Journal scan: A review of 25 recent papers of immediate clinical significance, harvested from major international journals
From the desk of the Editor-in-Chief
(1). Amrou Sarraj, et al. Trial of Endovascular Thrombectomy for Large Ischemic Strokes. N Engl J Med. 2023;388:1259-1271.
Background
Trials of the efficacy and safety of endovascular thrombectomy in patients with large ischemic strokes have been carried out in limited populations.
Methods
We performed a prospective, randomized, open-label, adaptive, international trial involving patients with stroke due to occlusion of the internal carotid artery or the first segment of the middle cerebral artery to assess endovascular thrombectomy within 24 hours after onset. Patients had a large ischemic-core volume, defined as an Alberta Stroke Program Early Computed Tomography Score of 3 to 5 (range, 0 to 10, with lower scores indicating larger infarction) or a core volume of at least 50 ml on computed tomography perfusion or diffusion-weighted magnetic resonance imaging. Patients were assigned in a 1:1 ratio to endovascular thrombectomy plus medical care or to medical care alone. The primary outcome was the modified Rankin scale score at 90 days (range, 0 to 6, with higher scores indicating greater disability). Functional independence was a secondary outcome.
Results
The trial was stopped early for efficacy; 178 patients had been assigned to the thrombectomy group and 174 to the medical-care group. The generalized odds ratio for a shift in the distribution of modified Rankin scale scores toward better outcomes in favor of thrombectomy was 1.51 (95% confidence interval [CI], 1.20 to 1.89; P<0.001). A total of 20% of the patients in the thrombectomy group and 7% in the medical-care group had functional independence (relative risk, 2.97; 95% CI, 1.60 to 5.51). Mortality was similar in the two groups. In the thrombectomy group, arterial access-site complications occurred in 5 patients, dissection in 10, cerebral-vessel perforation in 7, and transient vasospasm in 11. Symptomatic intracranial hemorrhage occurred in 1 patient in the thrombectomy group and in 2 in the medical-care group.
Conclusions
Among patients with large ischemic strokes, endovascular thrombectomy resulted in better functional outcomes than medical care but was associated with vascular complications. Cerebral hemorrhages were infrequent in both groups
(2). Xiaochuan Huo, et al. Trial of Endovascular Therapy for Acute Ischemic Stroke with Large Infarct. N Engl J Med 2023; 388:1272-1283.
Background
The role of endovascular therapy for acute stroke with a large infarction has not been extensively studied in differing populations.
Methods
We conducted a multicenter, prospective, open-label, randomized trial in China involving patients with acute large-vessel occlusion in the anterior circulation and an Alberta Stroke Program Early Computed Tomography Score of 3 to 5 (range, 0 to 10, with lower values indicating larger infarction) or an infarct-core volume of 70 to 100 ml. Patients were randomly assigned in a 1:1 ratio within 24 hours from the time they were last known to be well to undergo endovascular therapy and receive medical management or to receive medical management alone. The primary outcome was the score on the modified Rankin scale at 90 days (scores range from 0 to 6, with higher scores indicating greater disability), and the primary objective was to determine whether a shift in the distribution of the scores on the modified Rankin scale at 90 days had occurred between the two groups. Secondary outcomes included scores of 0 to 2 and 0 to 3 on the modified Rankin scale. The primary safety outcome was symptomatic intracranial hemorrhage within 48 hours after randomization.
Results
A total of 456 patients were enrolled; 231 were assigned to the endovascular-therapy group and 225 to the medical-management group. Approximately 28% of the patients in both groups received intravenous thrombolysis. The trial was stopped early owing to the efficacy of endovascular therapy after the second interim analysis. At 90 days, a shift in the distribution of scores on the modified Rankin scale toward better outcomes was observed in favor of endovascular therapy over medical management alone (generalized odds ratio, 1.37; 95% confidence interval, 1.11 to 1.69; P=0.004). Symptomatic intracranial hemorrhage occurred in 14 of 230 patients (6.1%) in the endovascular-therapy group and in 6 of 225 patients (2.7%) in the medical-management group; any intracranial hemorrhage occurred in 113 (49.1%) and 39 (17.3%), respectively. Results for the secondary outcomes generally supported those of the primary analysis.
