Rajeswari P
In charge Dietician, Kauvery Hospital, Salem, India
*Correspondence: +91 88384 13328; E-mail: [email protected]
Nutritional management of patient who underwent emergency laparotomy and GIST
Background
A 72-year-old gentleman was admitted with complaints of hematemesis for 2 days. No comorbidities were present. He initially went to a was nearby hospital and referred here for further management. The doctor assessed the patient and CT scan was taken. Multiphasic CECT abdomen was also taken.
Findings and Plan
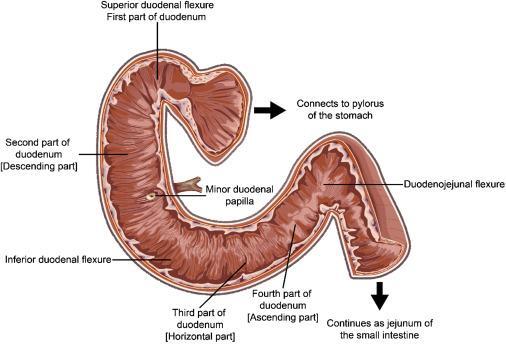
CT report
A well-defined, enhancing lesion with central areas of necrosis measuring 4*3 cm, adjacent to D2 duodenum, partly exophytic lesion from duodenum, compressing on duodenal lumen.
No active vascular contrast leak. Preplaced left hepatic artery from left gastric artery, features suspicious for GIST.
Surgical Plan:
Emergency laparotomy and excision of Gastrointestinal stromal tumour
What is GIST?
A gastrointestinal stromal tumor (GIST) is a type of cancer that begins in the digestive system. GISTs happen most often in the stomach and small intestine. A GIST is a growth of cells that’s thought to form from a special type of nerve cells. These special nerve cells are in the walls of the digestive organs.
Causes/Risk Factors
The only known risk factors for gastrointestinal stromal tumors (GISTs) are − older age and certain rare, inherited genetic syndromes – and cannot be changed. There are no known lifestyle-related or environmental causes of GISTs, so at this time we do not know of any way to protect against these cancers.
Symptoms
- Abdominal (belly) pain.
- A mass or swelling in the abdomen.
- Nausea and vomiting.
- Feeling full after eating only a small amount of food.
- Loss of appetite.
- Weight loss.
- Problems in swallowing (for tumors in the esophagus)
Is it curable?
Most patients with a primary, localized, GIST can be cured with surgery alone. However, if the cancer has spread, you may receive additional modalities of treatment. GISTs most commonly spread to the liver or peritoneum, the a layer of tissue that lines and covers abdominal organ.
| Name | Mr.X |
| Age | 73 years |
| Gender | Male |
| Date of Admission | 08.11.2022 |
| Date of Discharge | 27.11.2022 |
Personal Details
Anthropometric Data
Height: 165cm
Weight: 65kg
BMI: 23.8kg/m2
IBW: [Height(m2) X 24] to [Height(m2) X 27]: 65kg to 73kg
Clinical Data & Diet History
| Complaint | Hematemesis |
| Diagnosis | Gastrointestional stromal tumor |
| Past history | No comorbidities, Loss of appetite & weight loss(6kg in 2 month) |
| Treatment | Emergency laparotomy and excision of Gastrointestional stromal tumor |
| Personal history | Non-alcoholic, Non-smoker, |
| Diet Habit/Allergic | Non vegetarian/Nil |
| Subjective Global Assessment | Healthy Weight |
Biochemical Data
| Date | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 |
| Hb | 3.6 | 8.4 | 7.6 | 9 | 8.1 | 7.5 | 9 | 8.9 | 9.7 | 9.3 | 9.2 | 9.9 | 9.1 | 9.1 | 9.8 | 8.6 | 8.9 | 8.8 | 8.6 |
| PCV | 12.1 | 26 | 24.6 | 28.1 | 24.4 | 29.2 | 27.9 | 30.8 | 29.9 | 32.6 | 30 | 28.8 | 33.4 | 29.6 | 29.3 | ||||
| TC | 12030 | 18190 | 12030 | 9320 | |||||||||||||||
| Platelet | 1.38 | 1.43 | 1.1 | 1.04 | 1.3 | ||||||||||||||
| urea | 97 | 24.7 | |||||||||||||||||
| Creatine | 1.1 | 0.7 | |||||||||||||||||
| Sodium | 141 | 143 | 144 | 138 | |||||||||||||||
| Potassium | 3.8 | 3.4 | 3.8 | 3.4 | |||||||||||||||
| total Bilirubin | 0.4 | ||||||||||||||||||
| Direct | 0.2 | ||||||||||||||||||
| Indirect | 0.2 | ||||||||||||||||||
| SGOT | 26 | ||||||||||||||||||
| SGPT | 15 | ||||||||||||||||||
| GGTP | 8 | ||||||||||||||||||
| Total protein | 3.8 | ||||||||||||||||||
| Albumin | 2.4 | ||||||||||||||||||
| Globulin | 1.4 | ||||||||||||||||||
| BT | 13.3 | ||||||||||||||||||
| CT | 11.3 | ||||||||||||||||||
| PT/INR | 1.18 | ||||||||||||||||||
| Calcium | 7.7 | 7.3 |
Medical Nutritional therapy
- Energy: To provide adequate calories
- Carbohydrates: To provide moderate carbohydrates to prevent protein catabolism
- Protein: Provide for high protein for tissue repair and growth
- Fat: To provide moderate fat
- Fibre: Limit intake of fibre.
