Jaya Menon1,*, Ruby Ravichandran2, J. Jenma Rakkini3, S. Deepa3, D. Santhi3, P. Uma4, N. Suganya Periya Nayagi4
1Nursing Superintendent, Kauvery Hospital, Trichy-Cantonment, India
2Deputy Nursing Superintendent, Kauvery Hospital, Trichy-Cantonment, India
3Supervisor, Critical Care, Kauvery Hospital, Trichy-Cantonment, India
4Incharge, Critical Care, Kauvery Hospital, Trichy-Cantonment, India
*Correspondence: jayamenon@kauveryhospital.com
The revolutionary effect of a nursing-driven initiative to reduce ICU re-admissions
Problem statement
Hospital stays are a frightening and financially draining experience for the average person. The experience of living with a critically ill, bedridden patient is profoundly traumatic for their families, even the chronically sick. The readmission of a ward patient to a critical care unit is one of the most distressing situations.
Adverse events can occur when patients are transferred from the intensive care unit (ICU) to the non-intensive care unit. Very often, this is due to patients with severe illnesses transferring to environments with lesser processes and machines to monitor progress and more subjectivity to environmental factors and human capabilities as present in a ward. In some cases, complications may arise despite recovery after ICU discharge and not requiring lifesaving therapies, leading to unplanned readmission or even death.
What is the literature saying?
After being transferred from the ICU, patients have a 10% chance of being readmitted [1]. Readmissions to ICUs have been identified as a problem that results in poor patient outcomes, including a four-fold increase in the risk of hospital mortality and resources consumed [2]. Readmissions also impact the hospital system regarding the availability of ICU beds [3]. It is common for patients to be discharged from surgical trauma or the medical ICU too early or unplanned discharge. It is a significant driver of ICU demand. Patients with critical trauma or emergency surgery present 24 h a day and demand Surgical Trauma ICU (STICU)-level care, leading to an increasing trend of releasing patients from the ICU sooner and sicker and an ever-changing roster of patients in the STICU [4].
There are several contributing factors. Typically, a large volume of patient turnover within the ICU occurs in the middle of the night, when most traumas occur, often resulting in 5 poorer patient outcomes. In addition, clinicians are increasingly challenged to transfer patients out of the ICU to free up beds for others in need. An increase in patients’ lengths of stay will also impact hospital beds. To determine which patients are appropriate to be admitted or discharged from the ICU, the staff must frequently triage to meet the constant need for ICU beds [5].
Readmission to critical care units has been associated with an increased mortality rate, a longer length of stay, higher complications, and increased costs. ICU re-admissions increased the risk of prolonged hospital stay by two-fold [6]. The impact of readmission on hospital budgets is staggering [1-6].
Aim and objective
Early Identification of such patients is possible because there are indicators and is a common observation that points toward an increase in complications. This situation necessitates identifying strategies to prevent premature discharge from the ICU.
Our critical care nurses attempted to reduce these incidences with collaborative inputs by collecting data on total transfers out to wards, IP critical transfers within 72 h, code blue and MET calls, as well as de-lining of tubes and drains from all critical care units, including Neuro ICU, IMCU, PICU, and PIMCU.
(1) The objective of this initiative was:
(2) To improve the continuous patient care
(3) To improve patients’ satisfaction and safety
(4) To aid patients who cannot afford extended stays in ICUs
(5) To improve positive feedback and avoid negative feedback
(6) To avoid IP patients’ critical care re-transfer within 72 hrs
(7) To avoid MET calls and Code Blue
(8) To improve knowledge of handling tubes and drains
(9) To prevent novices from being afraid.
(10) Better management of the workforce
Methodology
The department heads drafted protocols to enhance patients’ overall well-being and reduce their anxiety, address all health-related questions, care for tubes and drains, and manage medications in conjunction with Modified Early Warning Score (MEWS).
MEWS is a reliable and safe system that scores patients based on their vital signs. MEWS gives scores for Respiratory Rate, Heart Rate, Systolic Blood Pressure, Level of consciousness, Temperature, Urine Output for over 2 hours or more, and Oxygen Saturation. According to the MEWS, a score of five or more is statistically linked to an increased likelihood of death or readmission to a critical care area. In medical emergency units where the staff was trained to use MEWS as a track and trigger system, it proved to be a helpful tool for patient triage and monitoring, thus improving patient care and ensuring optimal utilization of resources [7].
