Care of patient with Interstitial Lung Disease
Roseline
Deputy Nursing Superintendent, Kauvery Hospital, Vadapalani
Abstract
Interstitial lung diseases (ILD) is a group of disorders that cause progressive scarring of lung tissue, caused by long-term exposure to hazardous materials, such as asbestos or coal dust. It can also be caused by an autoimmune disease such as rheumatoid arthritis. Smoking and exposure to droppings of pigeons are other causes. Once lung scarring occurs, it’s generally irreversible. Symptoms include a dry cough and shortness of breath that can occur either at rest or after exertion. Treatment depends on the underlying cause but often includes steroids. For people with the most severe and rapidly worsening forms of interstitial lung disease, life expectancy is around 3 – 5 years after diagnosis. This article explains about the patient with ILD who underwent lung transplant.
Case presentation
A 41-years aged gentleman was admitted on 11 Dec 2023 at Kauvery hospital, Alwarpet. He was a known to have Interstitial Lung disease, Rheumatoid arthritis and peripheral neuropathy. He was admitted elsewhere with worsening oxygen requirement and was referred here for lung transplantation.
In view of respiratory failure, he was electively intubated on 06.11.2023. Family was counseled for V-VECMO and tracheostomy. On 09.11.2023, V-V ECMO was initiated & tracheostomy was performed. He was listed for bilateral lung transplant.
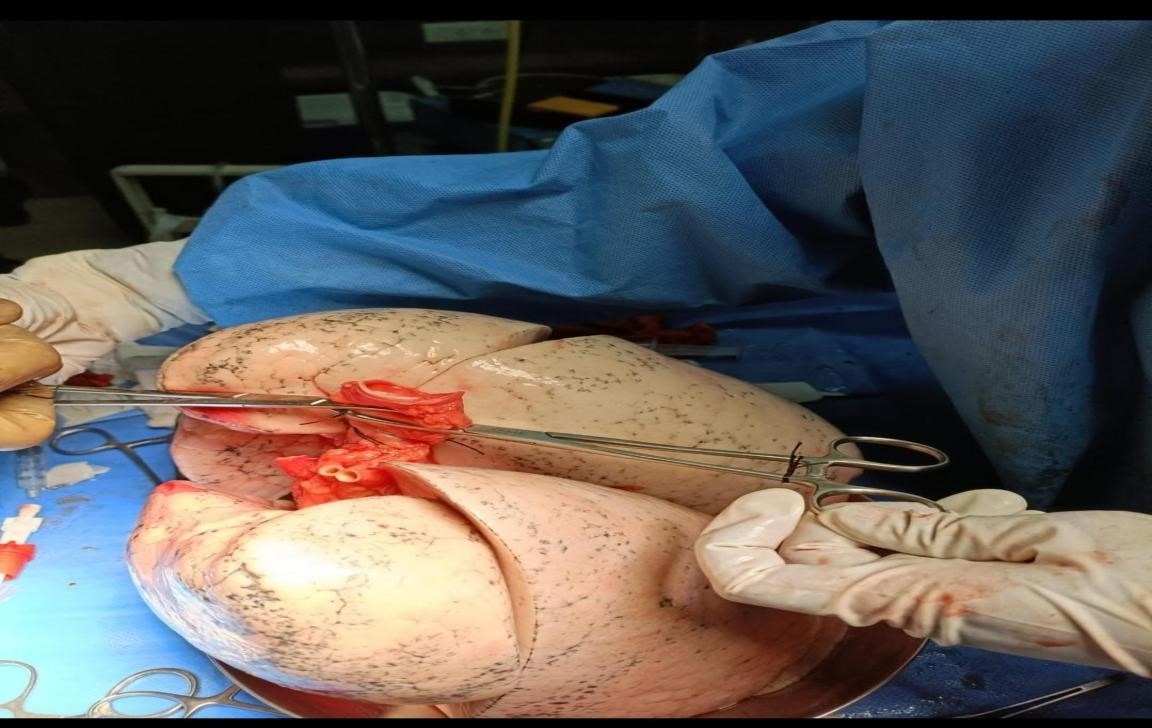
Patient had a matching donor alert call on 14.11.2023 and underwent bilateral sequential lung transplantation on 14.11.2023