- Fluids: To provide adequate fluid to maintain the hydration.
- Micro nutrient as per WHO recommendations
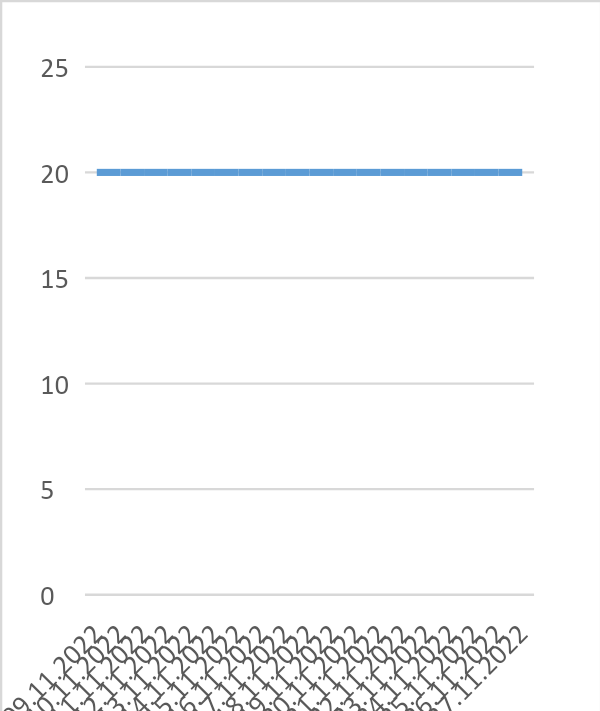
Post operative nutrition target
- Energy: 2800Kcal
- Protein: 1.8 gm/Kg of IBW(117gm)
- CHO: 60% of total Calories
- Fat: 20% of total calories
- Salt: Based on Sodium level
Diet Followup
| Day | Date | Type of Diet | Energy | Protein | Remarks |
| Day 1 | 09.11.2022 | NPO | |||
| Day 2 | 10.11.2022 | NPO | |||
| Day 3 | 11.11.2022 | NPO | |||
| Day 4 | 12.11.2022 | NPO(DNS-500ml/Day) | |||
| Day 5 | 13.11.2022 | FJ feed 1500ml/Day (60ml/hr) | 1500Kcal | 50gm | Feed start at 6.00am |
| Day 6 | 14.11.2022 | FJ feed 2500ml/Day (100ml/hr) | 2100Kcal | 80gm | No complaint |
| Day 7 | 15.11.2022 | FJ feed 2500ml/Day (100ml/hr) | 2100Kcal | 80gm | No complaint |
| Day 8 | 16.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Oral plain water 30ml/hr | 2100Kcal | 80gm | Oral Plain water start.No complaint |
| Day 9 | 17.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Oral liquid 50ml/ hr | 2100Kcal+300(2400) | 80gm+18gm | Oral liquid diet start 8.00am. Complaint of Gastritis at 12.30pm. |
| Day 10 | 18.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Semisolid diet | 2100Kcal+280(2380) | 80gm+15gm | Semisolid start at 9.00am. |
| Day 11 | 19.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Semisolid diet | 2100Kcal+450(2550) | 80gm+22gm | Oral intake was poor so FJ feed continue |
| Day 12 | 20.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Soft diet | 2100Kcal+530(2630) | 80gm+26gm | Oral intake not taken adequately. FJ feed continued. |
| Day 13 | 21.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Soft diet | 2100Kcal+430(2530) | 80gm+20gm | Oral intake not taken adequately . FJ feed continued. |
| Day 14 | 22.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Soft diet | 2100Kcal+510(2610) | 80gm+23gm | Oral intake not taken adequately. FJ feed continued. |
| Day 15 | 23.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Soft diet | 2100Kcal+600(2700) | 80gm+30gm | Oral intake not taken adequately. FJ feed continued. |
| Day 16 | 24.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Soft diet | 2100Kcal+550(2650) | 80gm+27gm | Oral intake not taken adequately. FJ feed continued. |
| Day 17 | 25.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Soft diet | 2100Kcal+420(2520) | 80gm+20gm | Oral intake not taken adequately. FJ feed continued. |
| Day 18 | 26.11.2022 | FJ feed 3000ml/Day (125ml/hr) + Soft diet | 2100Kcal+630(2730) | 80gm+33gm | Oral intake not taken adequately. FJ feed continued. |
| Day 19 | 27.11.2022 | FJ feed 3000ml/Day(125ml/hr)+ Soft diet | 2100Kcal+625(2725) | 80gm+33gm | Oral intake not taken adequately. FJ feed continued. |
Discharge Advice
Target Nutrition achieved.FJ feed continue 125ml/hr continued. High protein diet (oral encourage) advice. Patient is on regular follow-up.

Rajeswari P
In-charge Dietician

