Typhoid: A prospective observational study
P. Siranjeevi, B. Rubeshwaran
Clinical Pharmacist-Internship, Kauvery Hospital, Trichy
Abstract
Typhoid fever is an infectious disease that exclusively affects humans and is transmitted by feco- oral route. The main symptoms of the disease are fever, nausea, abdominal pain, and others such as indigestion, headache, chills, loss of appetite and back pain. In developing countries, typhoid is a disease that frequently affects travelers, such as tourists, soldiers, temporary workers, or travelers. Encephalopathy, gastrointestinal bleeding, nephritis, and hepatitis are common complications occurring in 5–7% of hospitalized patients, and gastrointestinal bleeding or colitis and intestinal perforation may also occur. A complete blood count, blood culture and Typhoid serology are the ways to confirm the diagnosis by isolating bacteria and testing for antibodies. The Widal test measures antibodies to O and H antigens of Salmonella typhi and Salmonella Para typhi A. Other rapid tests detect IGM antibodies to Salmonella Typhi antigens. This study was conducted with the aim to determine the clinical manifestation and treatment. Chloramphenicol, ampicillin, and co-trimoxazole were the first-line treatments for typhoid fever globally, until resistance to these three drugs emerged in the late 1980s. The bacteria became resistant to these drugs which led to the increasingly common use of fluoroquinolones, such as ciprofloxacin and ofloxacin. Resistance was later seen against these quinolones too. We noted that maximum patients in our series were treated with ceftriaxone and azithromycin. The carbapenems (imipenem, meropenem and ertapenem), oral penems (faropenem) and tigecycline may emerge as potential alternatives.
Introduction
Typhoid is a bacterial infection caused by the Gram-negative bacterium Salmonella enterica, subspecies enterica serovar Typhi (S. typhi). Typhoid fever is usually contracted by ingestion of food or water contaminated by faecal or urinary carriers excreting S. typhi. The predominant symptom of infection is high fever, with other symptoms including nausea, abdominal pain and abnormal bowel movements, headache, chills, loss of appetite, back pain. In developed countries, typhoid fever is a predominantly travel- associated disease. The 2017 World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization (SAGE) have recommended the introduction of typhoid conjugate vaccines (TCVs) for infants and children aged >6 months in typhoid-endemic countries.
Pathophysiology

Once contaminated food and water are consumed, typhoid bacteria cross the epithelial layer of the intestinal wall. They are then quickly consumed by macrophages and transported to the aggregates of lymphoid tissue in the small intestine (Peyer’s patches) where the immune function of the gut is most concentrated. The typhoid bacteria alter host cell signalling and function in such a way that host cells ultimately promote the survival and replication of S. typhi and S. para typhi. The incubation stage of a typhoid infection is characterized by the replication and transfer of S. typhi and S. para typhi from the Peyer’s patches in the gastrointestinal system, through the lymphatics, to the organs of the reticuloendothelial system including the lymph nodes, spleen, bone marrow, and liver. This results in varying degrees of necrosis and ulceration of Peyer’s patches of which the clinical manifestation is
bleeding and perforation. The terminal ileum is the most common site of perforation, but perforation has also been reported to occur anywhere from the duodenum to the colon including the gall bladder and appendix.
Depending on the strength of the host’s immune system and the size of the inoculum, the incubation phase may last 3 days to 3 weeks. During this interval, a patient may have no symptoms or vague complaints of fever and abdominal pain. Once the bacterial load reaches a critical mass, an individual is said to have an active typhoid infection.
Epidemiology
Typhoid is more common in urban than rural areas. Worldwide there are over 22 million cases with over 200,000 deaths each year, representing a 1-4% mortality rate. Typhoid and paratyphoid infections are relatively common in countries with poor water supply and sanitation, especially south Asia, southeast Asia, and sub-Saharan Africa, where they are a major cause of death and disability, especially among children.
