AAL – Kauvery Advanced Amputation Prevention in Lower Extremity
The unexpected COVID-19 pandemic has made significant changes in the treatment of the diabetic foot. The routine practice of the diabetic limb salvage goals of prevention, preservation & reconstruction and amputation prevention (PPA) are disrupted. The role of plastic surgeons in the management of diabetic foot complications has seen a great surge worldwide. In India, new and younger plastic surgeons are venturing into Diabetic Mellitus Foot (DMF) salvage after being encouraged by excellent results. Wound care and diabetic foot care need a multidisciplinary approach along with high-tech infrastructure and passionate doctors to manage it. ‘KAAL’ has seen phenomenal success in this aspect. In the earlier article titled “When Amputation Is Not an Option’, we shared our determination and the consequent success stories in saving the crushed and mangled lower extremity injuries following road traffic accidents. Our orthopaedic team, vascular team, interventional radiologists, diabetologists, infective disease specialists, ICU and anaesthetic team and plastic & reconstructive surgeons along with dedicated nursing and special wound care staff made this possible. Diabetic foot salvage is done with the same vigour and expertise.

In the first month of the COVID-19 pandemic, we saw the need to reach out to the public in an ever-evolving “new normal”. Diabetic foot treatment had to be streamlined. Patients and doctors had to understand their roles and had to change to tackle situations effectively during the lockdown. With this in mind, a colour coded table was used to make note of the patient’s status at the time of contact. It was useful for the doctors as well as the patients as it helped the patients to self-interpret by looking at their feet at regular or at specific time intervals as advised by the health care worker (HCW) or the doctor taking care of the patient. India has had a complete shutdown and with public transport being shut, even the health care workers were unable to travel.
This modified table is patient-centric and relies only on what the patient knows about himself – his ulcer, the state of his foot, his diabetes level and his organ systems. Symptoms of the COVID-19 pandemic, especially fever and breathlessness, have to be very judiciously and accurately assessed so that the appropriate treatment for the diabetic foot as well as COVID-19 can be instituted early. Nowadays many new patients also seek advice due to non-availability of their own doctor or for a second opinion. In such cases too, the table will be extremely helpful and will aid the doctor and HCW understand the status of the patient. With the addition and availability of home care services, this can be the new normal.
Interpretation of the Table and Discussion with Suitable Examples
The simple colour coded table below not only guides the doctor and the patient on the severity and the urgency but also directs when to get help. It educates the patients on what to look for and be aware of. Patients can also rest assured that help is at hand. Teleconsultations and home help are just a click or a phone call away. Thanks to medical care provided by a dedicated homecare help team, home dressings have been well appreciated by patients.
Let’s see how this table works. You start working from left to right and from top to bottom.
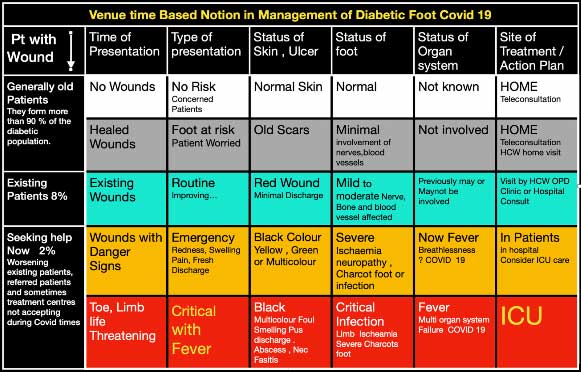

Existing Wounds: Through regular photos sent by WhatsApp, positive progress is appraised. Home dressings and an occasional HCW visit may be needed. Progress is monitored for over 22 days. Patients and relatives are made aware of the classification and signs and symptoms to be observed. A pink/red wound is now well known as a good sign. Following the colour code for observing the nature of the wound and selecting the boxes in the table guides patients and they can check if the wound is getting better or not. A move down the first column raises the red flag of danger and is a sign to seek help soon.

Wounds with Danger signs: These wounds are dynamic and show changes during treatment. Evaluation based on colour changes is very easy and is an important observation made by the patient and the health care team. As mentioned earlier, a red or a pink wound is a healthy wound well on the way to healing. A darkening or black wound or a sudden development of swelling and foul-smelling discharge from the wound is a danger sign. Early and prompt treatment will save the limb. Fever and breathlessness sometimes accompany this picture. COVID-19 has to be suspected.
It needs to be seen if this patient-centric, easy method can be used effectively during and after this pandemic, given the economic fallout of the pandemic. Clinical management and practice post COVID-19 is going to change. Specialties that come up with unique ideas to use technology to empower patients and provide safe care will surge ahead in this new unfolding era.
‘KAAL’ @ Kauvery is well ahead with the multidisciplinary team approach in the ‘new normal’ to not only prevent amputation of diabetic feet but also to educate, rehabilitate and reassure patients that help is available at the click of a button for patients stuck at home during this pandemic.
Article by Prof (Dr) V. B. Narayanamurthy, MBBS FRCS (G)
Sushrutha Professorship in Plastic Surgery
Dr Sathish Manivel
Dr Arul Mozhi Mangai
Staff Nurse Kalpana
Plastic Surgery Team
Kauvery Hospital, Chennai

