Journal scan: A review of 30 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Mental checklists, constant vigilance: A day living with type 1 diabetes.
No two days are the same. And yet, as humans, we are creatures who thrive on habits and routine, providing us with a sense of manageability in our lives. Meet Nichole Acosta, who has lived with type 1 diabetes (T1D) since she was diagnosed 18 years ago at age 18. T1D, which affects more than 2.5 million people in North America and Europe alone, is a chronic condition in which the pancreas produces little to no insulin, potentially leading to blindness, amputations, kidney failure, and can be fatal unless treated with insulin therapy. Nichole, along with many others who live with T1D, has constructed a carefully managed routine to regulate her glucose levels throughout the day, starting from the second she wakes up, affecting choices she makes every day regarding food, exercise levels, and other daily activities.
Nichole checking her glucose level as soon as she wakes up.
Since Nichole was first diagnosed with T1D, medical devices have improved her life, giving her the power to have more control over her glucose levels and minimize the risk of excessively high or low blood sugar levels. However, despite these improvements, she still makes countless decisions every day and prepares for various contingencies, an unrelenting mental burden.
Nichole wears a continuous glucose monitor (CGM) that sends blood sugar readings to her mobile app every five minutes, tracking her levels. A good start for her in the morning is between 80-150 mg/dl (milligrams per deciliter). This measurement represents the concentration of glucose per unit of blood and could require action to return it to the desired range. For Nichole, she can feel when she has high glucose levels and sometimes experiences fatigue or other symptoms. She has battled T1D for a long time, and often does not notice when her glucose levels go low. This is called hypoglycemia unawareness and puts many people like Nichole at risk for severe reactions, which may require hospitalization. As a result, Nichole relies heavily on her devices to notify her of these changes.
For breakfast, Nichole includes a balance of food groups, doing the math to ensure she receives the right amount of insulin to compensate for carbohydrates. Recently Nichole added an insulin pump to her T1D management arsenal of devices. The pump communicates with her CGM to administer her insulin accordingly. These devices have simplified my life tenfold, she says, as the device she is using adheres to her skin without tubes and delivers her insulin without a syringe.
Another significant part of Nicholes morning routine, in addition to preparing her toddler for daycare, is to run through a mental checklist before she leaves the house:
(2). Life as an Insulin Dependent Diabetic
Do I have enough insulin in my pump to last the remainder of the day? Is my cellphone charged? Does my insulin pump have enough batteries? When is my CGM sensor expiring?
Going through this checklist was a huge lifestyle change when she was diagnosed but has now become a routine part of her day. Before her diagnosis, this type of careful planning wasnt necessary.
I woke up, brushed my teeth, showered, grabbed a snack and my book bag, and ran out the door to go to school. There werent a slew of question marks or decisions in my daily routine.
Leaving the house while managing diabetes is formidable Nichole knows she must be ready for anything. She first packs her essentials snacks to regulate glucose levels and water. In addition, she packs a cell phone charger to make sure she can always access her mobile app, extra batteries for her insulin pump and hand sanitizer. The numbers on her CGM can lag behind capillary glucose levels by about 15 minutes. Therefore, she also packs lancets, or small needles, to be used with a lancing device to draw blood for testing her glucose levels using a monitor and testing strips.
Nicholes essentials that she always packs in her bag.
At all times, Nichole must listen for her CGM alarms, and checks her glucose levels on her mobile app before a meal. Ordering food means considering the impact choices will have on her glucose levels. She asks about portions, sugar content, and other additions made to the food that could impact her glucose levels. Since Nichole isnt often aware of any symptoms of low blood sugar, like so many people living with T1D, her partner is also on alert and reminds her to check her glucose levels. The CGM has a feature that allows her to wirelessly share her glucose levels with her partner, which is a great backup to have on hand. Nicholes partner often calls her if they see a prolonged high or low blood sugar and reminds her to adjust when needed.
After a long day, Nichole picks up her son from daycare and tends to his needs as well as hers. She checks her glucose levels, which may need a carbohydrate adjustment before preparing dinner, and gets her son ready for bed. After putting her son to sleep, she winds down by journaling and setting her high- and low-trend CGM alarm to its loudest setting for when she is asleep. If the alarm goes off at night, Nichole wakes up to make sure her insulin pump is administering the correct amount of insulin. Nighttime is often stressful for those with T1D; some people experience high overnight glucose levels while others fear a drop. This can make getting adequate sleep difficult, resulting in increased stress and fatigue.
Managing a long-term condition such as T1D can be a major source of exhaustion and near-constant worry. Talk therapy has helped Nichole manage her T1D-related stress, but she still hopes for continued change for the community. She dreams that one day there will be no need to count carbs, keep checklists or take insulin. She hopes for a life free of the mental and physiological burdens of managing T1D.
I dream of science helping our bodies function the way they ought to. Just freedom.
(3). Youngjoo Kang et al. Chronic pain: definitions and diagnosis. BMJ 2023;381:e076036
What we need to know
Acknowledging chronic pain as a diagnosis in its own right can help clinicians and patients move on from a mindset of searching for a diagnosis to discussing long term management strategies
Consider non-pain features such as poor sleep, low mood, and reduced physical activity: these can be both a cause and a consequence of chronic primary pain
Consultations where patients feel believed, listened to, and validated can enable a therapeutic relationship that forms the basis for subsequent management strategies, including supported self-management.
Pain related diseases are the leading cause of disability and disease burden worldwide. Chronic pain affects between a third and half of the population globally, and high impact chronic paindefined as pain experienced on most days or every day in the previous three months that causes restriction in at least one activityhas been found to affect 4.8% of the US adult population. Furthermore, chronic pain is a common reason for accessing healthcare, with 22-50% of GP consultations being related to pain. Patients often report a delay in diagnosis,with a longer and more difficult journey to diagnosis being associated with reduced satisfaction with subsequent treatment.
A lack of diagnostic biomarkers and universally effective treatment options for chronic pain often result in frustration for both patients and clinicians.Consultations can sometimes focus on how to treat pain, without first naming the diagnosis of chronic pain. Creating space in the consultation for this can help patients to feel heard, reduce frustration, and refocus on supported self-management strategies rather than the clinician striving to fix the problem
(4). Rohit Loomba et al. Randomized, Controlled Trial of the FGF21 Analogue Pegozafermin in NASH. 2023.
Background
Pegozafermin is a long-acting glycopegylated (pegylated with the use of site-specific glycosyltransferases) fibroblast growth factor 21 (FGF21) analogue in development for the treatment of nonalcoholic steatohepatitis (NASH) and severe hypertriglyceridemia. The efficacy and safety of pegozafermin in patients with biopsy-proven noncirrhotic NASH are not well established.
Methods
In this phase 2b, multicenter, double-blind, 24-week, randomized, placebo-controlled trial, we randomly assigned patients with biopsy-confirmed NASH and stage F2 or F3 (moderate or severe) fibrosis to receive subcutaneous pegozafermin at a dose of 15 mg or 30 mg weekly or 44 mg once every 2 weeks or placebo weekly or every 2 weeks. The two primary end points were an improvement in fibrosis (defined as reduction by ≥1 stage, on a scale from 0 to 4, with higher stages indicating greater severity), with no worsening of NASH, at 24 weeks and NASH resolution without worsening of fibrosis at 24 weeks. Safety was also assessed.
Results
Among the 222 patients who underwent randomization, 219 received pegozafermin or placebo. The percentage of patients who met the criteria for fibrosis improvement was 7% in the pooled placebo group, 22% in the 15-mg pegozafermin group (difference vs. placebo, 14 percentage points; 95% confidence interval [CI], 9 to 38), 26% in the 30-mg pegozafermin group (difference, 19 percentage points; 95% CI, 5 to 32; P=0.009), and 27% in the 44-mg pegozafermin group (difference, 20 percentage points; 95% CI, 5 to 35; P=0.008). The percentage of patients who met the criteria for NASH resolution was 2% in the placebo group, 37% in the 15-mg pegozafermin group (difference vs. placebo, 35 percentage points; 95% CI, 10 to 59), 23% in the 30-mg pegozafermin group (difference, 21 percentage points; 95% CI, 9 to 33), and 26% in the 44-mg pegozafermin group (difference, 24 percentage points; 95% CI, 10 to 37). The most common adverse events associated with pegozafermin therapy were nausea and diarrhea.
Conclusions
In this phase 2b trial, treatment with pegozafermin led to improvements in fibrosis. These results support the advancement of pegozafermin into phase 3 development.
(5). Muhammad M Mohiuddin et al. Graft dysfunction in compassionate use of genetically engineered pig-to-human cardiac xenotransplantation: a case report. 2023.
Background
A genetically engineered pig cardiac xenotransplantation was done on Jan 7, 2022, in a non-ambulatory male patient, aged 57 years, with end-stage heart failure, and on veno-arterial extracorporeal membrane oxygenation support, who was ineligible for an allograft. This report details our current understanding of factors important to the xenotransplantation outcome.
Methods
Physiological and biochemical parameters critical for the care of all heart transplant recipients were collected in extensive clinical monitoring in an intensive care unit. To ascertain the cause of xenograft dysfunction, we did extensive immunological and histopathological studies, including electron microscopy and quantification of porcine cytomegalovirus or porcine roseolovirus (PCMV/PRV) in the xenograft, recipient cells, and tissue by DNA PCR and RNA transcription. We performed intravenous immunoglobulin (IVIG) binding to donor cells and single-cell RNA sequencing of peripheral blood mononuclear cells.
