Leema Rebakkal Rosy,*, Sathiya Prabha
Assistant Nursing Superintendent, Kauvery Hospital, Tennur
Staff Nurse, Kauvery Hospital, Tennur
Teamwork makes a Dreamwork
Background
Viper envenomation is a potentially life-threatening disease caused by toxins in the bite of a venomous snake. Vipers, which include adders and rattlesnakes, have venoms that are generally hemotoxic. This means they attack the circulatory system. They can cause bleeding or interfere with the blood’s ability to clot. Viper envenomation is responsible for inflammatory disorders, hemorrhagic complications and local or extended necrosis. The occurrence of respiratory distress syndrome is exceptional.
Case Presentation
We have reported here the case of a 36-year-old lady who presented with alleged h/o snake bite at her farm near home on 05.05.2022 at 03.45 pm. Clinical evaluation correlated to haemotoxicity. Her right leg had swelling with great toe discoloration (+). H/o decreased output and high colored urine.
No comorbidities were found. Patient was hemodynamically stable, pedal edema +. She was started empirical antibiotics, PPI and other supportive measures.
In view of worsening renal function which was Acute Kidney Injury (AKI) Haemo Dialysis (HD) was planned and dialysis initiated. Wound debridement was done and shifted to ward. Due to worsening coagulopathy multiple transfusions were given.
On 14.05.2022, after 9th days of hospitalization, her condition was worsening due to pulmonary edema, accelerated HTN, tachycardia and dyspnea. She was shifted to ICU and intubated as she was not able to tolerate NIV.
Echo cardiogram revealed severe LV dysfunction due to septic myocarditis.
POWS revealed ARDS features. She needed high ventilator support. So, she was put on prone position due to worsening of ARDS and desaturation.
Discussion
ARDS management in patient with sepsis is always tricky and has to be dealt with cautiously. Appropriate planning and execution of case management with backup plan is vital in such challenging situations. Competency of entire team involved and good communication between the team members helps successful management of the patient and avoiding of serious complications such as aspirations, hypoxia, secure airway, pressure injury etc.
Medical Management
She was in need to be treatment with high-end antibiotics, diuretics, beta-blockers and anti-arrhythmic drugs due to severe LV dysfunction ARDS, AKI, hypertension, sepsis etc. Renal parameters and urine output were worsening, so we continued hemodialysis. We did all cultures like blood, urine and trachea secretions, which were negative for growth.
As she had necrosis of Rt great toe, after extubating, we planned for right great toe amputation.
Surgical Management
On admission, patient’s right leg had swelling with discoloration.
- Right foot wound debridement was done on 07.05.2022.
- Wound debridement was done on 12.05.2022
- Great toe amputation was done on 23.05.2022 due to necrosis
Mechanical Ventilator Management
On the 9th day of hospitalization, she developed breathlessness and pulmonary edema so she was shifted to ICU. Initially, she was treated with NIV support which she did not tolerate. So, she was intubated and put on mechanical ventilator support. Sedation reduced agitation and anxiety. Constantly we monitored the vital signs.
Even though the patient was on mechanical ventilation she had persistent hypoxia, and chest x-ray showed features of ARDS. Clinical evaluation also indicated ARDS. It was decided that she needs hyperventilation; entire team discussed to change prone position for 24 h. She needed high peep and high FiO2 (pressure control) ventilation. We have titrated the PEEP up to a high level of 25 to 30 cm. Because PEEP can increase intrathoracic pressure that can lower cardiac output, hemodynamic monitoring was done to determine the best PEEP setting each time for the patient. Continuous positive airway pressure at 35 to 40 cm H2O for 30 to 40 s can also open collapsed alveoli without severe hemodynamic compromise or barotrauma.to protect lung ventilation We have monitored the patient for changes in respiratory status such as increased respiratory rate, breath sounds, decreased oxygenation saturation and dyspnea every hourly, and after every change in PEEP or VT. We focused on limiting the plateau pressures to less than 30 cm H2O, maintaining PEEP, reducing FiO2 to 50 to 60%, Weaning protocols can reduce the time and cost of care while improving outcomes of patients in view of resolving sepsis. AKI was improving. Weaning trial was done on 20.05.2022. Patient’s health status improved and she was extubated on 21.05.2022.
