M. Vignesh
Physiotherapist, Kauvery Hospital, Salem, India
Abstract
Guillain- Barre syndrome is an acute polyneuropathy characterized by acute flaccid paralysis with or without sensory/ autonomous nerve dysfunction. Normally, your immune system only fights foreign invaders such as viruses or bacteria. The word auto means self, so autoimmune refers to a disorder in which your immune system attacks your own body.
Background
GBS is considered the most disabling neurological condition next to poliomyelitis. It affects 1 to 2 in 100000 per year. It can attack at any age, the most common age group is 30-50 years. The mortality is about 8 to 12%. The disability may persist after the treatment especially with ambulation.
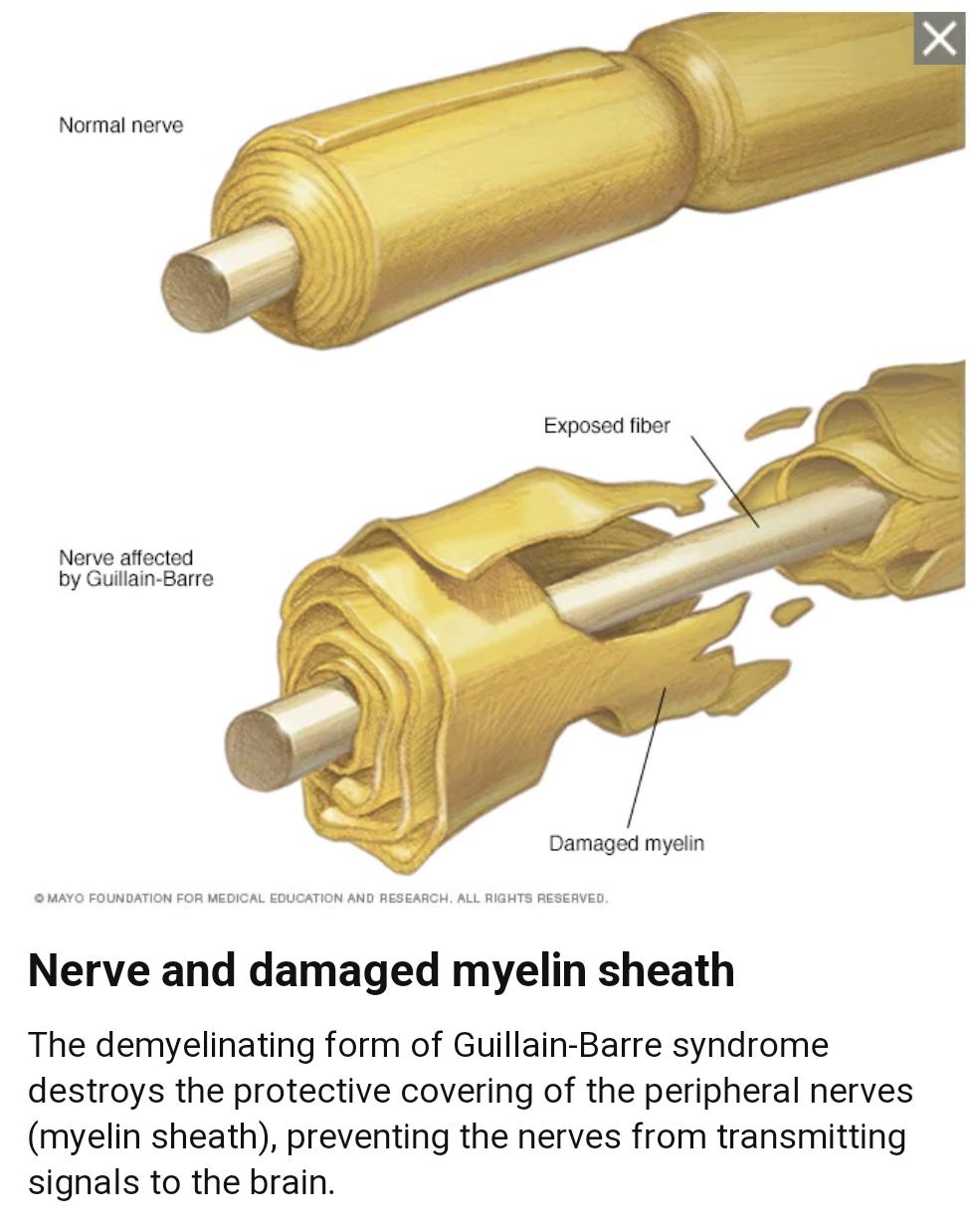
GBS is an autoimmune disorder in our own immune system that specifically attacks the nerves. You can think of a nerve as being similar to a wire that allows you to control your muscles and also feel what is happening in your environment. When this wire is damaged (as it is in GBS), your body loses the ability to control the muscles and sense the environment, leading to symptoms such as muscle weakness and numbness or tingling. These sensations can quickly spread, eventually paralyzing your whole body. In its most severe, form Guillain-Barre syndrome is a medical emergency. Most people with the condition must be hospitalized to receive treatment.