Findings
After successful xenotransplantation, the graft functioned well on echocardiography and sustained cardiovascular and other organ systems functions until postoperative day 47 when diastolic heart failure occurred. At postoperative day 50, the endomyocardial biopsy revealed damaged capillaries with interstitial oedema, red cell extravasation, rare thrombotic microangiopathy, and complement deposition. Increased anti-pig xenoantibodies, mainly IgG, were detected after IVIG administration for hypogammaglobulinaemia and during the first plasma exchange. Endomyocardial biopsy on postoperative day 56 showed fibrotic changes consistent with progressive myocardial stiffness. Microbial cell-free DNA testing indicated increasing titres of PCMV/PRV cell-free DNA. Post-mortem single-cell RNA sequencing showed overlapping causes.
Interpretation
Hyperacute rejection was avoided. We identified potential mediators of the observed endothelial injury. First, widespread endothelial injury indicates antibody-mediated rejection. Second, IVIG bound strongly to donor endothelium, possibly causing immune activation. Finally, reactivation and replication of latent PCMV/PRV in the xenograft possibly initiated a damaging inflammatory response. The findings point to specific measures to improve xenotransplant outcomes in the future.
Funding
The University of Maryland School of Medicine, and the University of Maryland Medical Center.
(6). Lu Ma et al. The third Intensive Care Bundle with Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial (INTERACT3): an international, stepped wedge cluster randomised controlled trial. Lancet 2023;402(10395):P27-40.
Background
Early control of elevated blood pressure is the most promising treatment for acute intracerebral haemorrhage. We aimed to establish whether implementing a goal-directed care bundle incorporating protocols for early intensive blood pressure lowering and management algorithms for hyperglycaemia, pyrexia, and abnormal anticoagulation, implemented in a hospital setting, could improve outcomes for patients with acute spontaneous intracerebral haemorrhage.
Methods
We performed a pragmatic, international, multicentre, blinded endpoint, stepped wedge cluster randomised controlled trial at hospitals in nine low-income and middle-income countries (Brazil, China, India, Mexico, Nigeria, Pakistan, Peru, Sri Lanka, and Viet Nam) and one high-income country (Chile). Hospitals were eligible if they had no or inconsistent relevant, disease-specific protocols, and were willing to implement the care bundle to consecutive patients (aged ≥18 years) with imaging-confirmed spontaneous intracerebral haemorrhage presenting within 6 h of the onset of symptoms, had a local champion, and could provide the required study data. Hospitals were centrally randomly allocated using permuted blocks to three sequences of implementation, stratified by country and the projected number of patients to be recruited over the 12 months of the study period. These sequences had four periods that dictated the order in which the hospitals were to switch from the control usual care procedure to the intervention implementation of the care bundle procedure to different clusters of patients in a stepped manner. To avoid contamination, details of the intervention, sequence, and allocation periods were concealed from sites until they had completed the usual care control periods. The care bundle protocol included the early intensive lowering of systolic blood pressure (target <140 mm Hg), strict glucose control (target 6178 mmol/L in those without diabetes and 78100 mmol/L in those with diabetes), antipyrexia treatment (target body temperature ≤375°C), and rapid reversal of warfarin-related anticoagulation (target international normalised ratio <15) within 1 h of treatment, in patients where these variables were abnormal. Analyses were performed according to a modified intention-to-treat population with available outcome data (ie, excluding sites that withdrew during the study). The primary outcome was functional recovery, measured with the modified Rankin scale (mRS; range 0 [no symptoms] to 6 [death]) at 6 months by masked research staff, analysed using proportional ordinal logistic regression to assess the distribution in scores on the mRS, with adjustments for cluster (hospital site), group assignment of cluster per period, and time (6-month periods from Dec 12, 2017). This trial is registered at Clinicaltrials.gov (NCT03209258) and the Chinese Clinical Trial Registry (ChiCTR-IOC-17011787) and is completed.
Findings
Between May 27, 2017, and July 8, 2021, 206 hospitals were assessed for eligibility, of which 144 hospitals in ten countries agreed to join and were randomly assigned in the trial, but 22 hospitals withdrew before starting to enrol patients and another hospital was withdrawn and their data on enrolled patients was deleted because regulatory approval was not obtained. Between Dec 12, 2017, and Dec 31, 2021, 10857 patients were screened but 3821 were excluded. Overall, the modified intention-to-treat population included 7036 patients enrolled at 121 hospitals, with 3221 assigned to the care bundle group and 3815 to the usual care group, with primary outcome data available in 2892 patients in the care bundle group and 3363 patients in the usual care group. The likelihood of a poor functional outcome was lower in the care bundle group (common odds ratio 086; 95% CI 076097; p=0015). The favourable shift in mRS scores in the care bundle group was generally consistent across a range of sensitivity analyses that included additional adjustments for country and patient variables (084; 073097; p=0017), and with different approaches to the use of multiple imputations for missing data. Patients in the care bundle group had fewer serious adverse events than those in the usual care group (160% vs 201%; p=00098).
Interpretation
Implementation of a care bundle protocol for intensive blood pressure lowering and other management algorithms for physiological control within several hours of the onset of symptoms resulted in improved functional outcome for patients with acute intracerebral haemorrhage. Hospitals should incorporate this approach into clinical practice as part of active management for this serious condition.
(7). Wendy C Ziai, et al. Acute spontaneous intracerebral haemorrhage: does a care bundle approach work? The Lancet 2023;402(10395):P2-3.
A care bundle is a small but crucial set of treatments that, when implemented together, can improve outcomes.1 Acute spontaneous intracerebral haemorrhage has few effective treatments and intracerebral haemorrhage-specific recommendations for care bundles.2, 3 In clinical practice, intracerebral haemorrhage is often approached with negativity.4 Moreover, the synergistic benefits of specialised nursing care, neurointensive and neurosurgical care, blood pressure control, reversal of coagulopathy, and other interventions have not been ascertained.5
In The Lancet, Lu Ma and colleagues6 report the results of INTERACT3, a cluster randomised, pragmatic, multicentre, blinded endpoint, stepped wedge controlled trial performed in 144 hospitals in ten predominantly low-income and middle-income countries to investigate the efficacy and safety of a care bundle incorporating early intensive blood pressure lowering and management protocols for hyperglycaemia, pyrexia, and abnormal anticoagulation in patients with intracerebral haemorrhage presenting within 6 h of symptom onset. Notably, the chosen sites had few or inconsistent intracerebral haemorrhage-specific protocols.
This is one of the largest intracerebral haemorrhage clinical trials, with 7036 included patients (3221 patients assigned to the care bundle group and 3815 patients to the usual care group). The mean age was 620 years, 360% were female, and 895% identified as Han Chinese. Hospital sites were randomly assigned into three sequences (with four time periods) with a balanced number of enrolments across sequences and periods. The primary outcome, the likelihood of a poor functional outcome on the modified Rankin scale (mRS) at 6 months, was significantly less likely in the care bundle group (odds ratio 086, 95% CI 076097; p=0015) compared with the usual care group. Serious adverse events were less common in the care bundle group. Secondary outcome results were mixed. However, 6-month mortality, mean overall health utility score, and hospital discharge by day 7 were significantly different between the groups and in favour of the intervention, whereas neurological impairment or death at day 7, death or disability (mRS 36), major disability in survivors (mRS 35), and home residence, all at 6 months, were not significantly different between the groups.
The attribution of benefit to a specific component of care is difficult in cluster trials. The overall benefit of the care bundle was attributed to the strong positive effect observed for blood pressure control. Although participants with alterations in blood pressure, blood glucose, pyrexia, and abnormal anticoagulation all had greater proportions who reached the target in the care bundle group compared with the usual care group, the mean differences in glucose and body temperature over 24 h did not differ significantly and there was no clear difference in time to anticoagulation reversal in the 12% of patients with elevated international normalised ratio at presentation.
Ma and colleagues6 should be congratulated on completing an important clinical trial despite major delays from COVID-19. INTERACT3 is a step forward in showing that a target-directed care bundle protocol for intracerebral haemorrhage can both reduce mortality and improve functional outcomes overall. This study is also the strongest evidence available regarding the implementation of a care bundle at the hospital level. A major unanswered question is whether this approach can decrease the proportion of survivors with long-term severe disability.
Clearly a bundle of care is more than just a set of guidelines and depends on multiple factors beyond the specific interventions: a multidisciplinary approach with patients receiving more frequent neurological and physiological monitoring; patients being in an intensive care unit setting to perform required protocols; and adherence with the bundle. Guidelines describing the benefits of these interventions have long preceded this test of the interventions as a bundle and many intracerebral haemorrhage centres use such guidelines. The so-called ABC bundle for intracerebral haemorrhage (anticoagulation reversal, intensive blood pressure lowering, neurosurgery consultation, and access to an intensive care unit) implemented in the UK reported reduced mortality rates, which were mediated by a reduction in do not resuscitate orders within 24 h and increased admissions to intensive care units, and not by time to anticoagulation reversal or intensive blood pressure lowering.2
In INTERACT3, many different factors might have been at play. The percentage of patients with the early withdrawal of active life support was minimal (<1%), but patient location after hospital admission might have been a bias since intensive care unit admission was 5% higher in the care bundle group than the usual care group, as was the use of intravenous blood pressure lowering treatments on days 27, typically an intensive care unit intervention. Elevated blood pressure affected most patients, although only 32% reached the systolic blood pressure goal of <140 mm Hg within 1 h in the intervention group. Whether the full effect of the bundle is due to blood pressure control alone and could be optimised further awaits future publications addressing mediation analysis and haemorrhage expansion rates. Selection bias is also a limitation, because patients were ineligible if they could not adhere to study treatment and follow-up. However, presentation outside the 6-h enrolment window was the main reason for exclusion (633%), and an impressive 648% of screened patients were enrolled.