Signs and symptoms
- typhi is four times more common than S. para typhi, in general, the clinical features of S. typhi and S. para typhi infections are virtually indistinguishable.
Signs and symptoms of the infection consist mostly of abdominal complaints including fever associated with frontal throbbing headache, nausea, vomiting, abdominal pain, anorexia, diarrhoea, constipation, gastrointestinal bleeding and hepatosplenomegaly, intravascular coagulation, haemolytic uremic syndrome, renal failure, cardiac failure, and respiratory failure
Neurologic problems include meningitis, Guillain-Barre syndrome and delirium.
Complications
Severe disease usually manifests in the second or third week of illness with continuing fever, increasing weakness, anaemia, weight loss, persistent vomiting, or a clouded mental state. Delayed treatment, the virulence of the bacterial strain, and host factors contribute to disease severity.
Cruz Espinoza LM, McCreedy E, Holm M, et.al., study found that Encephalopathy, gastrointestinal bleeding, nephritis, and hepatitis are common complications seen in 5-7% of hospitalised patients and also intestinal haemorrhage or colitis and intestinal perforation can occur. These present with signs of acute peritonitis or more insidiously with increasing restlessness, a diffusely tender abdomen, hypotension, tachycardia, and shock.
Diagnosis
Complete blood count and blood culture are done. Blood culture is the optimum method to confirm the diagnosis by isolating the organism and testing antimicrobial sensitivity.
C reactive protein (CRP) is usually elevated in enteric fever. Serological tests, including the Widal test, and newer rapid diagnostic tests are carried out.
The Widal test measures antibodies against O and H antigens of S Typhi and S. para typhi A. It is cheap and simple but lacks sensitivity and specificity.
Other rapid diagnostic tests detect IgM antibodies against S Typhi antigens.
Bone marrow culture gives a higher yield, but it is rarely performed. Faeces, urine, or bile aspirate may be cultured.
Our study
This study was conducted with the aim to determine the clinical manifestation and treatment.of Enteric Fever
Study type: A prospective observational study.
Study site: The study was conducted at Kauvery Hospital Cantonment Trichy.
Study Duration: The study was conducted from the period August 2024 – October 2024 (Period of 3 months).
Study population with sample size: Ten (10) patients were enrolled in the study.
Statistical Analysis: The data were subjected to descriptive statistical analysis by using Microsoft Excel.
Results
A prospective observational study of Typhoid patients was taken for the period of three months from Aug 2024 – Oct 2024. All the data were interpreted. The study assessed the outcomes of patients with Typhoid, treatment and clinical presentation of patients.
Total of 10 patients of typhoid positive were admitted to Kauvery Hospital, Cantonment. Data were collected and the significance of findings was tested and data interpreted.
