory problems, and promote diet intake, digestion, and return of bowel function. Laxatives, antiemetics, and deep vein thrombosis prophylaxis are also implemented the same day as surgery. Nonsteroidal anti-inflammatory medications are important adjuncts to minimize the use of opioids in the immediate postoperative phase and thus decrease the potential for ileus and other complications.
Immediate Post-Op Day Management
When we are receiving the patient from OT to ICU with ventilator support and multiple infusion we had challenges in managing the patient in dynamic monitoring of abdominal symptoms and signs, anticoagulant therapy to prevent postoperative thrombosis, prevention and care of complications, providing nutritional support to promote recovery, mobilizing limbs and in providing rehabilitation exercise guidance.
Intra-operatively, during procedure, our patient had hypotension and atrial fibrillation for which we started multiple infusions like inotropes (Inj. Nor adrenaline infusion) anti arrthymic drugs (Inj. Amiodorone infusion), hypoglycemic drugs (insulin infusion) and anti-coagulants (Inj. Heparin infusion).
Our team had a discussion about the frequent of assessment of the patient, anticipation of complications and about the proactive management.
We had some difficulty in managing our patient with multiple tubes and invasive line for 24 h, but we managed without any complication.
Since the patient undergone SMA thrombectomy procedure the administration of the anticoagulant drug was very crucial on immediate post op day period to prevent any clot formation and occlusion. So, during Inj. Heparin infusion we did 6th hourly APTT, ratio checked and based on the ratio we adjusted the heparin infusion flow rate.
He had hyperpyrexia, for which we gave tepid sponging frequently and administered antipyretics and antibiotics as per the advice
Since the blood glucose was high started insulin infusion, monitored glucose level and avoided hypoglycemic events
To correct the dehydration and to improve the perfusion we transfused iv fluids and blood components based on the urine output and avoided fluid overload. We did hemodynamic monitoring non-invasively; we monitored the patient’s BP, pulse rate, rhythm, skin temperature, skin color, capillary refill time, oxygen saturation, urine output etc. Invasively we monitored cardiac output, tissue perfusion and ABG analysis by means of an arterial catheter. ABG gave a clear picture on response to the treatment such as drugs and ventilator support. We managed proactively to assure a good outcome.
Later he was weaned from ventilator, extubated, early ambulation begun and shifted to ward
Diet: High protein diet, as TPN transfusion, was started; later switched to oral diet, of liquids and high protein of supplementary feed.
Psychological and Emotional Support
His relatives were very anxious, making decision marking very difficult on daily treatment. Our team gave emotional and psychological support to the patient and family members. We provided the best communication and coordination with other team members, so that the patient’s health improved and attained the best possible outcome.
Stoma Care
Ostomy pouch was applied over the stoma. Stool from an ileostomy was expressed continuously or irregularly, and is liquid in nature; continuous use of a pouch to collect the drainage was therefore necessary. He was assessed frequently for bleeding, stoma viability, and function. In the early postoperative period, small amounts of blood in the pouch were expected. A healthy stoma appears pink or red and moist as a result of mucus production. The frequent assessment was done, particularly in the initial postoperative period to ensure stoma health and monitor for possible complications. As the stoma started to function, the pouch was emptied. Initial drainage was dark green, viscid, and odourless. Drainage gradually thickens and becomes yellow-brown. The pouch is emptied when it is one-third is full. Drainage is measured and included as an output on intake and output records. The pouch was rinsed and the clamp was reapplied. The peristomal skin was assessed. The skin around the stoma should remain clean and pink and free of irritation, rashes, inflammation, or excoriation. Any abnormal assessment findings were reported to the consultant.
Preventive aspects of care
The patient received the best example of evidence-based practices for best nursing care.
To prevent HAI in spite of all invasive lines, bundle care practices were strictly adhered to and achieved the best outcome of No CLABSI, No CAUTI, No pressure injury throughout the hospital stay also no NOSOCOMIAL infections. Our team had done risk assessment in each shift and planned and implemented all preventive measure against FALL, DVT, Delining of tubes and pressure injury Our nurses adhered to the Antibiotic Policy.
We adhered to FASTHUGSBID in critical care units and in wards for the preventive aspects of care. F-Feeding/Fluids, A-Analgesia, S-Sedation, T-Thromboprophylaxis, H- Headup position, U- Ulcer prophylaxis, G-Glycemic control, S-Spontaneous breathing trial, B- Bowel Care, I-Indwelling catheter removal, D-Drug de-escalation.
Based on the patient í¢€Ëœs condition we set the clinical alarm in multi para monitor and, if the alarm indicated any deviation in vital parameters, we immediately responded to the alarm, did reassessment and proactively managed and prevented major complications.
Conclusion
His further post operative period was uneventful. He was discharged on 22.09.2022. At the time of discharge, his wound was healthy and was tolerating normal diet.
Mesenteric ischemia can be a devastating disease that carries a high risk of mortality if it is not diagnosed early and reversed in a timely manner. Being knowledgeable of this rare disease presentation, its complications, possible etiologies, diagnostic measures and desired outcomes allows nurses to detect, contribute, and collaborate with the medical team to attain the best physical and psycho social outcomes for patients.