The generalisability of these data depends on the organisation of individual-site intracerebral haemorrhage programmes. Considering this from outside a low-income and middle-income country viewpoint, for many high-volume intracerebral haemorrhage treatment centres, the bundle of care strategy already exists in audited guideline-driven intracerebral haemorrhage protocols. The fine tuning of variables such as temporal aspects might be the next step to improving outcomes. Notably, there was substantial heterogeneity in the treatment effect between subgroups split by region and COVID-19 period. Finally, the absence of level 1 evidence for all bundle components might affect acceptance, especially for blood pressure control, where guidelines have differed.6, 7, 8
INTERACT 3 is promising, demonstrating that an intracerebral haemorrhage care bundle focused on physiological control interventions, whether synergistic or not, might promote better outcomes in hospitals where care has not previously optimised sustained interventions. The care bundle has minimal risks of cost and coordination and a high public health effect. This effort is an outstanding example of why less therapeutic negativity and more intervention might benefit survivors of intracerebral haemorrhage.
WCZ is supported by grants from the National Institutes of Neurological Disorders and Stroke for other trials in intracerebral haemorrhage. DFH is supported by grants from the National Institutes of Neurological Disorders and Stroke for other trials in intracerebral haemorrhage. MB declares no competing interests.
(8). Erika Martinelli et al. Angiogenesis inhibition in metastatic colorectal cancer continuum of care. Lancet 2023;402(10395):P4-5.
Current treatment for most patients with metastatic colorectal cancer consists of sequential lines of different systemic therapies, including chemotherapy combinations (5-fluorouracil plus irinotecan or oxaliplatin) with the addition of molecular-targeted drugs, such as anti-angiogenic drugs (independently of the molecular characterisation of the tumour) or anti-epidermal growth factor receptor drugs (for patients whose tumours are wild type for KRAS and NRAS genes). More recently, for the subgroup of patients with high microsatellite instable or mismatch repair deficient tumours (approximately 5% of patients), immune checkpoint inhibitors (pembrolizumab or nivolumab plus ipilimumab) have been shown to be highly effective as first-line or second-line therapies. Furthermore, in patients whose tumours show HER2 gene amplification, BRAFV600E mutation, or KRASG12C mutation, current treatment options also incorporate the corresponding appropriate molecular-targeted drugs.
(9). Sarah S Richardson. The new science of menstruation. Lancet 2023;402(10395):P16.
Ever since Gloria Steinem’s 1978 satirical essay, If Men Could Menstruate, feminists have asked what the world would look like if people did not need to adapt to the norms of those who do not menstruate. Steinem imagined that menstruation would be openly discussed and celebrated. Menstruation is a normal process of development for at least half the world’s population, but it is routinely stigmatised as an unruly pathology requiring medical management, and as a lamentable curse of womanhood. Movements for menstrual equity have begun to challenge these perspectives, calling for policies such as workplace flexibility and tax-free sanitary pads in recognition of the link between menstrual stigma and the maintenance of restrictive gender norms and hierarchies. As the reproductive biologist Kate Clancy shows in Period: The Real Story of Menstruation, these perspectives are also beginning to transform our understanding of the biology of menstruation and fertility.
Clancy’s informed, stereotype-puncturing tale of how menstruation works is a powerful call for a science of women’s menstruation and fertility that expands and multiplies the range of the normal. As we learn about terms and concepts such as brainovary communication, ovarian follicle waves, cervical crypts, and competition between female gametes, Clancy dresses down scientific views of menstruation for their misogyny and negative framing of periods. One zinger of a chapter dismantles the notion of the 28-day cycle, that controlling statistic embedded in birth control pill packs since the 1960s. In clear prose, Clancy explains how the past few decades of research tell a different story, raising questions about this rigid, normative idea of the timing and pacing, as well as usual age of onset, of the so-called typical menstrual cycle. While relating the new science, Clancy maintains an open-minded stance of curiosity, making it evident that the science of menstruation and ovulation is very much still an unfolding one.
Period is an authoritative and broadly accessible analysis of up-to-date science of menstruation and fertility and a scholarly contribution to reproductive biology. At the same time, it is an energising read that models and opens critical conversations about ethically and politically reflective practices in the life sciences. Period joins such transformative feminist classics as Sarah Blaffer Hrdy’s Mother Nature and Natalie Angier’s Woman.
Clancy, who runs a feminist reproductive ecology laboratory at the University of Illinois, Champagne-Urbana, IL, USA, places herself in the text, as a menstruator, as a scientist, as a survivor of sexual harassment in science, as a parent, and as an athlete. Telling her own story as she navigates the challenging scientific and sociopolitical matters that weave through her analysis, Clancy engages the reader in a dialogue that ignites curiosity and invites further inquiry, offering dollop after rich dollop of fascinating science while also reflecting on how science works and on the wider context in which scientific claims influence people’s lives.
Period is not only an exquisite work of science writing, it is a life-altering read. Fierce and unsparing in its call for a better science of menstruation, Period changed my understanding of my own body and radicalised my compassion for my friends and family who have struggled with matters of menstruation and fertility, frequently finding little recognition or affirmation of their experiences from medical practitioners.
Clancy concludes by provoking readers to question technologies of passing that normalise femininity as fitting in to male spaces while minimising one’s differently gendered body. Living in a world dominated by this dualistic, male-centered perspective has disconnected me at key points in my life from the world around me, Clancy writes. I wonder sometimes if some negative symptoms associated with the processes of the menstrual cycle and/or reproduction are in part a response to how out of place we can feel. Of course, as gender systems and reproductive technologies have changed, so too has the embodied, gendered, and sexed experience of menstruation. For example, not too long in the human past, women rarely menstruated during their reproductive lives, as they were frequently lactating or pregnant. Today, many people use contraceptives to suppress menstruation. While from one perspective menstrual suppression may be seen as a passing technology, sustaining negative attitudes about periods, it can be an affirming choice for many, including non-binary and transgender people who have a uterus. Wherever we come down on this debate, all menstruators deserve a rigorous biological understanding of menstruation that allows us to make informed decisions, liberated from ignorance of how our bodies work, and a science of menstruation that is self-aware about the intimate ties between menstruation, the sexual politics of health, and gender equality.
(10). Nadia Sabbah et al. Recurrent vomiting and confusion in pregnancy: hypercalcaemia due to parathyroid adenoma. Lancet 2023;402(10395):P62-63.
A 32-year-old woman, who was 12 weeks pregnant, was referred to our emergency department feeling generally unwell after recurrent vomiting. She had no notable medical history.
On arrival at the hospital, she was mildly confused and reported polyuria. On clinical examination she was unwell and showed signs of dehydration; her pulse was 119 beats per min and her blood pressure was 100/60 mm Hg, and temperature 37°C. An electrocardiogram showed a prolonged PR interval and repolarisation was abnormal.
Laboratory investigations found a serum potassium concentration of 3 mmol/L (normal range 3551) and a serum creatine concentration of 43 μmol/L (normal range 64104); the patient’s thyroid hormone concentrations were normal. Total serum calcium and phosphorus concentrations were 415 mmol/L (normal range 220255) and 102 mmol/L (normal range 0815), respectively; serum parathyroid hormone (PTH) concentration was 992 pg/mL (normal range 650).
We made a working diagnosis of primary hyperparathyroidism presenting as a hypercalcaemic crisis. The patient was rehydrated with a saline infusion of 5 L given over 24 h and an intravenous infusion of calcitonin100 U over 8 hunder cardiac monitoring. After 48 h, as the patient’s serum calcium had reduced to 389 mmol/L, but still above normal range, cinacalcet was added at a dose of 30 mg every 8 h. The clinical condition of the patient improved, but after 72 h, severe hypercalcaemia (340 mmol/L) persisted. Two sessions of dialysis using a low-calcium dialysate transiently lowered the serum calcium level; the patient’s albumin-adjusted serum calcium concentration remained stable at 31 mmol/L, while she was given a saline infusion, calcitonin, and cinacalcet.