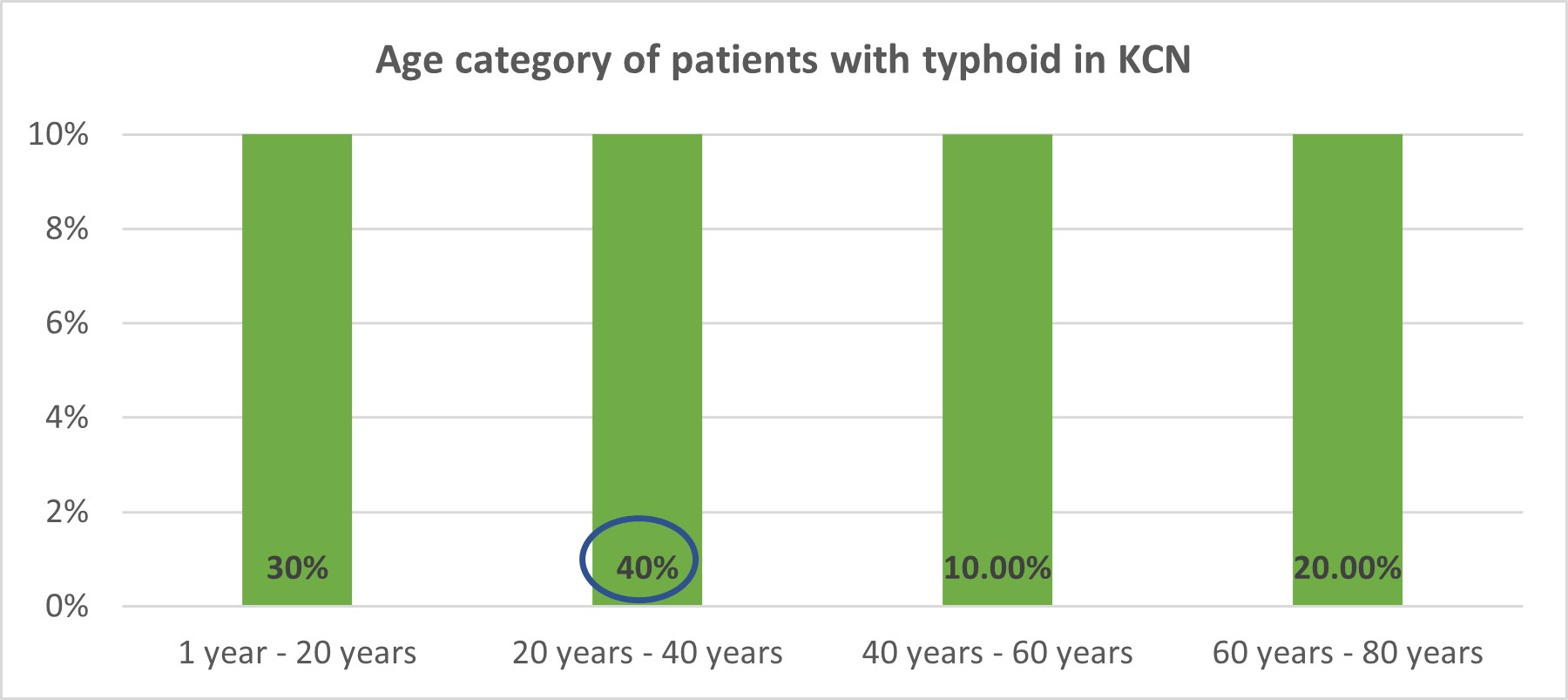
1. Age category of patients with typhoid in KCN
2. Gender category of patients with typhoid in KCN

3. Symptoms category of patients with typhoid in KCN

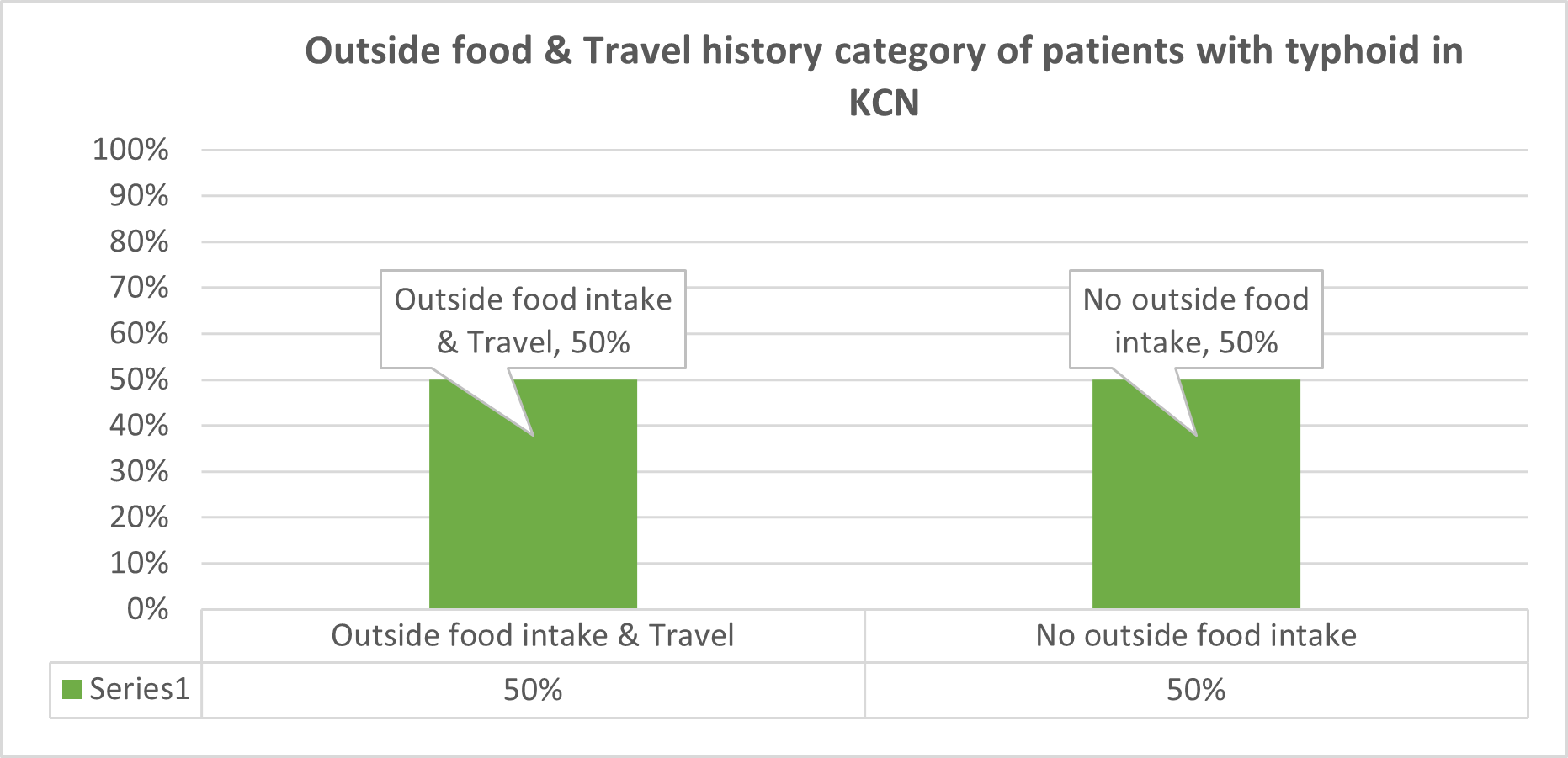
4. Outside food & Travel history category of patients with typhoid in KCN
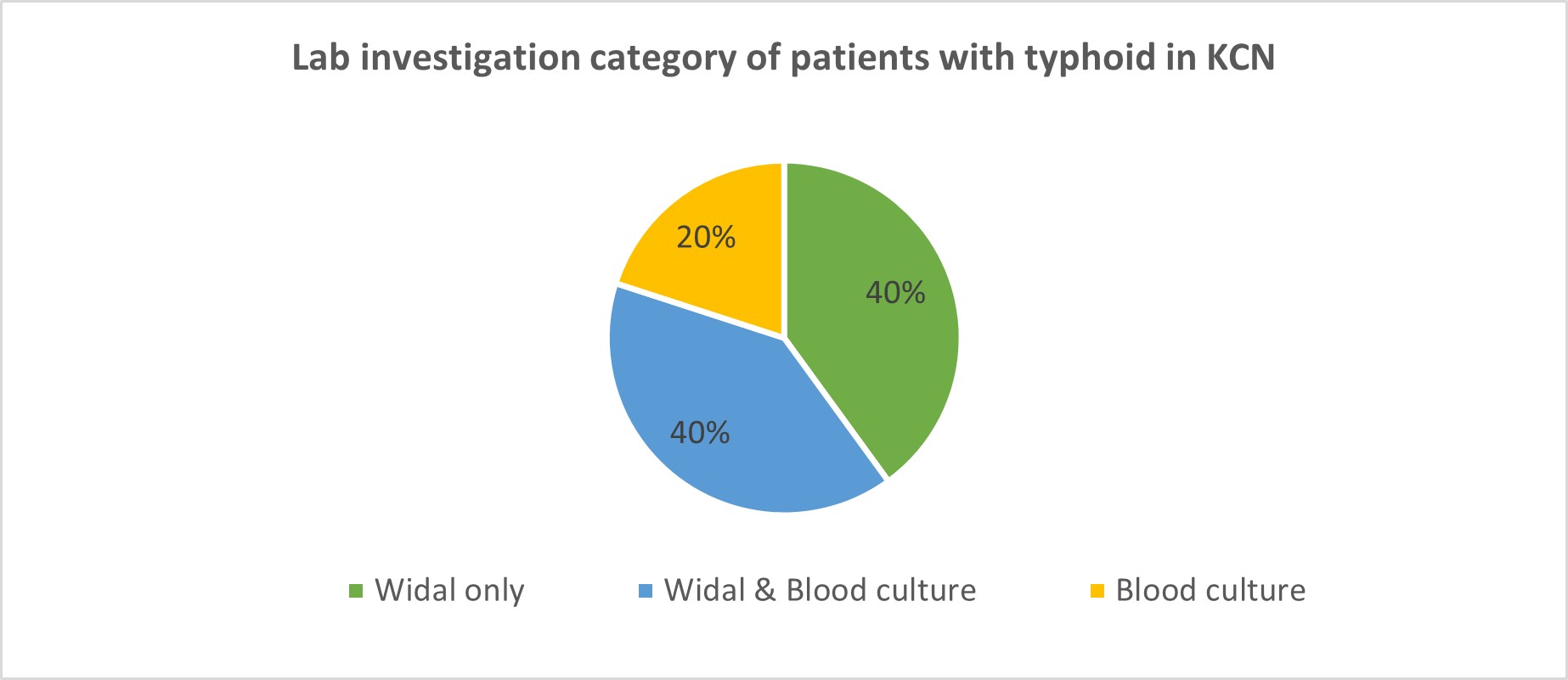
5. Lab investigation category of patients with typhoid in KCN
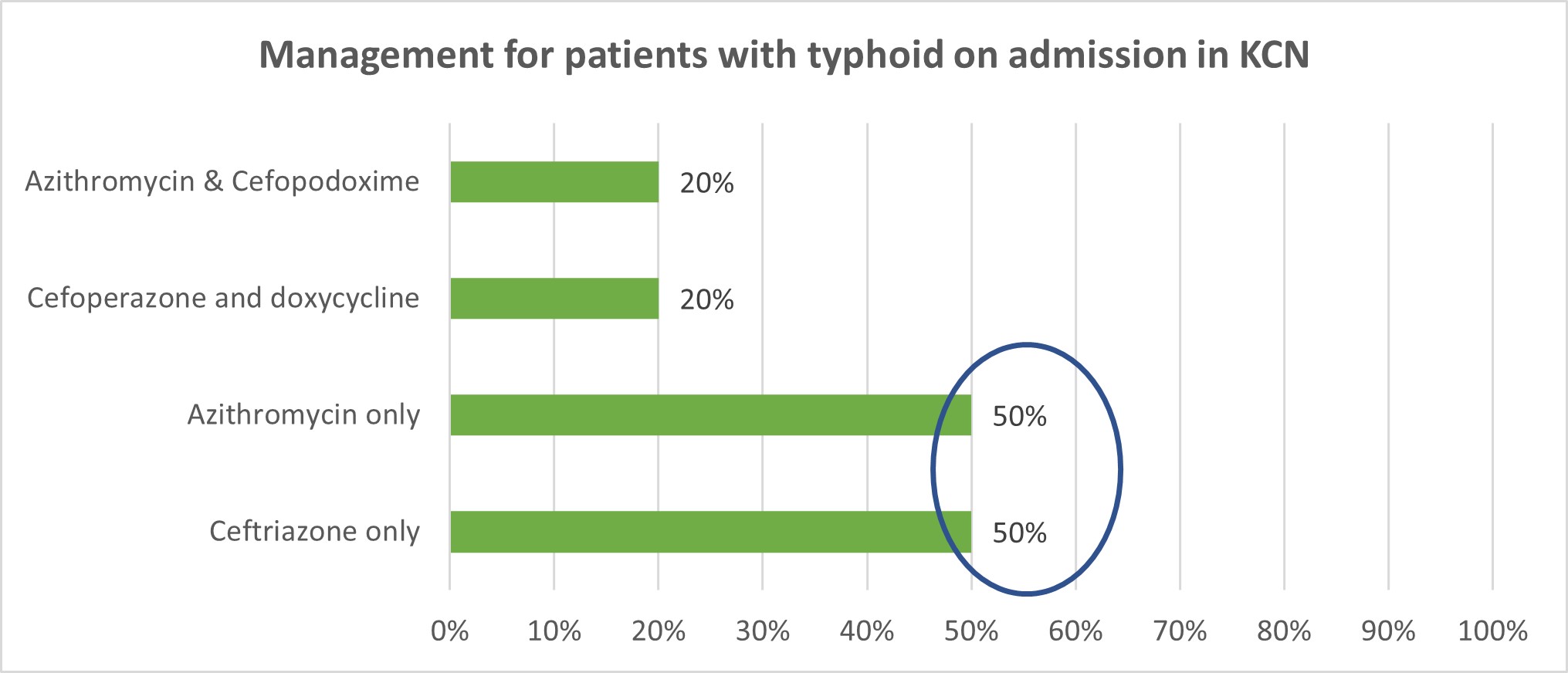
6. Management for patients with typhoid on admission in KCN
7. Discharge medications for patients with typhoid in KCN

Discussion
- The present study was carried out to determine a clinical manifestation and management.