There’s no known cure for Guillain-Barre syndrome, but several treatments can ease symptoms and reduce the duration of the illness. Although most people recover completely from Guillain-Barre syndrome, some severe cases can be fatal. While recovery may take up to several years, most people are able to walk again 6 months after symptoms first started. Some people may have lasting effects from it, such as weakness, numbness or fatigue.
Types
Guillain-Barre syndrome has several forms. The main types are:
Acute inflammatory demyelinating polyradiculoneuropathy (AIDP)
Progressive para or tetraparesis, sensor deficits, hypo or areflexia, with or without cranial nerve involvement with over month recovery
Acute motor axonal neuropathy (AMAN)
Mainly motor deficiency with pain or sensory loss, with deep tendon reflex absent, with rapid or slow recovery
Acute motor-sensory axonal neuropathy (AMSAN)
Similar to AMAN but with a sensory deficit, usually with a severe disease course.
Miller Fisher syndrome (MFS)
Progressive weakness from distal to proximal begins with weakness of orbital muscles, areflexia, ataxia, and dysphagia.
Case presentation
A 59 years old male patient came to the hospital with multiple episodes of loose stools for two to 3 days.
- H/O tiredness 1 day,
- H/o dizziness and profuse sweating for 1 day,
- H/o two episodes of hematemesis at ER,
- O/E patient was conscious and obeying, moving all four limbs,
- LCN: Normal,
- Vitals: BP: 200/110 mmHg, PR: 72 bpm, RR: 20 bpm, SpO2: 98% in RA.
Course in the hospital
The patient deteriorated rapidly after admission with progressive ascending weakness of limbs and was subsequently intubated. He was evaluated for his symptoms and significant demyelinating/axonal neuropathy was detected. Based on the symptoms patient was suspected of GBS (AMAN) and treated with IvIG, Antiplatelet, Neuro protectants, Physiotherapy and supportive care.
On the second day of admission, the patient had a transient decrease in sensorium for which a CSF study (normal) and MRI Brain were done. MRI features suggested brainstem encephalitis/infarct in the medial medulla and medications continued.
Patient sensorium improved to obeying commends and B/L upper limb minimal movements present to pain stimulus. Adequate physiotherapy was given.
He underwent a tracheostomy for adequate chest toileting and early weaning off from the ventilator, Patient had increased tracheal sensation and persistent temperature spikes. Tracheal aspiration showed Pseudomonas growth and was managed appropriately.
He improved well symptomatically without any fresh deficits, and gradually weaned off to a tracheal tube to room air. The patient was given a trail of tracheal tube de-cannulation maintained for about a day and developed tachypnea and strider and reinserted.