A cervical ultrasound showed a 27 mm × 12 mm × 8 mm, highly hypoechoic oval thyroid nodule vascularised in the periphery of the right thyroid lobesuggestive of a malignant lesionwhich we graded 5 on the European Thyroid Imaging Reporting and Data System (figure). No lesions in the usual parathyroid sites were seen. A cervicothoracic CT scan confirmed the intrathyroid lesion and showed no evidence of parathyroid adenoma in the usual or ectopic sites (figure). We did a fine needle aspiration and PTH concentrationmeasured in the evacuated aspiratewas found to be very high (1495 pg/mL), indicative of a parathyroid adenoma. Notably, PTH is normally undetectable in non-parathyroid tissue. Additionally, parathyroid scintigraphy, which would have helped localise the lesion, is currently unavailable in French Guiana. The patient had an emergency operation to remove the intrathyroid lesion (figure). Serum PTH and calcium concentrations reduced from preoperative levels of 1465 pg/mL and 322 mmol/L, respectively to 103 pg/mL and 306 mmol/L intraoperatively, and to 16 pg/mL and 27 mmol/L immediately postoperatively. Histopathological examination of a sample of the excised lesion confirmed a parathyroid adenoma (figure). Postoperatively, the patient’s general condition markedly improved; a fetal ultrasound showed no abnormalities, and the remainder of the patient’s pregnancy was uneventful
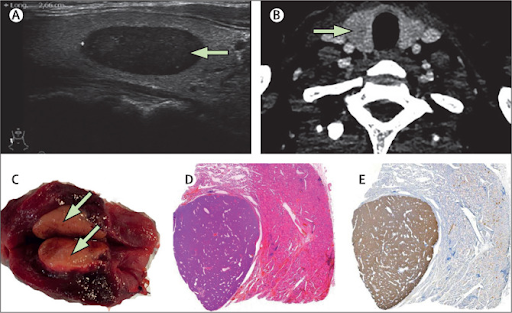
- A cervical ultrasound shows a 27 mm × 12 mm × 8 mm, highly hypoechoic oval thyroid nodule vascularised in the periphery (arrow). (B) Axial CT scan shows a hypodense nodule in the right thyroid lobe (arrow). (C) Photograph shows the parathyroid adenoma after surgical removal. (D) Histopathology of a sample of the parathyroid adenoma shows clear demarcation from typical thyroid tissue by a thin fibrous capsule (haematoxylin and eosin stain). Original magnification ×  5. (E) Immunohistochemical staining of a sample of the parathyroid adenoma shows parathyroid hormone as brown. Original magnification ×  5.
Diagnosing hypercalcaemia during pregnancy can be difficult. Symptomsincluding nausea, vomiting, and fatigueare like those of early pregnancy. Furthermore, long-standing hypercalcaemia may lead to preeclampsia, which in early pregnancy can lead to shortness of breath, tachycardia, and confusion; both mother and child’s needs must be considered during management and treatment. Primary hyperparathyroidism is the commonest cause, and adenomas may be difficult to find. Fine needle aspiration and PTH measurement in the aspirate may be an alternative method of diagnosisparticularly in resource-limited settings.
(11). Patrick OByrne, et al. Rates of sexually transmitted infections are rising. BMJ 2023;381:p1492.
In June 2023, the UK Health Security Agency reported a 23.8% increase in sexually transmitted infection (STI) diagnoses in 2022 compared with 2021,1 including for chlamydia (24.3%), gonorrhoea (50.3%), and syphilis (15.2%). Most of the syphilis infections occurred in men who have sex with men. These increases exceed the 13.4% rise in STI testing in 2022 compared with 2021, indicating true increases in transmission, not better case finding from more testing. Similar trends have emerged in the United Stateswhere the number of syphilis diagnoses rose by 28.6% and gonorrhoea by 4.6% in 2020-21 compared with 20192and in Canada, where rates of syphilis rose by 20% in 2020-21.
This situation is important for a few reasons. Firstly, STIs cause harm, including pelvic inflammatory disease, disseminated gonococcal infection, and neurosyphilis. Secondly, drug resistant gonorrhoea is now being reported internationally, showing the spread of antimicrobial resistance. Thirdly, in Canada and the US, growth in the incidence of syphilis among gay, bi, and queer men is risinhg
(12). Pensée Wu, et al. Hypertensive disorders of pregnancy. BMJ 2023;381:e071653.
Hypertensive disorders of pregnancy (HDP) are one of the most commonly occurring complications of pregnancy and include chronic hypertension, gestational hypertension, and pre-eclampsia. New developments in early pregnancy screening to identify women at high risk for pre-eclampsia combined with targeted aspirin prophylaxis could greatly reduce the number of affected pregnancies. Furthermore, recent advances in the diagnosis of pre-eclampsia, such as placental growth factor based testing, have been shown to improve the identification of those pregnancies at highest risk of severe complications. Evidence from trials has refined the target blood pressure and timing of delivery to manage chronic hypertension and pre-eclampsia with non-severe features, respectively. Importantly, a wealth of epidemiological data now links HDP to future cardiovascular disease and diabetes decades after an affected pregnancy. This review discusses the current guidelines and research data on the prevention, diagnosis, management, and postnatal follow-up of HDP. It also discusses the gap in knowledge regarding the long term risks for cardiovascular disease following HDP and illustrates the importance of improving adherence to postnatal guidelines to monitor hypertension and the need for more research focused on primary prevention of future cardiovascular disease in women identified as being at high risk because of HDP.
(13). Nelsan Pourhad et al. Menopausal hormone therapy and dementia: nationwide, nested case-control study. BMJ 2023;381:e072770.
Objectives: To assess the association between use of menopausal hormone therapy and development of dementia according to type of hormone treatment, duration of use, and age at usage.
Design: Nationwide, nested case-control study.
Setting: Denmark through national registries.
Participants: 5589 incident cases of dementia and 55890 age matched controls were identified between 2000 and 2018 from a population of all Danish women aged 50-60 years in 2000 with no history of dementia or contraindications for use of menopausal hormone therapy.
Main outcome measures: Adjusted hazard ratios with 95% confidence intervals for all cause dementia defined by a first time diagnosis or first time use of dementia specific medication.
Results: Compared with people who had never used treatment, people who had received oestrogen-progestogen therapy had an increased rate of all cause dementia (hazard ratio 1.24 (95% confidence interval 1.17 to 1.33)). Increasing durations of use yielded higher hazard ratios, ranging from 1.21 (1.09 to 1.35) for one year or less of use to 1.74 (1.45 to 2.10) for more than 12 years of use. Oestrogen-progestogen therapy was positively associated with development of dementia for both continuous (1.31 (1.18 to 1.46)) and cyclic (1.24 (1.13 to 1.35)) regimens. Associations persisted in women who received treatment at the age 55 years or younger (1.24 (1.11 to 1.40)). Findings: persisted when restricted to late onset dementia (1.21 (1.12 to 1.30)) and Alzheimers disease (1.22 (1.07 to 1.39)).
Conclusions: Menopausal hormone therapy was positively associated with development of all cause dementia and Alzheimers disease, even in women who received treatment at the age of 55 years or younger. The increased rate of dementia was similar between continuous and cyclic treatment. Further studies are warranted to determine whether these findings represent an actual effect of menopausal hormone therapy on dementia risk, or whether they reflect an underlying predisposition in women in need of these treatments.
(14). Julian Sheather. Water matters: we must end the pollution of our rivers with sewage. BMJ 2023;381:p1481.
eeping open waters clean is a public health and environmental priority, writes Julia
I was born on a houseboat on the upper reaches of the river Thames. Summer was spent in the river. Home from school I would tear off my uniformtorture wearing it in those hot, sunstruck classroomsand hurl myself into the cool water. This was the Seventies. Although the river ran green or brown according to the day, it was clean. Despite the disbelief of onlookers, it was, biologically at least, safe to swim in. My father marvelled at the comparison with the London Thames he knew in the Forties and Fifties: a dead river, little more than a toxic, anaerobic sluice, foul with human and industrial waste. But as a kid I swam in water that trout were rumoured to haunt. It was so obviously progress, such a hands down win for the worldfor the environment, for the liberty of summer, for the joy of being alivethat I took its continuance for granted.
Recently I was walking the river Wandle. It rises in south Croydon and winds its beguiling way to the Thames at Wandsworth. Despite meandering through a deal of exurbia, suburbia, and light industry, it is that rarest of things, a chalk streamthere are only 200 in the world, almost all in southern England. As I edged a new housing development, I saw a pipe leaking effluent into the river. It was awful stuff: ashen, grainy, smothering. Like death itself being dribbled into the water. A few hundred yards downstream, a couple of guys were fishing. Kayaking near Victoria Bridge after a spot of rain, I paddled through a shoal of what Scousers dub Mersey otters, brown and buoyant, fresh from a toilet. And this is just the visible tip of a vast polluting. In 2022 alone, raw sewage was pumped into UK rivers over 800 times a day.1 There is almost no open water in the UK that is biologically safe to swim in. We have turned it toxic.
In a slightly laconic opinion piece on Gov.UK, Chris Witty, along with the Chairs of Ofwat and the Environment Agency, restate public health orthodoxy: One of the greatest public health triumphs of the last 200 years was separating human faeces from drinking water.2 Only vaccination can compete with it for impact. The Thames is not drinking water, accepted, but it is tough to swim ebulliently without taking a little water onboard. And this is where the health threat gets serious. Witty et al again: When bacteria from human faeces (coliforms) are ingested, it increases the risk of significant infections including antibiotic resistant bacteria. Keeping human faeces out of water people might ingest remains a public health priority.