Conclusions
In a trial conducted in China, patients with large cerebral infarctions had better outcomes with endovascular therapy administered within 24 hours than with medical management alone but had more intracranial hemorrhage
(3). Elisabeth Mahase. Unexplained hepatitis in children may be linked to adeno associated virus 2, studies find. BMJ 2023;381:793
Outbreaks of unexplained hepatitis in children that began in 2022 have been linked to adeno associated virus 2 (AAV2) in three studies looking at cases in the UK and the US.
The mysterious cases of non-A to E hepatitis were first flagged in April 2022 in Scotland,1 and by July 2022 the World Health Organization had registered more than 1010 probable cases across 35 countries.2 As of July 2022, 15 cases in the UK had received a liver transplant and no deaths had been recorded.
All three studies, published in Nature under its accelerated article preview system, found that AAV2 was detected in nearly all the cases of unexplained hepatitis and that many of the children also had signs of infection with a helper virus, such as human adenovirus or herpesviruses.
(4). Carolina M Perdomo et al. Contemporary medical, device, and surgical therapies for obesity in adults. 2023.
Summary
The goal of obesity management is to improve health. Sustained weight loss of more than 10% overall bodyweight improves many of the complications associated with obesity (eg, prevention and control of type 2 diabetes, hypertension, fatty liver disease, and obstructive sleep apnoea), as well as quality of life. Maintenance of weight loss is the major challenge of obesity management. Like all chronic diseases, managing obesity requires a long-term, multimodal approach, taking into account each individual’s treatment goals, and the benefit and risk of different therapies. In conjunction with lifestyle interventions, anti-obesity medications and bariatric surgery improve the maintenance of weight loss and associated health gains. Most available anti-obesity medications act on central appetite pathways to reduce hunger and food reward. In the past 5 years, therapeutic advances have seen the development of targeted treatments for monogenic obesities and a new generation of anti-obesity medications. These highly effective anti-obesity medications are associated with weight losses of more than 10% of overall bodyweight in more than two-thirds of clinical trial participants. Long-term data on safety, efficacy, and cardiovascular outcomes are awaited. Long-term studies have shown that bariatric surgical procedures typically lead to a durable weight loss of 25% and rapid, sustained improvements in complications of obesity, although they have not yet been compared with new-generation highly effective anti-obesity medications. Further work is required to determine optimal patient-specific treatment strategies, including combinations of lifestyle interventions, anti-obesity medications, endoscopic and bariatric surgical procedures, and to ensure equitable access to effective treatments.
(5). Olaparib: Drug to treat inherited cancers offered on NHS in England and Wales
https://www.bbc.com/news/health-65188865
The drug olaparib is designed to treat specific cancers linked to faulty versions of genes known as BRCAs.
How does olaparib work?
Olaparib works by blocking an enzyme that helps cells repair damaged DNA, thereby preventing cancer cells from growing and spreading while leaving healthy cells intact.
The medicine helps patients with breast cancer due to inherited gene faults (BRCA1 or BRCA2 are the most common), which can be tested for quite easily.
Around 5% of women with breast cancer carry these altered genes
It then targets that particular weakness and improves someone’s chances of surviving breast cancer or extends their life with prostate cancer in a way that has not been possible before.
NICE, the National Institute for Health and Care Excellence, said a deal had been struck between NHS England and manufacturer AstraZeneca to allow the drug to be offered
- to adults with HER2-negative, high-risk early breast cancer who have inherited faults in their BRCA1 or BRCA2 genes, after surgery and chemotherapy
- people with previously treated hormone-relapsed metastatic prostate cancer who have the same BRCA mutations
Olaparib has already been available on the NHS in England and Wales for women with advanced ovarian cancer, caused by the same faulty genes.
There are 55,000 new cases of breast cancer in the UK each year, and the disease kills 1,500 women annually.
Prostate cancer is the most common cancer in men, with 52,000 new diagnoses and 12,000 deaths each year.