- Out of 10 patient’s 7 were male (70%) and 3 were female (30%).
- Among 10 patients in our study, they were categorized by four different age groups of 01-20, 21-40, 41-60 and 61-80 in which the age group 20-40 yrs has 4 patients (40%), 01-20 yrs has 3 patients (30%), 60-80 yrs has 2 patients (20%), 41-60 yrs has 1 patient (10%).
- Among 10 patients in our study, there were 50% of patients had fever, vomiting and headache, 25 % of patients had fever, loose stools, abdominal pain and another 25% of patients had Fever, chills, body pain, vomiting. Fever was common to all.
- Cruz Espinoza LM, McCreedy E, Holm M, et.al., study had reported encephalopathy, gastrointestinal bleeding, nephritis, and hepatitis as common complications seen in 5-7% of hospitalised patients and also that intestinal haemorrhage or colitis and intestinal perforation can occur. These present with signs of acute peritonitis or more insidiously with increasing restlessness, a diffusely tender abdomen, hypotension, tachycardia, and shock. None of these complications were reported from our study.
- Out of 10 patients 50 % had travel history and also of having consumed street food . CDC Yellow Book 2024 had reported that approximately 85% of typhoid fever and 92% of paratyphoid fever cases in the United States occur among international travellers; most are in travellers returning from South Asia, primarily Bangladesh, India, and Pakistan.
- Among 10 patients 40 % had widal test reported, 40% had both widal and blood culture reported, 20% had blood culture. They were the diagnostic tests done in the study by Zulfiqar A Bhutta. “Current concepts in the diagnosis and treatment of typhoid” falso mention these diagnostic tests
- In our study, the treatment with antibiotics was as follows: 50% patients were treated with ceftriaxone only, 50% patients treated with azithromycin only, 20% of patients treated with azithromycin & cefpodoxime combined therapy and 20% of patients treated with cefoperazone & doxycycline.
