Fear of the White Coat
World Hypertension Day – May 17th
Iatrophobia is a condition in which a person may have an extreme fear of doctors and medical tests. The term originated from the Greek word “iatros” which means healer and “phobos” which means fear.
Sometimes a person with iatrophobia may refuse to seek medical attention even when he/she is very sick or is showing signs of severe illness.
What is surprising is that this condition is not so rare!

Although iatrophobia may be at the extreme end of the spectrum, a minimal fear of pricks or needles is definitely a lot more common. One such irrational fear among patients is white coat syndrome, which leads to the well-known ‘white coat hypertension’.
White coat hypertension, more commonly called white coat syndrome, is a form of labile hypertension in which people exhibit an elevation in blood pressure levels in a clinical or hospital setting although they do not exhibit the same in other settings.
Masked hypertension (MH) is a contrasting phenomenon, whereby a patient’s blood pressure is above the normal range during daily living but not in a clinic setting.
What could be the causes of white coat hypertension?
ANXIETY
Whether it’s the tightening of the arm-cuff or the fear of a potential diagnosis, the anxiety brought on by anticipation can be enough to raise your blood pressure. Those who have been diagnosed with generalized anxiety are more likely to suffer from white coat hypertension.
PHOBIA
Your symptoms may be result from a true, honest-to-goodness fear of having your blood pressure taken. Though, if your white coat hypertension is the physical manifestation of a legitimate phobia, the effects will extend beyond the doctor’s office and your experience will be the same every time your blood pressure is taken regardless of the setting.
More About White Coat Hypertension
Hypertension is a condition that is widely prevalent nowadays. As hypertension is a risk factor for cardiovascular disease (CVD), it is imperative that BP levels be monitored and appropriate treatment rendered. To elaborate further, a 20 mm Hg increase or a 10 mm Hg increase in systolic or diastolic pressure respectively, could result in a two-fold increase in the risk of death or CVD.
While it is normal for BP levels to fluctuate during the day, some people show higher BP readings when they are checked by hospital staff (compared to the lower readings they show when they check themselves). If a 24-hour ambulatory blood pressure monitoring confirms this, the person is said to have white coat syndrome.
White coat syndrome can affect both normal patients as well as those with hypertension. Some authors concur that this is due to a neuro-endocrine reflex of the sympathetic nervous system because of the fear of being diagnosed with an illness. While it is agreed that anxiety does play a role in increasing BP levels, anxiety by itself is not thought to be the cause of white coat syndrome.
Identification of white coat hypertension is necessary to avoid uncalled for hypertension treatment.
Is White Coat Hypertension Dangerous?
A new study led by researchers from Penn Medicine, published in the Annals of Internal Medicine, points out two risks that patients with undetected white coat hypertension have – the first is the increase in the probability of a heart disease and the second is the increase in mortality due to heart disease.
The study also proposes that of 5 adults, 1 will possibly have white coat hypertension. The study’s author stresses on the importance of detecting the condition and monitoring the individuals to check if they develop continuous hypertension irrespective of place.
To understand the overall trend of the condition, a study was conducted among 60,000 individuals to find out the risks emanating from white coat hypertension. It was found that when the condition was left untreated, the risk of heart disease and death increased by 36% and 33% respectively while death from heart disease showed an increase of 109%.
Thus, in view of the increased risks, there is a need to check and monitor blood pressure for individuals who have white coat syndrome. For people who are not on medication for white coat syndrome, making changes to their way of life including quitting smoking, alcohol, etc., gains importance. Doctors should refrain from over-medicating patients with white coat syndrome who are already on medicines for hypertension.
Hypertension is closely linked to increased cardiovascular risk and the development of target organ damage (TOD). Therefore, proper clinical follow-up and treatment of hypertensive subjects are mandatory.

Hypertension and White Coat Syndrome
To detect white coat syndrome, the use of ambulatory blood pressure management and home blood pressure monitoring is advised.
The steps for diagnosis of hypertension conditions are represented in the flowchart.
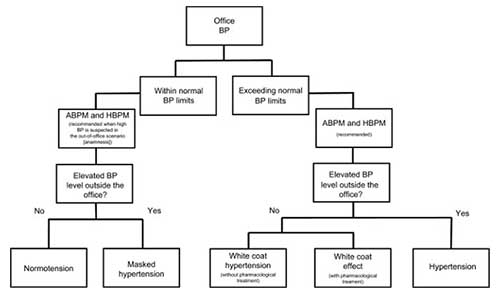
Flowchart of the pathway to diagnosis/classify the white coat syndrome according to the BP levels.
Note: Steps for diagnosis of normotension, hypertension, and phenomena related to white coat syndrome.
Abbreviations: ABPM, ambulatory BP monitoring; BP, blood pressure; HBPM, home BP monitoring.
Role of Ambulatory Monitoring
Blood pressure is characterized by considerable variability. In patients with mild elevation of their office blood pressure on the first visit to a physician, systolic and diastolic blood pressure decrease on average by 15/7 mm Hg by the third visit. Indeed, some patients do not reach a stable blood pressure value until the sixth visit. This reduction in office blood pressure with subsequent visits represents regression to the mean, placebo or nocebo effects, and diminution of the alerting reaction or the fight and flight phenomenon. However, this does not occur in all subjects, leading to the possibility that the phenomenon may be, at least in part, attributable to a conditioning process.
The Task Force of the Eighth International Consensus Conference on Blood Pressure Monitoring recommends ambulatory monitoring to exclude white-coat hypertension in untreated patients when (1) the office blood pressure is ≥140/90 mm Hg on ≥3 separate office visits; (2) ≥2 blood pressure measurements taken outside the office are <140/90 mm Hg, frequently using a home blood pressure monitoring; and (3) there is no evidence of hypertensive target organ damage. For patients with a confirmed daytime ABPM of ≥135/85 mm Hg, physicians may wish to consider starting antihypertensive drug treatment. The recent British National Institute for Health and Clinical Excellence (NICE) guidelines advocate that every person with elevated office blood pressure aged >18 years undergo ABPM to rule out a diagnosis of white-coat hypertension with the potential for savings in health costs by virtue of unnecessary treatment with antihypertensive drugs.
How Do You Overcome White Coat Hypertension?
- Practice relaxation techniques
- Try breathing exercises
- Request a quiet room
- Take a brisk 15–20-minute walk
- Drink a glass of water
- Watch what you eat before your doctor’s visit
- Sleep well before your doctor’s visit
Management
Once ABPM has confirmed the diagnosis of white-coat hypertension, the European Society of Hypertension Working Group on Blood Pressure Monitoring recommends that the diagnosis be reconfirmed in 3 to 6 months and followed up yearly with ambulatory monitoring to detect any evidence of progression to sustained hypertension.