In trials, 82.7% of people having olaparib after chemotherapy and surgery were alive and free of breast cancer after four years, compared with 75.4% with a dummy drug.
Trials in patients with advanced prostate cancer showed the drug could increase how long people lived if given instead of, or in addition to, current standard treatments.
(6). Image Challenge, NEJM 2023
An 87-year-old man with chronic kidney disease, hypertension, and atrial fibrillation presented to the emergency department with a 3-day history of constipation and lower abdominal pain. Physical examination was notable for abdominal distention and tenderness to palpation of the right lower quadrant without rebound or guarding. A plain radiograph of the abdomen is shown. What is the most likely diagnosis?
The plain radiograph of the abdomen showed an air-filled loop of large bowel resembling a coffee bean, a finding that may be seen in cecal or sigmoid volvulus. Computed tomography of the abdomen was not available at the remote island hospital to which the patient presented. He was taken urgently to the operating room, and a cecal volvulus without signs of bowel compromise was identified and successfully detorsed. Owing to intraoperative hemodynamic instability, a cecopexy and cecostomy were performed rather than an ileocecectomy or right colectomy. The patient’s postoperative course was uncomplicated. At 6 months of follow-up, he was doing well and declined ostomy reversal at that time.
(7). Gerald W. Smetana et al. How Would You Manage This Patient With Benign Prostatic Hyperplasia?
Abstract
Lower urinary tract symptoms due to benign prostatic hyperplasia (BPH) are common in older patients assigned male sex at birth, regardless of gender identity, and treatment of these symptoms is therefore common in primary care practice. In 2021, the American Urological Association published guidelines for management of BPH. They recommend using a standardized scoring system such as the International Prostate Symptom Score to help establish a diagnosis and to monitor the efficacy of interventions, α-blockers as the first-choice pharmacotherapy option, and 5α-reductase inhibitors for patients with prostate size estimated to be at least 30 cc. Tadalafil is another option regardless of erectile dysfunction. Combination therapies with α-blockers and 5α-reductase inhibitors, anticholinergic agents, or β3-agonists are effective options. A surgical referral is warranted if the BPH results in chronic kidney disease, refractory urinary retention, or recurrent urinary tract infections; if there is concern for bladder or prostate cancer; or if symptoms do not respond to medical therapy.
(8). Rixecker TM, et al. Daratumumab for a Patient With Refractory Antineutrophil Cytoplasmatic Antibody-Associated Vasculitis. JAMA Intern Med. 2023.
Antineutrophil cytoplasmatic antibody (ANCA)-associated vasculitis (AAV) is characterized by multisystem organ involvement with necrotizing granulomatous inflammation and vasculitis.1 ANCA antibodies are considered both specific and pathogenic for this group of autoimmune diseases.2 Hence, B-cell depletion by anti-CD20 therapy has shown substantial benefit and is now considered the standard of care.3 Some patients, however, do not respond to conventional therapy and require additional treatment options.Long-lived plasma cells are not affected by usual immunosuppressive therapies and have been shown to maintain ANCA production, thereby leading to ongoing autoimmune inflammation.4 Daratumumab (Darzalex; Janssen Biotech) is a monoclonal antibody that binds to CD38, which is highly expressed on long-lived plasma cells and overexpressed on multiple myeloma cells. Targeting CD38 with daratumumab has been shown to benefit patients with multiple myeloma.5 Daratumumab has also been used to treat patients with systemic lupus erythematosus.6 We report the case of a patient with AAV and severe pulmonary and cutaneous involvement who received conventional therapy that failed and who then recovered following daratumumab therapy.MethodsThis case took place in 2022 at the Saarland University Medical Center, Homburg, Germany. The male patient was in his late 20s and initially presented with a cutaneous ulceration on his right foot and upper lobe predominant, centrilobular consolidations. Positive anti-proteinase 3 (PR3) ANCA titers were documented. Histological examination