Nursing Diagnosis
1. Ineffective breathing pattern: Related to increased breathing rate as evidenced by dyspnea, tachypnea, changes in the depth of respiration and restlessness.
Desired outcome: The patient should be taking relaxed breathing at a normal rate and depth. Should have absence of dyspnea and blood gas analysis should show normal parameters
2. Impaired gas exchange: Related to the abnormal gas concentration of oxygen and carbon dioxide as evidenced by hypoxia and restlessnessx
Desired outcome: The patient should be able to maintain adequate gas exchange as evidenced by normal ABG findings and no sign of any breathlessness, tachycardia, or any anxiety.
3. Risk for decreased cardiac output: Related to mechanical ventilation- positive pressure ventilation
Desired outcome: Is that the patient maintains required cardiac output as evidenced by strong peripheral pulsations, heart rate between 60-100 beats/min, normal blood pressure and urine output greater than 30 mL/h.
4. Risk for ineffective airway protection: Related to increased secretions, improper ventilator setting, improper alarm setting.
Desired outcomes is injury-free patient as evidenced by proper ventilator setting and appropriate arterial blood gases limits.
5. Anxiety related to inability to breathe, change in environment, change in health status as evidenced by restlessness, withdrawal, tachypnea, eyes on equipment and monitors, and tense facial expression.
Desired outcome is that the patient shows reduced anxiety, as evidenced by a calm manner and cooperation. The patient uses effective coping mechanisms.
Nursing Management
1. Perfusion
External mechanical ventilation causes decreased venous return to the heart. As a result, blood pressure decreases, heart rate increases and cardiac output decreases. As the brain cannot not get enough oxygen, the level of consciousness alters. Inotropic medications cause an increase in cardiac output. The goal of care for ARDS patients is to maximize perfusion in the pulmonary capillary system by increasing oxygen transport between the alveoli and pulmonary capillaries. To achieve the goal, we have increased the fluid volume without overloading the patient, and avoid inotropes support.
2. Positioning
Prone positioning improves the V/Q ratio. Ventilation improves because the heart no longer compresses the posterior areas of the left lung as it does in the supine position. With the patient in the prone position, most lung tissue, which is in the posterior areas, moves toward the anterior, clearing the airways of debris, decreasing atelectasis, reducing lung inflammation, and producing more efficient oxygenation and perfusion. So, patient is put on prone position, with pillows supporting the chest and pelvis to allow the abdomen to hang free and gel pad applied to support the chin. Every couple of hours assess the pressure points, and evaluate the patient’s volume status by measuring blood pressure, mean arterial pressure, central venous pressure, and urine output and venous oxygen saturation.
After 24 hours of proning our patient did not show any improvement and again went into hypoxia. The team planned 48 hours of continuous proning to increase the oxygen concentration. Patient showed good response to proning, which was continued for 4 days. She was on an improving trend on the subsequent days.
Suctioning clears the secretions, improves breathing and increases airway patency, so we did suctioning on the basis of objective data rather than time intervals.
During prone position, to prevent pressure injury and HAI, are very challenging to nursing team. So. our team is fully focused on bundle care adherence to prevent HAI. For pressure injury prevention, we applied a gel pad to support the head and chin, and at all the bony promises water bag was applied. In spite of all the preventive measure we found skin damage in the chin (grade 2 pressure injury); we took immediate measure and focused on preventing its extension. It healed within a week. Gradually she responded to ventilation and her oxygenation improved, so weaning was done on 7th day, and extubated.