Responsibility for pollution on the current scale, along with the release of viable coliforms into rivers as part of business as usual sewage management rests squarely with the water companies. It looks like their approach has been woefully short term and extractive, prioritising shareholder return and lower bills over public health and the environmental integrity of our open water. But the politics are tricky. Investment in infrastructure is expensive. Absent serious government investment, some of the cost will be passed directly to consumers. Eliminating storm overflows would cost between £350bn and £600bn, hiking household bills by between £569 and £999 a year. It would also be highly disruptive and complex to deliver.3 Open water swimming is stilldespite the best efforts of The Guardiana niche enthusiasm. With the cost-of-living skyrocketing, many consumers are tightly focused on their household bills. Why fret over the cleanliness of water they would not dream of swimming in?
There are inevitableand plausiblecalls to take water back into public ownership. I have some sympathy. The combination of private profit and poisoned public goods is galling. As ever, the degradation of the environment is seen as an externalitynot priced into the costs of the goods we consume. But nationalised industries also have their Achilles heel: inefficiency. If regulation and price controls are effective without nationalisation, this could be sidestepped. Sarah Hendry has an interesting blog over at the LSE that nicely untangles some of the policy issues.4 And if there were any doubt that this is politics, remember there are only two stretches of river in the UK certified to swim in. France has five hundred.
I admit though that my interest in good water is personal, biographical. It started in childhood, but a decade or so ago, slightly mauled by depression, I returned to outdoor swimming. It was an Indian summerlong, still autumn days, mist in the morning, shadows lengthening early afternoon. For me depression is, among other woes, a disorder of temperature. My body and mind start to overheat, gradually broiling in the oven of themselves. That autumn, as September slowly tilted over into October, the cold water began its quiet magic. Joy crept back into the day. I knew I had found a lifelong ally. Then lockdown closed everything, including my local lido. Bereft, I took to cycling to Teddington to get my morning hit of cold water. Dawn dips in the last of the non-tidal Thames. But this is no longer the Thames of my youth. I eye it suspiciously. If its been raining at all, I keep my head upthe water as much threat as restorative. What microscopic menace lurks invisible in its flow?
So I cant help it. When I look at the stark calculus of water policy, at the pros and cons of investment and public ownership, of cost and benefit, something in me refuses. I have skin in this game. Water matters. It is a primary good, just like our healthto which it is linked in a thousand supersubtle ways. And to move beyond public health, beyond the irrefutable science: water is surely originary. It is a mythic substance, foundational to life. And rational as I try to be, I cannot accept a trade-off that poisons our wells, that corrupts the sources, mythological and otherwise. We cannot swim with Mersey otters. We must end the fouling of our water.
(15). Ioannis Gallos et al. Randomized Trial of Early Detection and Treatment of Postpartum Hemorrhage. N Engl J Med 2023;389:11-21.
Background
Delays in the detection or treatment of postpartum hemorrhage can result in complications or death. A blood-collection drape can help provide objective, accurate, and early diagnosis of postpartum hemorrhage, and delayed or inconsistent use of effective interventions may be able to be addressed by a treatment bundle.
Methods
We conducted an international, cluster-randomized trial to assess a multicomponent clinical intervention for postpartum hemorrhage in patients having vaginal delivery. The intervention included a calibrated blood-collection drape for early detection of postpartum hemorrhage and a bundle of first-response treatments (uterine massage, oxytocic drugs, tranexamic acid, intravenous fluids, examination, and escalation), supported by an implementation strategy (intervention group). Hospitals in the control group provided usual care. The primary outcome was a composite of severe postpartum hemorrhage (blood loss, ≥1000 ml), laparotomy for bleeding, or maternal death from bleeding. Key secondary implementation outcomes were the detection of postpartum hemorrhage and adherence to the treatment bundle.
Results
A total of 80 secondary-level hospitals across Kenya, Nigeria, South Africa, and Tanzania, in which 210,132 patients underwent vaginal delivery, were randomly assigned to the intervention group or the usual-care group. Among hospitals and patients with data, a primary-outcome event occurred in 1.6% of the patients in the intervention group, as compared with 4.3% of those in the usual-care group (risk ratio, 0.40; 95% confidence interval [CI], 0.32 to 0.50; P<0.001). Postpartum hemorrhage was detected in 93.1% of the patients in the intervention group and in 51.1% of those in the usual-care group (rate ratio, 1.58; 95% CI, 1.41 to 1.76), and the treatment bundle was used in 91.2% and 19.4%, respectively (rate ratio, 4.94; 95% CI, 3.88 to 6.28).
Conclusions
Early detection of postpartum hemorrhage and use of bundled treatment led to a lower risk of the primary outcome, a composite of severe postpartum hemorrhage, laparotomy for bleeding, or death from bleeding, than usual care among patients having vaginal delivery. (Funded by the Bill and Melinda Gates Foundation)
(16). Heiner Wedemeyer et al. A Phase 3, Randomized Trial of Bulevirtide in Chronic Hepatitis D. N Engl J Med 2023; 389:22-32.
Background
Coinfection with hepatitis D virus (HDV) accelerates the progression of liver disease associated with chronic hepatitis B. Bulevirtide inhibits the entry of HDV into hepatocytes.
Methods
In this ongoing phase 3 trial, patients with chronic hepatitis D, with or without compensated cirrhosis, were randomly assigned, in a 1:1:1 ratio, to receive bulevirtide subcutaneously at 2 mg per day (2-mg group) or 10 mg per day (10-mg group) for 144 weeks or to receive no treatment for 48 weeks followed by bulevirtide subcutaneously at 10 mg per day for 96 weeks (control group). Patients will complete 96 weeks of additional follow-up after the end of treatment. The primary end point was a combined response at week 48 of an undetectable HDV RNA level, or a level that decreased by at least 2 log10 IU per milliliter from baseline, and normalization of the alanine aminotransferase (ALT) level. The key secondary end point was an undetectable HDV RNA level at week 48, in a comparison between the 2-mg group and the 10-mg group.
Results
A total of 49 patients were assigned to the 2-mg group, 50 to the 10-mg group, and 51 to the control group. A primary end-point response occurred in 45% of patients in the 2-mg group, 48% in the 10-mg group, and 2% in the control group (P<0.001 for the comparison of each dose group with the control group). The HDV RNA level at week 48 was undetectable in 12% of patients in the 2-mg group and in 20% in the 10-mg group (P=0.41). The ALT level normalized in 12% of patients in the control group, 51% in the 2-mg group (difference from control, 39 percentage points [95% confidence interval {CI}, 20 to 56]), and 56% in the 10-mg group (difference from control, 44 percentage points [95% CI, 26 to 60]). Loss of hepatitis B virus surface antigen (HBsAg) or an HBsAg level that decreased by at least 1 log10 IU per milliliter did not occur in the bulevirtide groups by week 48. Headache, pruritus, fatigue, eosinophilia, injection-site reactions, upper abdominal pain, arthralgia, and asthenia were more common in the 2-mg and 10-mg groups combined than in the control group. No treatment-related serious adverse events occurred. Dose-dependent increases in bile acid levels were noted in the 2-mg and 10-mg groups.
Conclusions
After 48 weeks of bulevirtide treatment, HDV RNA and ALT levels were reduced in patients with chronic hepatitis D.
(17). Eric Karr et al. Hairy Tongue. N Engl J Med 2023;389:e3.
A 64-year-old man who reported current use of tobacco presented to the primary care clinic with a 2-week history of tongue discoloration. Approximately 21 days before presentation, he had completed a course of clindamycin to treat a periodontal infection. After the tongue discoloration began, a course of fluconazole was prescribed to treat possible oral candidiasis. However, the tongue changes had persisted. He reported no associated dysgeusia or tongue pain. On physical examination, the tongue had elongated filiform papillae and green discoloration. No other oral or dental lesions were noted. A diagnosis of hairy tongue was made. Hairy tongue is a benign condition that involves elongation and discoloration of the filiform papillae on the dorsal aspect of the tongue. Risk factors include smoking, dehydration, poor oral hygiene, and antimicrobial use. Although the tongue discoloration is frequently black in which case it is called black hairy tongue or lingua villosa nigra brown, yellow, or green discoloration is possible, as well. The patient was advised to gently scrub the surface of his tongue with a toothbrush four times daily and was counseled on smoking cessation. At 6-month follow-up, the tongue appearance had returned to normal despite the patient continuing to smoke.

(18). Takashi Ono et al. Corneal Crystalline Deposits in a Patient with Multiple Myeloma. N Engl J Med 2023;389:71.
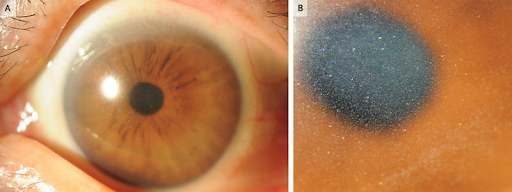
A 66-year-old woman presented to the eye hospital with a 6-month history of photophobia and blurry vision. On physical examination, the visual acuity was 20/25 in the right eye and 20/30 in the left eye. Diffuse corneal clouding by crystalline deposits with multicolored reflectivity was seen in the corneal stroma of both eyes on slit-lamp examination (Panels A and B). The rest of the eye examination was normal. Corneal crystalline deposits may occur in the context of primary ophthalmologic conditions, such as ocular infections or corneal dystrophy, or in the context of systemic diseases, such as cystinosis or paraproteinemias. Owing to concern for an underlying systemic condition, laboratory testing was performed, which showed a new normocytic anemia. The patient was subsequently referred to a hematologist for further evaluation, and IgG kappa multiple myeloma was ultimately diagnosed. A final ophthalmologic diagnosis of corneal immunoglobulin deposition due to multiple myeloma was made. The patient was treated with chemotherapy and autologous hematopoietic stem-cell transplantation. At follow-up 1 year after the transplantation, the corneal clouding had resolved and the patients vision had returned to normal.