of a tissue sample obtained from his foot revealed granulomatosis with polyangiitis (GPA). Kidney involvement was not apparent during the entire course of his disease. Despite intensive immunosuppression, including both rituximab (3 applications at 375 mg/m2) and cyclophosphamide (3 intravenous applications at 750 mg/m2 followed by 4 mg/kg/d of continuous oral therapy) induction regimens, therapeutic plasma exchange (11 treatments at 60 mL/kg of albumin replacement by means of filter separation), 6 pulses of methylprednisolone (1000 mg each), prednisolone maintenance (1 mg/kg/d), and avacopan (30 mg twice daily), clinical disease activity progressed unimpeded. Sixty-seven days after hospital admission, he finally required extracorporeal membrane oxygenation (ECMO) due to bronchoscopy-proven diffuse alveolar hemorrhage. Because of the continuing presence of positive PR3 ANCAs in this situation, we administered daratumumab in the light of its effectiveness for patients with systemic lupus erythematosus.Daratumumab was administered according to protocols approved for multiple myeloma.5 The patient’s representative provided written informed consent for the off-label use of daratumumab. The procedure was performed according to the Good Clinical Practice guidelines. A commercial sponsor was not involved. Due to the retrospective nature of this analysis and anonymized clinical data, ethical approval was waived by the institutional review board of Saarland University Medical School.ResultsDaratumumab (16 mg/kg infusions once a week) was initiated 3 days after the patient started ECMO therapy. Figure 1 shows the evolution of his pulmonary and cutaneous disease manifestations after adding daratumumab to oral cyclophosphamide, prednisolone, and avacopan. Figure 2 shows an overview of his treatment, his respiratory support, and ANCA titer from the time of hospital admission to hospital discharge. Eleven days after the patient received daratumumab, his ANCA titer became negative for the first time throughout his entire treatment course. With continuation of daratumumab, oral cyclophosphamide, and prednisolone tapering, he could successfully be weaned from ECMO and respiratory support. On September 6, 2022, hospital day 120 and 50 days after starting daratumumab, the patient was sent home without supplemental oxygen and with a healing wound on his foot; cyclophosphamide and avacopan were discontinued. Daratumumab (16 mg/kg infusions every 4 weeks) and prednisolone (last with 10 mg/d) were continued. As of January 2023, the patient remained in remission.DiscussionIn AAV, the ANCAs are believed to contribute to the pathogenesis of the disease.2 If those autoantibodies are produced by long-lived plasma cells, the immunosuppressive therapies for AAV that are usually administered may be ineffective. A limitation of this case report is that the patient could have improved due to the cumulative intensive immunosuppressive therapy that he received and not specifically because of treatment with daratumumab. Nonetheless, the clinical course and apparent response to daratumumab suggest that therapies targeting CD38 should be further studied for patients with severe refractory pulmonary and cutaneous AAV.
(9). János Tomcsányi. Chest Pain and Wide QRS Tachycardia. JAMA Intern Med. 2023.
A patient in their 70s with diabetes presented with 3 hours of chest pain. The patient had a history of acute myocardial infarction 5 years before, with stenting of the right coronary artery and left anterior descending coronary artery. At the current hospital admission, the patient denied any dyspnea but felt dizzy while in the sitting position. The patient’s supine blood pressure measured 100/55 mm Hg. Laboratory test results revealed a 83 ng/L serum troponin T level (upper limit of normal [ULN], 14 ng/L; to convert to μg/L, multiply by 1) and 76 U/L serum creatine kinase level (ULN, 170 U/L; to convert to μkat/L, multiply by 0.0167).
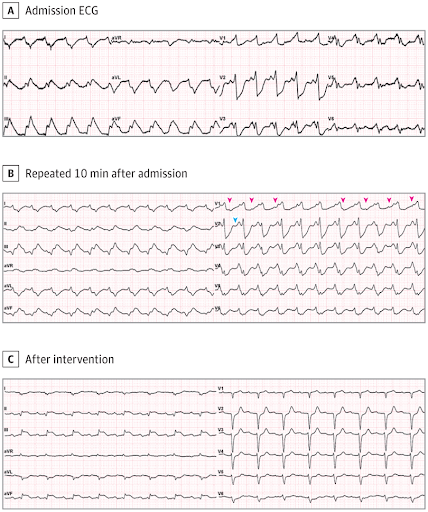
The electrocardiogram (ECG) on admission showed a regular tachycardia at a rate of 135 beats per minute. There was an unusual right bundle branch block morphology with right axis deviation (Figure, A). A repeated ECG about 10 minutes later showed an identical heart rate, with similar QRS morphology in the chest leads. However, the frontal plane QRS axis had changed substantially (Figure, B).