Nursing perspective
- Our Transplant ICU nurses meticulously managed the care of patient with utmost care to prevent infection as the patient was shifted to ICU with central V-A ECMO with chest open. ECMO was weaned off and chest closed.
- However, his RV function worsened and hence peripheral V-V ECMO was initiated. He was gradually weaned off ECMO and decannulated on 21.11.2023.
Immunosuppression was started using Tacrolimus, Mycophenolate and Steroids.
Tacrolimus – It is a calcineurin inhibitor used for the prevention of allograft rejection in heart and lung transplant recipients. It is commonly administered orally for long term immunosuppression. In the first month post – transplant, the TAC trough level is maintained between 10-15ng/mL. The TAC trough level reduced to 8-12ng/mL in 2nd and 3rd post-transplant. At the end of 3rd month, the routine TAC trough level is maintained within 5-10ng/mL.
Mycophenolate mofetil (MMF) –It is a inosine monophospate dehydrogenase inhibitor used to prevent the rejection of heart and lung transplants. It depletes guanosine nucleotides preferentially in T and B lymphocytes and inhibits their proliferation, thereby suppressing cell-mediated immune responses and antibody formation.
Steroid (Methylprednisolone)– The primary use of the drug is to suppress inflammatory and immune responses. It achieves this primarily by regulating the number and function of leukocytes, cytokines and chemokines.
- Blood culture grew Klebsiella pneumonia and BAL- Stenotrophomonas maltophilia, Pseudomonas Aeruginosa and Elizabethkingia meningoseptica.
Klebsiella pneumonia
Klebsiella pneumonia is a gram negative, lactose fermenting anaerobic bacteria, found in normal flora of the mouth, skin and intestine. It can cause destructive changes to lungs, specifically to the alveoli resulting in bloody, brownish jelly like sputum. It is sensitivity is limited to Gentamycin, Tigecycline and Colistin.
Stenotrophomonas maltophilia
Stenotrophomonas maltophilia has had multiple different names in the past. It was first found in a pleural effusion in 1943 and given the name Bacterium bookeri. It was then renamed to Pseudomonas maltophilia in 1961. It was moved to the genus Xanthomonas in 1983, and most recently to Stenotrophomonas in 1993
S.maltophilia is an environmental bacterium found in aqueous habitats, including plant rhizospheres, animals, foods, and water sources. Infections of S.maltophilia can occur in a range of organs and tissues; the organism is commonly found in respiratory tract infections.
S.maltophilia are sensitive to co-trimoxazole and ticarcillin, though resistance has been increasing. It is usually susceptible to piperacillin and ceftazidime. Tigecycline is also an effective drug. Polymyxin B may be effective treatment, at least in vitro, though not without frequent adverse effects
Pseudomonas Aeruginosa
- aeruginosa is a multidrug resistant pathogen recognized for its ubiquity, its intrinsically advanced antibiotic resistance mechanisms, and its association with serious illness hospital-acquired infections such as ventilator-associated pneumonia and various sepsis syndromes
According to the World Health Organization P. aeruginosa poses one of the greatest threats to humans in terms of antibiotic resistance.
Due to widespread resistance to many common first-line antibiotics carbapenems, polymyxins, and more recently tigecycline were considered to be the drugs of choice.
Elizabethkingia meningoseptica
Elizabethkingia meningoseptica, a ubiquitous gram-negative aerobic bacillus.
Environmental studies have revealed that the organism can survive in chlorine-treated municipal water supplies, often colonizing sink basins and taps, intubation tubes, humidifiers, incubators for newborns, ice chests and syringes, and has become a potential reservoir for infections in the hospital environment.
This bacterium is usually multi resistant to antibiotics typically prescribed for treating Gram-negative bacterial infections, including extended-spectrum beta-lactam agents (due to production by most strains of two betalactamases: one ESBL and one class B carbapenem-hydrolyzing metallolactamase), aminoglycosides, tetracycline, and chloramphenicol.
Presently ciprofloxacin, minocycline, trimethoprim-sulfamethoxazole, rifampin, and novobiocin are considered good alternatives.
Challenges to Nurses
- Cellulitis
- Surgical wound – Daily dressing with antibacterial ointment and primapore
- Rheumatoid arthritis – Daily active range of motion exercise.
- Septic shock (high grade fever and CO2 retention; he required high inotropes for hemodynamic stability)
Nursing management of Cellulitis
He had cellulitis on both lower and upper limbs requiring.
- Daily sterile dressing with Bactigras (Jelonet- paraffin gauze) and soft roll
- Timely administration of antibiotics
- Elevated foot

Care towards surgical wound
- Daily dressing with betadine solution and betadine ointment done iwith sterile precautions
- Followed the SSI bundle protocol
Nursing role in septic shock
- Monitor hemodynamics
- To provide prophylaxis against DVT and stress ulcers
- Maintain intake/output chart.
- Monitor oxygenation and provide adequate oxygenation
- Administer antibiotics as per the order.
Mobilization of the patient
- Challenging part was mobilization; he was on tracheostomy and had critical illness myopathy.
- Daily exercise of lower and upper limbs was done.
- Motor muscle exercises were encouraged.
- Shifted to chair with tracheostomy and mechanical ventilation
Nutrition improvement:
TPN was initially started and later converted to RT feed
Daily requirement of calories and protein were calculated to achieve the required nutrition
Initially he had continuous vomiting when started oral soft diet. Antiemetic drug administered prior to feed and gradually increased to soft solid diet.
Improvement in-patient
- Cellulitis – Recovered over two months.
- Septic shock – Recovered over three months
- Sinus, Right knee s – Recovered
- Acute kidney Injury – recovered over two months
Outcome of patient
He was gradually weaned off ventilator and BIPAP was initiated.
His bronchoscopy revealed left bronchial stenosis, which necessitated metallic stent.
Discharge was planned with BIPAP support.
He was mobile, self-caring, and hemodynamically stable when discharged in a stable condition.


Ms. Roseline
Deputy Nursing Superintendent