(19). Glenn Eastwood, et al. Mild Hypercapnia or Normocapnia after Out-of-Hospital Cardiac Arrest. N Engl J Med 2023; 389:45-57.
Background
Guidelines recommend normocapnia for adults with coma who are resuscitated after out-of-hospital cardiac arrest. However, mild hypercapnia increases cerebral blood flow and may improve neurologic outcomes.
Methods
We randomly assigned adults with coma who had been resuscitated after out-of-hospital cardiac arrest of presumed cardiac or unknown cause and admitted to the intensive care unit (ICU) in a 1:1 ratio to either 24 hours of mild hypercapnia (target partial pressure of arterial carbon dioxide [Paco2], 50 to 55 mm Hg) or normocapnia (target Paco2, 35 to 45 mm Hg). The primary outcome was a favorable neurologic outcome, defined as a score of 5 (indicating lower moderate disability) or higher, as assessed with the use of the Glasgow Outcome ScaleExtended (range, 1 [death] to 8, with higher scores indicating better neurologic outcome) at 6 months. Secondary outcomes included death within 6 months.
Results
A total of 1700 patients from 63 ICUs in 17 countries were recruited, with 847 patients assigned to targeted mild hypercapnia and 853 to targeted normocapnia. A favorable neurologic outcome at 6 months occurred in 332 of 764 patients (43.5%) in the mild hypercapnia group and in 350 of 784 (44.6%) in the normocapnia group (relative risk, 0.98; 95% confidence interval [CI], 0.87 to 1.11; P=0.76). Death within 6 months after randomization occurred in 393 of 816 patients (48.2%) in the mild hypercapnia group and in 382 of 832 (45.9%) in the normocapnia group (relative risk, 1.05; 95% CI, 0.94 to 1.16). The incidence of adverse events did not differ significantly between groups.
Conclusions
In patients with coma who were resuscitated after out-of-hospital cardiac arrest, targeted mild hypercapnia did not lead to better neurologic outcomes at 6 months than targeted normocapnia. (Funded by the National Health and Medical Research Council of Australia)
(20). Daniel Q Huang et al. Type 2 diabetes, hepatic decompensation, and hepatocellular carcinoma in patients with non-alcoholic fatty liver disease: an individual participant-level data meta-analysis. 2023.
Background
Data are scarce regarding the development of hepatic decompensation in patients with non-alcoholic fatty liver disease (NAFLD) with and without type 2 diabetes. We aimed to assess the risk of hepatic decompensation in people with NAFLD with and without type 2 diabetes.
Methods
We did a meta-analysis of individual participant-level data from six cohorts in the USA, Japan, and Turkey. Included participants had magnetic resonance elastography between Feb 27, 2007, and June 4, 2021. Eligible studies included those with liver fibrosis characterisation by magnetic resonance elastography, longitudinal assessment for hepatic decompensation and death, and included adult patients (aged ≥18 years) with NAFLD, for whom data were available regarding the presence of type 2 diabetes at baseline. The primary outcome was hepatic decompensation, defined as ascites, hepatic encephalopathy, or variceal bleeding. The secondary outcome was the development of hepatocellular carcinoma. We used competing risk regression using the Fine and Gray subdistribution hazard ratio (sHR) to compare the likelihood of hepatic decompensation in participants with and without type 2 diabetes. Death without hepatic decompensation was a competing event.
Findings
Data for 2016 participants (736 with type 2 diabetes; 1280 without type 2 diabetes) from six cohorts were included in this analysis. 1074 (53%) of 2016 participants were female with a mean age of 578 years (SD 142) years and BMI of 313 kg/m2 (SD 74). Among 1737 participants (602 with type 2 diabetes and 1135 without type 2 diabetes) with available longitudinal data, 105 participants developed hepatic decompensation over a median follow-up time of 28 years (IQR 1455). Participants with type 2 diabetes had a significantly higher risk of hepatic decompensation at 1 year (337% [95% CI 210511] vs 107% [057186]), 3 years (749% [5361008] vs 292% [192425]), and 5 years (1385% [10431775] vs 395% [267560]) than participants without type 2 diabetes (p<00001). After adjustment for multiple confounders (age, BMI, and race), type 2 diabetes (sHR 215 [95% CI 139334]; p=00006) and glycated haemoglobin (131 [95% CI 110155]; p=00019) were independent predictors of hepatic decompensation. The association between type 2 diabetes and hepatic decompensation remained consistent after adjustment for baseline liver stiffness determined by magnetic resonance elastography. Over a median follow-up of 29 years (IQR 1457), 22 of 1802 participants analysed (18 of 639 with type 2 diabetes and four of 1163 without type 2 diabetes) developed incident hepatocellular carcinoma. The risk of incident hepatocellular carcinoma was higher in those with type 2 diabetes at 1 year (134% [95% CI 064254] vs 009% [001050], 3 years (244% [136405] vs 021% [004073]), and 5 years (368% [218577] vs 044% [011133]) than in those without type 2 diabetes (p<00001). Type 2 diabetes was an independent predictor of hepatocellular carcinoma development (sHR 534 [1671709]; p=00048).
Interpretation
Among people with NAFLD, the presence of type 2 diabetes is associated with a significantly higher risk of hepatic decompensation and hepatocellular carcinoma.
(21). Meletios A Dimopoulos, et al. Management of multiple myeloma-related renal impairment: recommendations from the International Myeloma Working Group. 2023.
Summary
Here, the International Myeloma Working Group (IMWG) updates its clinical practice recommendations for the management of multiple myeloma-related renal impairment on the basis of data published until Dec 31, 2022. All patients with multiple myeloma and renal impairment should have serum creatinine, estimated glomerular filtration rate, and free light chains (FLCs) measurements together with 24-h urine total protein, electrophoresis, and immunofixation. If non-selective proteinuria (mainly albuminuria) or involved serum FLCs value less than 500 mg/L is detected, then a renal biopsy is needed. The IMWG criteria for the definition of renal response should be used. Supportive care and high-dose dexamethasone are required for all patients with myeloma-induced renal impairment. Mechanical approaches do not increase overall survival. Bortezomib-based regimens are the cornerstone of the management of patients with multiple myeloma and renal impairment at diagnosis. New quadruplet and triplet combinations, including proteasome inhibitors, immunomodulatory drugs, and anti-CD38 monoclonal antibodies, improve renal and survival outcomes in both newly diagnosed patients and those with relapsed or refractory disease. Conjugated antibodies, chimeric antigen receptor T-cells, and T-cell engagers are well tolerated and effective in patients with moderate renal impairment.
(22). Howard Libman et al. How Would You Manage A Patient With Recurrent Diverticulitis? 2023.
Abstract
Acute diverticulitis, which refers to inflammation or infection, or both, of a colonic diverticulum, is a common medical condition that may occur repeatedly in some persons. It most often manifests with left-sided abdominal pain, which may be associated with low-grade fever and other gastrointestinal symptoms. Complications may include abscess, fistula formation, perforation, and bowel obstruction. The American College of Physicians recently published practice guidelines on the diagnosis and management of acute diverticulitis, the role of colonoscopy after resolution, and interventions to prevent recurrence of this condition.
Among the recommendations were the use of abdominal computed tomography (CT) scanning in cases where there was diagnostic uncertainty, initial management of uncomplicated cases in the outpatient setting without antibiotics, referral for colonoscopy after an initial episode if not performed recently, and discussion of elective surgery to prevent recurrent disease in patients with complicated diverticulitis or frequent episodes of uncomplicated disease.
(23). Athimalaipet V Ramanan, et al. Baricitinib in juvenile idiopathic arthritis: an international, phase 3, randomised, double-blind, placebo-controlled, withdrawal, efficacy, and safety trial. 2023.
Background
Juvenile idiopathic arthritis can be refractory to some or all treatment regimens, therefore new medications are needed to treat this population. This trial assessed the efficacy and safety of baricitinib, an oral Janus kinase 1/2-selective inhibitor, versus placebo in patients with juvenile idiopathic arthritis.
Methods
This phase 3, randomised, double-blind, placebo-controlled, withdrawal, efficacy, and safety trial was conducted in 75 centres in 20 countries. We enrolled patients (aged 2 to <18 years) with polyarticular juvenile idiopathic arthritis (positive or negative for rheumatoid factor), extended oligoarticular juvenile idiopathic arthritis, enthesitis-related arthritis, or juvenile psoriatic arthritis, and an inadequate response (after ≥12 weeks of treatment) or intolerance to one or more conventional synthetic or biologic disease-modifying antirheumatic drugs (DMARDs). The trial consisted of a 2-week safety and pharmacokinetic period, a 12-week open-label lead-in period (10 weeks for the safety and pharmacokinetic subcohort), and an up to 32-week placebo-controlled double-blind withdrawal period. After age-based dosing was established in the safety and pharmacokinetic period, patients received a once-daily 4 mg adult-equivalent dose of baricitinib (tablets or suspension) in the open-label lead-in period. Patients meeting Juvenile Idiopathic Arthritis-American College of Rheumatology (JIA-ACR) 30 criteria (JIA-ACR30 responders) at the end of the open-label lead-in (week 12) were eligible for random assignment (1:1) to receive placebo or continue receiving baricitinib, and remained in the double-blind withdrawal period until disease flare or up to the end of the double-blind withdrawal period (week 44). Patients and any personnel interacting directly with patients or sites were masked to group assignment. The primary endpoint was time to disease flare during the double-blind withdrawal period and was assessed in the intention-to-treat population of all randomly assigned patients. Safety was assessed in all patients who received at least one dose of baricitinib throughout the three trial periods. For adverse events in the double-blind withdrawal period, exposure-adjusted incidence rates were calculated. The trial was registered on ClinicalTrials.gov, NCT03773978, and is completed.