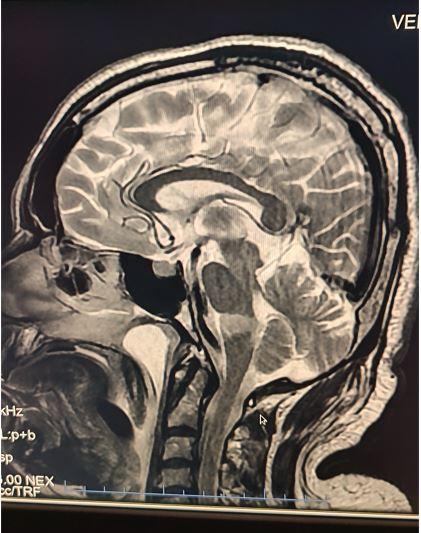
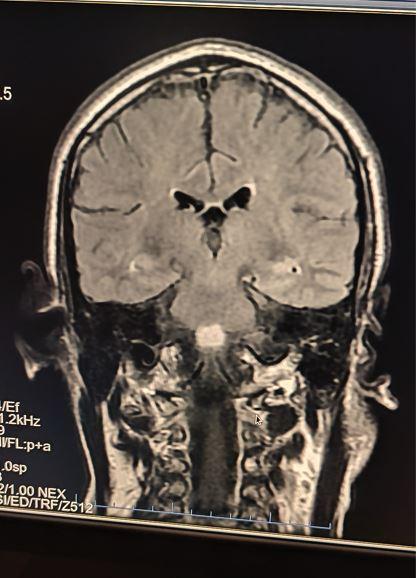
MRI Brain (sagittal and coronal view)
Condition on discharge
Patient is conscious and obeying commends
- On TT: Room air, B/L lower limb power:0/5, B/L Upper limb power: 0/5 (minimal movement present to pain).
Physiotherapy management for the patient during the hospital stay
Assessment
- Muscle tone: Flaccid
- Muscle tone: Flaccid
- Muscle Power: 0/5 (MRC grading)
- Deep Tendon Reflexes: Areflexia
- Balance: Neck control and sitting balance poor
Management:
Inside the ICU
- Patient was given adequate chest physiotherapy for maintaining a patent airway.
- Passive ROM exercise given to all four limbs to maintain muscle and joint integrity and to prevent DVT (DVT stocking was also donned).
- Patient was mobilized to chair sitting with a tracheostomy to improve lung compliance and to gain the patient’s confidence.
- Lower limb positioning was done with a foot drop splint and sandbag.
- Ensured the position was changed regularly to prevent bedsore.
In ward
- Along with all these management, the patient was ambulated to high sitting to improve neck control and sitting balance.
- Patient was ambulated to a chair sitting with sacral cushion support for patient comfort.
- Electrical stimulation was given to antagonist muscle groups of all four limbs to improve muscle tone and prevent muscle wasting.
- Proprioceptive neuromuscular facilitation techniques, muscle tapping and stroking, quick icing and joint compression were given to facilitate and enhance the muscle activity.
Discussion
On referral patient was intubated on ventilator support and GCS was E1 Vt M4 muscle power was 0/5 (all four limbs), after the second day of admission GCS was improved to E4 Vt M6. Chest physiotherapy was given for tracheal toileting ambulated to a chair to improve chest compliance. The patient was transferred out to the room side and electrical stimulation and balance training were given as mentioned above. Discharge advice was given to the patient attender and advice to review at the physiotherapy department during every hospital visits. Patient visito our department after one month for review, when we assessed the patient, his muscle power was improved from 0/5 to 2+/5 in right upper limb and 1/5 in left upper limb, 2-3/5 in both lower limbs. During this one month they continued physiotherapy in their home as per our prescribed exercise protocol.



References
- Intensive Care and Treatment of Severe Guillian-Barre Syndrome done by Pei Shang, Jiachun Feng, Wei Wu and Hong-Liang Zhang
- Intensive Care and Treatment of Severe Guillian-Barre Syndrome done by Pei Shang, Jiachun Feng, Wei Wu and Hong-Liang Zhang
- Role of physiotherapy in Guillian-Barre Syndrome: A Narrative Review done by Shah Nehal, Shirivasrava Manisha
- https://rarediseases.org/rare-diseases/guillain-barre-syndrome
- Tidy’s Physiotherapy- Stuart Porter
- Therapeutic exercise- Carolyn kisner
- www.physio-pedia.com