- 60% patients were given cefixime on discharge, 20% with azithromycin and rifaximin. 10% with amoxicillin & Doxycycline.
- In the study of Ashraf Mahmoud et al., Adekunbi Oluyemisi et al., Recent advances in the diagnosis and management of typhoid fever in Africa: A review found that Fluoroquinolones confer an added advantage over cephalosporin’s; however, the decreased sensitivity of ciprofloxacin on emerging resistant strains has limited their usage, mainly in Asia.
- Azithromycin and extended-spectrum cephalosporin’s offer an alternative to manage decreased fluoroquinolone sensitive typhi.
- Combining cephalosporin’s and azithromycin customarily produce a potent regimen to treat patients who fail to respond to fluoroquinolones appropriately.
- The main reason for their use is to extend the antibacterial action range, thereby maximising the regime’s synergy and reducing the risk of developing drug resistance during therapy.
- According to Christopher M Parry, Buddha Basnyat & John A Crump et al, What could we recommend for the treatment if a multiple drug resistant strain with combined resistance to (fluoroquinolones, cephalosporin’s and azithromycin) drugs were to emerge? The carbapenems (imipenem, meropenem and ertapenem), oral penems (faropenem) and tigecycline could be potential alternatives, but there is as yet no clinical trial data to support their use.
Conclusion
In summary, this prospective observational study on typhoid fever emphasizes the importance of timely diagnosis and effective management to improve patient outcomes. Early intervention reduces complications and enhances recovery. The findings advocate for increased public health initiatives, including vaccination and awareness, especially in endemic areas, and highlight the need for ongoing research into antibiotic resistance to optimize treatment strategies. This study also focuses the appropriate treatment patterns for patients.
Reference
- Cristina Masuet- Aumatell et al., Jorge Atouguia et al. Typhoid fever infection – Antibiotic resistance and vaccination strategies: A narrative review. 8 December 2020.
- Cruz Espinoza LM, McCreedy E, Holm M, et al. Occurrence of typhoid fever complications and their relation to duration of illness preceding hospitalization: a systematic literature review and meta-analysis.
- Neta Petersiel ID, Sudeep Shresta et al., The epidemiology of typhoid fever in the Dhulikhel area, Nepal: A prospective cohort study. September 27, 2018.
- Typhoid & Paratyphoid Fever CDC Yellow Book 2024.
- Zulfiqar A Bhutta et al., Current concepts in the diagnosis and treatment of typhoid fever. VOLUME333 8JULY2006.
- The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. February 18, 2019.
- John A et al., Crump et al., Progress in Typhoid Fever Epidemiology. 18 February 2019.
- Falan Mouton et al., Dr. Esohe I. Ohuobaet et al., Typhoid Enteric Fever (Part 1). 4th OCT 2016.
- A. Rahman et al., M. O. Wasfy et al., Multi-drug resistance and reduced susceptibility to ciprofloxacin among Salmonella enterica serovar Typhi isolates from the Middle East and Central Asia. Volume2Number4, July2014.
- Ashraf Mahmoud et al., Adekunbi Oluyemisi et al., Recent advances in the diagnosis and management of typhoid fever in Africa: A review. 7 November 2022.
- Narcisa Muresu et al., Giovanni Sotgiu et al., Travel-Related Typhoid Fever: Narrative Review of the Scientific Literature.18 January 2020.
- Abhilasha Karkeya et al.,, Guy E. Thwaites et al., The evolution of antimicrobial resistance in Salmonella Typhi. 2017.
- Christopher M Parry, Buddha Basnyat & John A Crump et al., The management of antimicrobial-resistant enteric fever. 10 Jan 2014.