3. Nurses’ role in preventing complications:
The most common complications are deep vein thrombosis (DVT), pressure ulcers, decreased nutritional status, and ventilator-associated pneumonia (VAP). So our nursing team together decided to do frequent risk assessment and take preventive measures
Prevention of DVT
Deep Vein Thrombosis is an acute condition characterized by inflammation and thrombus formation in the deep veins that may lead to pulmonary embolism. About 16% of patients receiving mechanical ventilation develop DVT, typically during the first 5 days in the ICU. To prevent DVT, we followed range-of-motion exercises, frequent position changes, anticoagulant prophylaxis, and used compression devices and thromboembolic stockings. this preventive measure we have started immediately when the patient under gone ventilator support.
Prevention of Pressure ulcers
Because of poor tissue perfusion and limited movement, pressure ulcers may develop. Our patient had high risk to develop pressure injury; the measures our team took to prevent this complication include relieving pressure with frequent position changes, restoring circulation with mobility, and promoting adequate nutrition. By assessing our patient skin frequently, provided meticulous skin care, monitored nutrition status, and implemented pressure-relieving devices such as air mattresses, instead of all this measure patient had mild skin pealing on the chin due to 48 h of prone position for that strictly followed push chart and healed within a week
Prevention of deteriorating nutritional status
ARDS patients have a severely compromised nutritional status, so we have started nutritional support as soon as possible within 24 h of intubation. Our preferred support method is enteral nutrition because it causes fewer complications than parenteral nutrition. When we are managing the ARDS patient, we consulted with a dietitian and provided high protein diet every two hourly to prevent hypo albuminemia.
Prevention of VAP
As many as 40% of ARDS patients develop VAP, which is nosocomial pneumonia that develops after 48 hours or more of mechanical ventilation. Most cases result from aspiration of bacteria from the mouth and GI tract. This condition complicates the ARDS patient’s recovery who would require a longer duration of mechanical ventilation and longer length of stay. By following evidence-based practice we saved the patient from VAP, improved patient outcome and decreased the length of stay in ICU.
Ventilator alarms: We ensured the alarms of the ventilator are on. Immediately we informed intensivist of any discrepancies in ventilator settings and assessed the oxygen saturation through pulse oximetry. We did ABGs as per need and assessed the rate and rhythm of the patient’s respiratory pattern. We also checked for signs of pulmonary infection, as well as for signs of barotrauma. By following evidence based practice we saved our patients from complications.
4. Psychological and emotional support:
She and her relatives were very anxious which occasionally made decision-making on daily treatment difficult. Daily, ongoing treatments were explained to the relatives. When the patient was facing a problem in communication, we provided a writing pad and pencil, and received and rectified her needs. She was conscious on ventilator and she communicated through action and appreciated the nurses and their dedication. Our team gave full psychological support to patient to overcome from the critical state
Social and financial status wise her family members were handicapped. Sample drugs of high-cost medications were arranged and administered
Condition at discharge
Patient’s renal parameters and lab values normalized, vitals became stable, she clinically improved, was in good general condition and wound was clean. We gave emotional and psychological support to the patient and family members, and achieved best communication and coordination with other team members.
She was discharged on 22nd day and went home happily
Conclusion
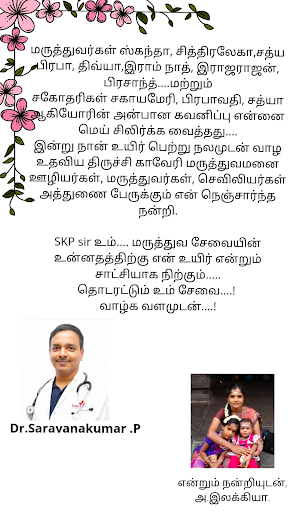
Nurses are responsible for recognizing patients symptoms, taking measures within their scope of practice, to administer medications, providing other measures for symptom alleviation and collaborating with other professionals to optimize patients comfort, and families understanding and adaptation. Early identification of hypoxia had a better outcome in our patient. Patients’ satisfaction with nursing care energizes elevating quality of nursing care. It facilitates the creation of high standards of care. Monitoring both results and patients’ perceptions of quality help. This patient sent testimony to our nursing team. Patient testimonials are one of the most powerful ways to earn trust and attract new patients to your practice.