Ovarian Torsion: A case report and discussion
Vincy Praba. A1*, Kalaiarasi2, Mahalakshmi3
1Staff nurse, Kauvery Hospital, Tennur
2Nursing supervisor, Kauvery Hospital, Tennur
3Nursing Superintendent, Kauvery Hospital, Tennur
Abstract
Idiopathic ovarian torsion is uncommon in adolescents and the incidence is reportedly higher in women aged 20–40 years. Most twisted cysts in adolescent are benign. Ovarian torsion (OT) is the fifth most common gynaecological emergency with a reported prevalence of 2.5–7.4%. This condition is usually associated with reduced venous return from the ovary as a result of stromal oedema, internal haemorrhage, hyper stimulation, or formation of a mass. Ovarian tumours, both benign and malignant, are implicated in 50–60% of cases of torsion. Approximately 17% of cases have been found to occur in pre-menarcheal (or) postmenopausal women. Ovarian torsion is a surgical emergency. It remains one of the most challenging diagnoses in an emergency room. Prompt diagnosis and surgical intervention are keys to good outcomes.
Case presentation
A 21 years’ young girl presented with sudden onset of severe lower abdominal pain radiating to right iliac fossa on first day of her menstrual cycle, that was associated with nausea. The pain was localized and colicky. She reported having had a few similar episodes in the past 1 year, that resolved by taking oral analgesics. She had not sought medical attention for the pain because she believed it was normal, probably related to menstruation, and it usually resolved spontaneously. The patient had no history of diarrhoea, chest pain, giddiness, fever. Her pain score was 10 and she reported that it got worse when she moved. She had no other bowel (or) urinary symptoms.
The patient had no history of abdominal trauma. Her menarche occurred at age of 14 years and her menstrual cycles were regular, every 30 days with 3 days on flow with painful menstruation. She had never taken hormonal contraceptives. She had no other gynaecological symptoms. She had no significant past medical, surgical (or) drug history, nor any relevant family history. She was generally fit and well.
On examination, the patient was conscious and oriented. Temp: 98.4F, PR: 86/min, BP: 110/70mmHg, RR: 20/min, CVS: S1 S2 (+), RS: BAE (+).
An abdominal examination revealed soft tenderness on right iliac fossa. No pelvic examination was performed. CBC was done.
She was initially treated with IVF, IV analgesics.
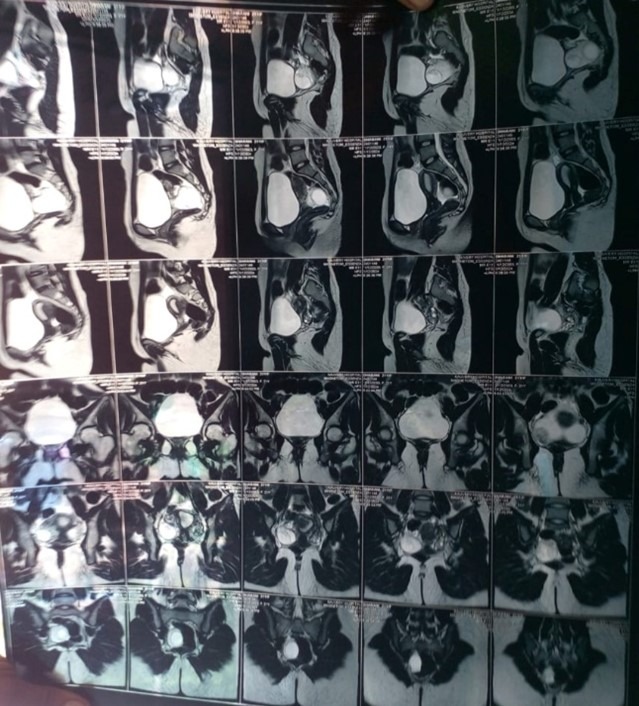
Opinion of Oncology surgeon was obtained. He advised to do USG abdomen & pelvis and MRI Pelvis. An abdominal ultrasound revealed that enlarged right ovary with 2 haemorrhagic cysts, 3.1 x 3.1cm, and minimal free fluid in pelvis) was present.
Right ovarian torsion was diagnosed. An emergency laparoscopy was scheduled. After appropriate pre op evaluation and optimisation she underwent Laparoscopic Ovarian Detorsion with Oophoropexy and Cystectomy, done on 12.01.2024 under general anaesthesia
Procedure :One 10 mm camera port inserted 2-5mm working port inserted Right ovarian detorsion done Right ovary fixed to lateral pelvic wall Cystectomy done and Wash given Port closure with J vicryl skin clips

