
Kidney transplantation offers a permanent solution to patients with irreversible kidney failure. Unlike any other surgery where a diseased organ is removed – for example appendix, uterus, etc., or a damaged joint is replaced by an artificial metallic joint, organ transplantation involves transplanting a live organ from a donor to a patient.
We all have an immune system in our body that normally fights against any infections. This is done through the process of identifying foreign proteins that are present in the bacteria or virus that causes the infection. Similarly, when an organ is placed from a donor to the patient, his/her immune system will not differentiate this lifesaving organ from disease-causing bacteria and tends to reject the organ.
In order to make this organ function, patients need to take immune suppressive medications that will enable the organ to function without getting rejected. The extent of these medications depends on genetic matching between the donor and the recipient. The more the matching, the lesser these medications. These medications, by lowering the immune function, predispose the patients to infections wherein the immune system will not fight against and the patients could get into life-threatening complications.
The transplantation is considered to be low-risk when it falls under one of the following categories:
- Performed within close relatives as they have good genetic matching.
- Blood group compatible donors – O blood group donors are universal donors and AB blood group patients are universal recipients. Opposite blood group donors can still donate but the immune suppressive medications’ doses are much higher making them vulnerable to infections.
- Live transplantation compared to organs from a brain-dead victim (cadaveric transplantation).
- First-time transplantations.
- Women are immunologically at higher risk as pregnancy increases the risk of organ rejection.
Case Scenario:
We encountered a strange situation where one of our patients with blood group A needed a transplantation and his wife was the only available donor. But her blood group was B.
Another patient in a similar situation had blood group B and his wife who was the only available donor had blood group A.
At this point, the option available was to do blood group incompatible transplantation for both of them. Though it is possible, it requires both these patients to receive much higher doses of immune suppressive medications and associated risks.
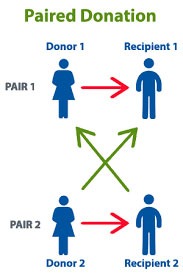
We counselled both families and made them understand the advantages of switching donors. In this situation, both the patients will receive a blood group compatible organ and they could take lesser doses of immune suppressive medications.
After going through the necessary evaluation, they were found to be suitable to donate organs and the transplantations were performed simultaneously six months ago both the patients and the donors are doing well with normal kidney functions.
Swap Transplantation Current Scenario:
SWAP KIDNEY TRANSPLANTATION or PAIRED EXCHANGE PROGRAM is an ideal method where we can do organ transplantation with minimal risk of infectious complications to the recipients. Ideally, any transplant unit should look into their patient and donor profile to see if organs can be swapped.
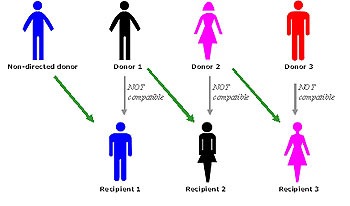
These transplantations are gaining momentum across the world and transplantations beyond two pairs are also being done – DOMINO TRANSPLANTATIONS for multiple technical reasons.

Dr. R. Balasubramaniyam
Chief Nephrologist & Head of Department of Nephrology
Kauvery Hospital Chennai