Findings
Between Dec 17, 2018 and March 3, 2021, 220 patients were enrolled and received at least one dose of baricitinib (152 [69%] girls and 68 [31%] boys; median age 140 years [IQR 120160]). 219 patients received baricitinib in the open-label lead-in period, of whom 163 (74%) had at least a JIA-ACR30 response at week 12 and were randomly assigned to placebo (n=81) or baricitinib (n=82) in the double-blind withdrawal period. Time to disease flare was significantly shorter with placebo versus baricitinib (hazard ratio 0241 [95% CI 01280453], p<00001). Median time to flare was 2714 weeks (95% CI 1529not estimable) in the placebo group, and not evaluable for patients in the baricitinib group (<50% had a flare event). Six (3%) of 220 patients had serious adverse events during the safety and pharmacokinetic period or open-label lead-in period. In the double-blind withdrawal period, serious adverse events were reported in four (5%) of 82 patients (incidence rate [IR] 97 [95% CI 27249] per 100 patient-years at risk) in the baricitinib group and three (4%) of 81 (IR 102 [21297]) in the placebo group. Treatment-emergent infections were reported during the safety and pharmacokinetic or open-label lead-in period in 55 (25%) of 220 patients, and during the double-blind withdrawal period in 31 (38%) of 82 (IR 1021 [95% CI 6931449]) in the baricitinib group and 15 (19%) of 81 (IR 590 [330973]) in the placebo group. Pulmonary embolism was reported as a serious adverse event in one patient (1%; IR 24 [95% CI 01133]) in the baricitinib group in the double-blind withdrawal period, which was judged to be related to study treatment.
Interpretation
Baricitinib was efficacious with an acceptable safety profile in the treatment of polyarticular juvenile idiopathic arthritis, extended oligoarticular juvenile idiopathic arthritis, enthesitis-related arthritis, and juvenile psoriatic arthritis, after inadequate response or intolerance to standard therapy.
(24). Himmatrao S Bawaskar. Research in a rural setting in India. 2023.
I read with great interest the Offline piece about global health by Richard Horton.1 I hope that it is an eye opener to scientists and researchers residing in high-income countries.
In 2022, in Maharashtra, India, it is reported that 2942 farmers died by suicide.2 These suicides have been linked to repeated droughts, untimely rain, excessive debt to money lenders, and a reluctance of the government to guarantee fixed prices for farmers’ goods.
True science cannot be purchased. However, many academic institutions in high-income countries are in a state of privileged seclusion, where money is prioritised over progress. Institutions are often only interested in getting grants and improving their own facilities. For individual scientists, grants and subsidies are only necessary for funding their research goals, whereas Institutions are interested solely in the fees. Too much of researchers time is wasted preparing protocols and applications for getting grants and, ultimately, many scientists lose their passion and interest in the research, which is detrimental to global health.
Between 1978 and 2023, I have published 115 PubMed indexed articles related to 15 various medical health issues in The Lancet, the New England Journal of Medicine, the British Medical Journal, and many other national and international journals.3 In this time, fatality from acute refractory pulmonary oedema caused by scorpion stings has gone from 30% to less than 1%partly as a result of my research into prazosin and scorpion antivenom treatment.4, 5 This uninterrupted research over the past 45 years has been done without help from any funding agency and solely from my own personal income. The most immense satisfaction I have felt in this time was from witnessing a person who had been successfully treated for acute pulmonary oedema being discharged and walking out of my hospital. I remember thinking at the time that, although I am poor in terms of money, I am rich in terms of academic currency.
Sadly, most world authorities from high-income countries will not visit low-income countries unless their travel and accommodation are arranged and expenses covered. I am sure that many of these individuals would not spend a single penny of their own money towards their work in global health.
Working in a rural setting, it is very difficult to be a scientist like myself and make publications in subjects of interest. The biggest challenge that I face is that English is not my first language. Many of the articles that I submit are probably rejected without being properly read. Furthermore, it is discouraging that similar articles are often published soon after by authors from high-income countries. It has been reassuring that several of my Articles and Correspondences have been accepted at The Lancet since 1978.6, 7 The Lancet accepts pieces on the basis of their data and not on the basis of the submission authors nationality, country of residence, or language. Furthermore, I have not been charged for any of these publications.
Even in Open Access journals, some printed articles are not free and submitting authors must pay for publication charges. Many of my articles that are accepted cannot be published because I am unable to pay the publication charges. In the case of private practitioners such as myself, no government or other institute helps with publication.
Nevertheless, I am sure that irrespective of scarce resources, individual passion, sincerity, dedication, and practical research directly applicable to global health will be rewarded.
(25). Sarah McErlean et al. Familial hypercholesterolaemia. BMJ 2023;382:e073280.
What we need to know
Familial hypercholesterolaemia is a common genetic condition affecting 1 in 310 people, resulting in premature coronary artery disease due to elevated cholesterol levels from birth
If a parent has familial hypercholesterolaemia, there is a 50% chance their child will inherit the condition
Treatment is based on lowering low density lipoprotein (LDL) cholesterol concentration, with a target of at least 50% reduction from baseline
Heterozygous familial hypercholesterolaemia is the most common autosomal dominant genetic condition, affecting approximately 1 in 310 people around the world.12 It causes markedly elevated low density lipoprotein (LDL) cholesterol from birth.1234 It has a high penetrance, and elevated LDL cholesterol can begin in utero, with an LDL cholesterol concentration >4mmol/L in children and >5mmol/L in adults suggesting its presence.5
What is familial hypercholesterolaemia?
Familial hypercholesterolaemia is caused by a functional mutation that impairs LDL receptor-mediated uptake of the LDL particle, therefore resulting in higher LDL cholesterol in the bloodstream.67 Most of those affected (85-90%) have a mutation in the LDL receptor gene.68 Familial hypercholesterolaemia can be classified as heterozygous or homozygous depending on the presence of one or two affected gene alleles.9 However, the heterozygous form is common, whereas the homozygous form is very rare.
It is estimated that 25-35 million people worldwide inherit the condition but fewer than 10% are ever diagnosed and most remain untreated.1349 Most studies reporting the prevalence of familial hypercholesterolaemia in the general population are from Europe, North America, East Asia, and Australia, so it is unclear if the same underlying prevalence exists in different parts of the world and among different ethnicities.
(26). Steve Goodacre et al. Diagnosis and management of sepsis in the older adult. BMJ 2023;382:e075585.
What you need to know
Diagnosing sepsis in older adults is difficult, with organ dysfunction often reflecting comorbidities rather than a dysregulated response to infection
The term sepsis should not be used to describe uncomplicated infection and should ideally be limited to cases with organ dysfunction consequent upon a dysregulated host response
Frailty and comorbidities are key determinants of outcome in older adults with sepsis
Management needs to take into account frailty, comorbidities, patient values, and the limited applicability of available evidence and guidelines
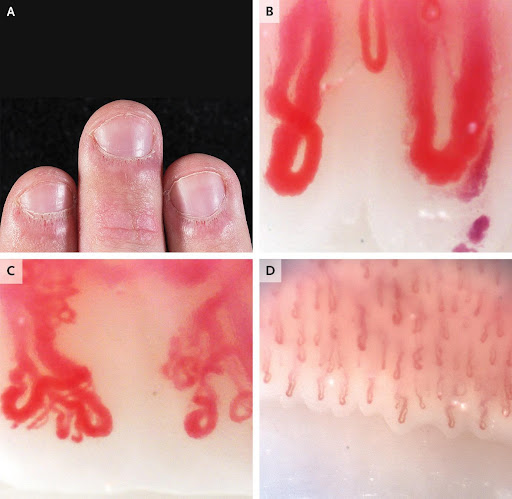
(27). Ashima Makolet al. Nailfold Capillaroscopy in Rheumatic Disease. 2023.
A 19-year-old man presented to the rheumatology clinic with a 3-year history of Raynauds phenomenon and a 1-year history of fatigue, rash on the face and hands, and pain in the finger joints.
On physical examination, there were erythematous plaques on the metacarpophalangeal and interphalangeal joints, without associated synovitis. The nailbeds had periungual erythema, cuticular hypertrophy (also known as ragged cuticles), and prominent dilated capillary loops (Panel A). Erythema was also present on the patients hairline, nasolabial folds, and periorbital region.
The results of strength testing were normal.
Nailfold capillaroscopy was performed. Nailfold capillaroscopy is a bedside assessment of nailbed microcirculation that is performed with the use of a handheld ophthalmoscope, a dermatoscope, a wide-field microscope, or a videocapillaroscopy probe. In this patient, nailfold videocapillaroscopy revealed giant nailfold capillaries with an apical diameter of more than 50 μm (reference value, <15) (Panel B), branched and bushy neovascularized capillary loops (Panel C), and markedly reduced capillary density; for comparison, Panel D shows normal findings on nailfold capillaroscopy.