Health promotion
- Haemodynamic monitoring:
Our team aggressively managed this patient; we monitored the patient by using non-invasive BP, pulse rate and quality, skin temperature and colour, capillary refill time, pulse oximeter and invasive when required.
BP: 120/80mmHg, SpO2: 97% in room air, PR: 94/min, Temp: 98.2 F. Supine
Whenever the patient had any complaints regarding position, we immediately managed. The patient had pain over the surgical site (Pain score 5). analgesics were given.
- Intake and output monitoring
The patient had poor oral intake due to NPO status and also pain. Periodically we monitored intake and output every 2nd hourly to rule out dehydration status
We educated the patient and family members to monitor the amount and colour of urine and watched patient health status such as muscle cramping, lethargy, giddiness, etc. to rule out dehydration (Fluid volume deficit).
- Fluid management
Fluids were administrated through IV at first due to dehydration. IVF NS / RL 100ml per hour to be administered to the patient till clearing their NPO status and after clearance of patient NPO status reduced the IVF NS / RL 75ml per hour.
- Pain management
On PO Day 1, patient had moderate pain (Score – 5). Patient was initially treated with IV analgesics such as Inj. Para 1gm IV TDS, Inj. Tramadol 50mg IV BD and Inj. Ketorolac (Ketorolac Tromethamine) 1ml IV SOS.
- Nutritional support
For any patient to come out of their illness the nutrition part is very important. This patient was prone to develop dehydration. The nurses were focused on patient nutrition, along with doctor’s and dieticians, to avoid nutritional deficiency etc. Our team had taken the challenge and provided good nutrition with adequate calories, protein, fibre rich diet and supported with IV fluids.
Health education
- Medication
Educated the patient and family members regarding taking the medications regularly at correct time. Abdominal (or) pelvic pain is common after surgery but should start to improve within a few days. Advised the patient to continue to use prescribed pain medication as recommended.
- Diet
Constipation is common after surgery. So, we have advised to take high fibre rich and high protein diet for relieving constipation as well as wound healing purpose. Urology surgeon recommended laxatives for constipation
- Activity
- To avoid brisk exercise and lifting more than 10 pounds for 4 – 6 weeks.
- Avoid driving for 2 – 4 weeks (or) longer if still on pain medication.
- To walk as much as she can to persistent complications like blood clots.
- To do deep breathing exercises.
- Wound care
- She should be able to shower 72 hours after your operation.
- Advised the patient to gently wash surgical site and pat them dry with the clean towel afterward.
- To wear clean cloths and avoid wearing of tight inner wear for avoid over compression of surgical site.
- To note for any redness, warmth, swelling (or) abnormal discharge from incision site which would need medical attention as soon as possible.
Psychological support
Our team gave emotional and psychological support to the patients and family members and provided the best communication and coordination with other team members. So, the patient and family members were satisfied and the patient’s health improved and attained positive outcomes.
Conclusion
Patient was discharged in stable conditions. Laparoscopic detorsion of the ovary is the best treatment modality irrespective of the grade of ischemia. Laparoscopic management of adnexal torsion is safe and feasible and facilitates enhanced patient recovery.

Vincy Praba. A
Staff Nurse

Kalaiarasi
Nursing Supervisor