Therefore, nurses assessed the readiness of a patient to transfer by utilizing the NEWS. A final evaluation of the tool’s effectiveness focused on the primary outcome goal: to decrease the number of patients requiring ICU readmission within 72 h.
At multiple levels, the team had to address the challenge – identify the need for critical care transfer, estimate the odds of adverse events, describe the reasons behind unfavourable status changes, and formulate the clinical decision and management plans based on those factors.
Results
In the study, abnormal vital signs typically preceded patients’ deterioration in the hospital. A composite score is developed by comparing these observations to normal vitals. A proforma was developed to track patient progress and readmissions, if any. The “72 hours checklist,” as it was soon referred to by nursing personnel, was developed for patients transferring out of the intensive care unit.
The study collected data on total ICU patient transfers to wards, IP critical transfers within 72 h, code blue & MET calls, de-lining of tubes & drains, and HIC adherence from all critical care areas such as Neuro ICU, IMCU, PICU, PIMCU. An attempt was made to analyze the dynamics and address them with collaborative inputs.
As per the observations, in 2020, IP critical care re-transfers within 72 h were 17.3% and then dropped significantly to 4.7% in 2021, as shown in Fig. 1.
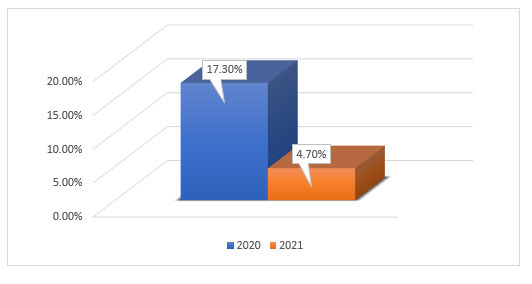
Fig. 1. Critical care bounce back within 24 h.
This observation was based solely upon NEURO ICU observation. In all patient transfer areas of the hospital, there were similar numbers of untoward incidents, with positive feedback increasing and negative feedback decreasing.
Conclusion
In critical care, patients transferred out are not necessarily out of risk since the underlying cause of further risk is unknown. Therefore, there is a high chance of ICU readmission within 72 h of transfer. Continual monitoring by nurses on the ward assures a patient’s safety and progress. Nurses have a wide range of clinical responsibilities, including their role as patient supporters. Nurse-driven initiatives and enhanced care could help reduce readmissions significantly.
As observed in our study, critical care nurses could enhance nurse-patient relationships and their competencies with their supervision and guidance, enabling them to provide a fearless environment for ward care nurses. As a result of a fearless environment that was created and prototypically facilitated, nursing care practice and delivery thrived, and patient satisfaction increased tremendously.
References
[1] Ponzoni CR, Corríªa TD, Filho RR, et al. Readmission to the intensive care unit: Incidence, risk factors, resource use, and outcomes. A retrospective cohort study. Ann Am Thorac Soc. 2017;14(8):1312-9.
[2] Hosein FS, Bobrovitz N, Berthelot S, et al. A systematic review of tools for predicting severe adverse events following patient discharge from intensive care units. Crit Care. 2013;17(3):R102.
[3] Fakhry SM, Leon S, Derderian C. Intensive care unit bounce back in trauma patients: An analysis of unplanned returns to the intensive care unit. J Trauma Acute Care Surg. 2013;74(6),1528-1533.
[4] Christmas AB, Freeman E, Chisolm A, et al. Trauma intensive care unit “bouncebacks”: Identifying risk factors for unexpected return admission to the intensive care unit. Am Surg. 2014;80(8), 778-782.
[5] Utzolino S, Kaffarnik M, Keck T, et al. Unplanned discharges from a surgical intensive care unit: readmissions and mortality. J Crit Care. 2010;25(3):375-81.
[6] Kramer AA, Higgins TL, Zimmerman JE. Intensive care unit readmissions in U.S. hospitals: Patient characteristics, risk factors, and outcomes. Crit Care Med 2012;40(1):3-10.
[7] Bhatnagar M, Sirohi N, Dubey AB. Prediction of hospital outcome in emergency medical admissions using modified early warning score (MEWS): Indian experience. J Family Med Prim Care. 2021;10(1):192-8.