The patients nailbed findings, in combination with his symptoms, were suggestive of an underlying rheumatic condition.
After serologic evaluation and a skin biopsy, a diagnosis of clinically amyopathic dermatomyositis was made, and the patients symptoms abated after immunosuppressive therapy was initiated.
(28). Ania M. Jastreboff et al. TripleHormone-Receptor Agonist Retatrutide for Obesity A Phase 2 Trial, for the Retatrutide Phase 2 Obesity Trial Investigators. 2023.
Background
Retatrutide (LY3437943) is an agonist of the glucose-dependent insulinotropic polypeptide, glucagon-like peptide 1, and glucagon receptors. Its doseresponse relationships with respect to side effects, safety, and efficacy for the treatment of obesity are not known.
Methods
We conducted a phase 2, double-blind, randomized, placebo-controlled trial involving adults who had a body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) of 30 or higher or who had a BMI of 27 to less than 30 plus at least one weight-related condition. Participants were randomly assigned in a 2:1:1:1:1:2:2 ratio to receive subcutaneous retatrutide (1 mg, 4 mg [initial dose, 2 mg], 4 mg [initial dose, 4 mg], 8 mg [initial dose, 2 mg], 8 mg [initial dose, 4 mg], or 12 mg [initial dose, 2 mg]) or placebo once weekly for 48 weeks. The primary end point was the percentage change in body weight from baseline to 24 weeks. Secondary end points included the percentage change in body weight from baseline to 48 weeks and a weight reduction of 5% or more, 10% or more, or 15% or more. Safety was also assessed.
Results
We enrolled 338 adults, 51.8% of whom were men. The least-squares mean percentage change in body weight at 24 weeks in the retatrutide groups was 7.2% in the 1-mg group, 12.9% in the combined 4-mg group, 17.3% in the combined 8-mg group, and 17.5% in the 12-mg group, as compared with 1.6% in the placebo group. At 48 weeks, the least-squares mean percentage change in the retatrutide groups was 8.7% in the 1-mg group, 17.1% in the combined 4-mg group, 22.8% in the combined 8-mg group, and 24.2% in the 12-mg group, as compared with 2.1% in the placebo group. At 48 weeks, a weight reduction of 5% or more, 10% or more, and 15% or more had occurred in 92%, 75%, and 60%, respectively, of the participants who received 4 mg of retatrutide; 100%, 91%, and 75% of those who received 8 mg; 100%, 93%, and 83% of those who received 12 mg; and 27%, 9%, and 2% of those who received placebo. The most common adverse events in the retatrutide groups were gastrointestinal; these events were dose-related, were mostly mild to moderate in severity, and were partially mitigated with a lower starting dose (2 mg vs. 4 mg). Dose-dependent increases in heart rate peaked at 24 weeks and declined thereafter.
Conclusions
In adults with obesity, retatrutide treatment for 48 weeks resulted in substantial reductions in body weight. (Funded by Eli Lilly)
(29). Christopher J Schwarzbach et al. The structured ambulatory post-stroke care program for outpatient aftercare in patients with ischaemic stroke in Germany (SANO): an open-label, cluster-randomised controlled trial. 2023
Background
Patients with ischaemic stroke are at risk of recurrent stroke. In this study, we aimed to compare the effect of a structured ambulatory post-stroke care programme versus usual care on recurrent vascular events and death and control of cardiovascular risk factors.
Methods
We did a prospective, open-label, cluster-randomised controlled trial (SANO) at stroke centres in regions of Germany. A cluster was defined as a region in which acute stroke care is provided by a participating stroke centre. Patients were eligible for participation if they were aged 18 years or older, had no severe disabilities before the index stroke (modified Rankin scale 01), had at least one modifiable cardiovascular risk factor, and presented within 14 days of symptom onset of their first ischaemic stroke. The participating regions were randomly assigned (1:1) to the intervention and control group (usual care) by the statistician using block randomisation (block sizes of six), stratified by rural and urban regions. In intervention regions, a cross-sectoral multidisciplinary network was established to provide a 1-year organisational and patient-centred intervention. Due to the type of intervention, masking of participants and study physicians was not possible. Endpoint adjudication was performed by an independent endpoint adjudication committee who were masked to cluster allocation. The primary endpoint was a composite of recurrent stroke, myocardial infarction, and all-cause death within 12 months after baseline assessment, assessed in the modified intention-to-treat (mITT) population, which included all patients who did not withdraw consent and completed the primary endpoint assessment at 12 months. This study was registered with the German Clinical Trials Register, DRKS00015322.
Findings
Between Jan 1, 2019 and Dec 22, 2020, 36 clusters were assessed for eligibility, of which 30 were randomly assigned to the intervention group (n=15 clusters) or control group (n=15 clusters). No clusters dropped out of the study. 1203 (86%) of 1396 enrolled patients in the intervention group and 1283 (92%) of 1395 enrolled patients in the control group were included in the mITT population. The primary endpoint was confirmed in 64 (53%) of 1203 patients in the intervention group and 80 (62%) of 1283 patients in the control group (unadjusted odds ratio [OR] 080 [95% CI 049130]; adjusted OR [aOR] 095 [95% CI 054167]). All-cause deaths occurred in 31 (24%) of 1203 patients in the intervention group and 12 (10%) of 1283 patients in the control group. The incidence of serious adverse events was higher in the intervention group (266 [231%] of 1151) than the control group (106 [92%] of 1152). Falls (134 [114%] of 1203 patients in the intervention group; 39 [33%] of 1152 patients in the control group), hypertensive crisis (55 [47%]; 34 [28%]), and diagnosis of depression (51 [43%]; 13 [11%]) were the most frequent adverse events in both groups. No differences were identified in the rate of readmission to hospital between groups.
Interpretation
No differences were identified between patients with ischaemic stroke in the intervention group and control group with regard to the incidence of vascular events 1 year after baseline assessment, despite positive effects with regard to the control of some cardiovascular risk factors. Longer-term effects and other potentially favourable effects on stroke-related sequelae and quality of life require further evaluation.
(30). T Jacob John et al. How to avoid causing polio in the name of its eradication. Lancet 2023;402(10397): P179-180.
WHO began immunising children against polio in low-income and middle-income countries (LMICs) in 1974, through the Expanded Programme on Immunisation, using a trivalent oral poliovirus vaccine (tOPV)three doses during infancy. In 1984, a dose at birth was added.
Polio was not controlled in LMICs despite the four-dose tOPV schedule. Hence, in 1988, WHO proposed, and the World Health Assembly unanimously passed, a resolution to eradicate polio by 2000.1 In our inequitable world, aiming for equity in polio prevention was altruism that inspired everyone, particularly financial donors.
Eradication meant reducing the incidence of polio to zero and interrupting poliovirus transmission, globally.2 Reaching country-level zero polio and zero poliovirus transmission is defined as elimination.2
Before 1988, Sweden, Iceland, Finland, and Norway had eliminated polio using the inactivated poliovirus vaccine (IPV), with three doses during infancy and one or more boosters later.3 Denmark achieved polio elimination using a sequential schedule of IPV followed by the oral poliovirus vaccine (OPV).3 These experiences provided proof of principle and a one-stage, rapid, polio elimination model.
For achieving zero incidence of polio by 2000, the Global Polio Eradication Initiative (GPEI) should have transitioned to the IPV in LMICs and phased out the OPV, since it causes vaccine associated paralytic polio (VAPP) in an occasional vaccinated child or unvaccinated contact.4 Indeed, OPV use is incompatible with polio eradication.
Several countries had achieved zero incidence of polio caused by wild polioviruses using tOPV but had to switch to IPV to avoid VAPP and reach polio elimination. This method was a slow, two-phase polio elimination model. France discontinued OPV in 1988, Germany in 1989, and the USA in 2000, all achieving elimination within 1 year of IPV switch.
Unfortunately, the GPEI could not manage to end wild poliovirus using tOPV because of its well documented suboptimal efficacy in tropical and subtropical LMICs.5 Thus the two-phase model was inapplicable for polio eradication. Only one tactic could eradicate polio: to introduce IPV and when 80% coverage of three doses of IPV is reached, to phase out OPV, country by country. This method required a policy shift in the early 1990s so that the industry could ramp up IPV production.
Continuing use of the OPV beyond 1999, without ensuring protection from polio with IPV, has resulted in: between 8800 and 17 600 children being paralysed by VAPP;6 sporadic polio, caused by vaccine-derived polioviruses types 1, 2, or 3, and polio outbreaks, caused by these circulating viruses, having paralysed nearly 5000 children; and wild poliovirus not yet being eliminated in Afghanistan and Pakistan where a section of society do not trust the OPV, particularly when given in repeated house-to-house campaigns.
Since the future polio-eradicated world can use only the IPV, transition to IPV is the sensible way forward. This policy shift must be announced without delay so that supply, especially of combination vaccines containing IPV, can be expedited. No child is recorded to have developed polio after receiving three doses of IPV during infancy. We appeal to the GPEI, donors, and global opinion leaders, to ensure that no more polio is caused in the name of its eradication. The promised equity must be delivered.