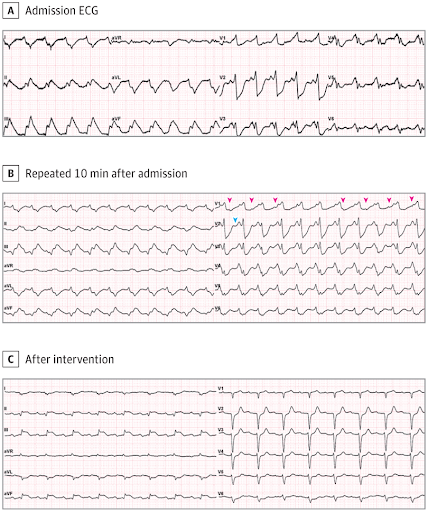
A, The admission ECG showed an unusual regular wide QRS tachycardia at a rate of 135 beats per minute. B, Repeated ECG 10 minutes later revealed an identical heart rate but different morphology in the frontal plane (QRS axis, -300 to -600; QRS duration, 220 milliseconds). Pink arrowheads indicate dissociated P waves. The blue arrowhead indicates the onset of QRS in lead V2. After this arrowhead, the positive little bump is not a P wave but part of the QRS. C, After 1 treatment with intravenous lidocaine, 100 mg, the ECG demonstrated sinus rhythm with first-degree atrioventricular block, abnormal Q waves in leads I and aVL, and ST segment elevation in the inferior leads.
Questions: What was the cause of the wide QRS complex tachycardia and abrupt change in the QRS axis? What were the best treatment options for the patient?
Interpretation
The ECG on presentation showed a regular wide QRS complex tachycardia with QRS duration of more than 160 milliseconds and a rate of 135 beats per minute. The ECG performed by the emergency department physician was initially interpreted as supraventricular/sinus tachycardia with right bundle branch block and precordial ST segment depression. However, on closer inspection, there were at least 2 important ECG features that suggested ventricular tachycardia. In the first ECG (Figure, A), the apparent P waves, the small bumps seen in leads V2 and V3, occurred simultaneously with the onset of the QRS complexes in the V1 lead, indicating that these positive waves were part of the wide and notched QRS complexes rather than separate P waves. A second ECG (Figure, B) demonstrated a wide QRS complex tachycardia with deep ST depression in the precordial leads. In this ECG, the lead V1 hid regular small upright P waves (see arrowheads) at a rate of 100 beats per minute, dissociated from the wide QRS complexes. Atrioventricular (AV) dissociation is a defining characteristic for ventricular tachycardia. The identical rate and near-identical horizontal plane QRS morphology but changing QRS axis suggested ventricular tachycardias with different exit points.
Clinical Course
Given the stable blood pressure, the patient received lidocaine, 100 mg, which was administered intravenously over 2 minutes. Within minutes, the tachycardia terminated, but the chest pain did not resolve. The ECG now depicted sinus rhythm with first-degree AV block and inferior ST segment elevation myocardial infarction (Figure, C). Treatment with intravenous heparin was initiated, and the patient was transferred to the cardiac catheterization laboratory, where urgent coronary angiography results showed an occluded right coronary artery distal to the previously implanted stent. The peak creatine kinase level was 3700 U/L (UNL, 170 U/L). The left ventricular ejection fraction decreased to 10%. Because of progressive heart failure and concomitant kidney failure, the patient died on the fifth hospital day.
Discussion
Several studies have shown that wide-complex tachycardia identification algorithms perform poorly at the bedside and are frequently associated with misdiagnosis and inappropriate treatment.1,2 There are several common scenarios associated with misdiagnosis. First is not recognizing AV dissociation, a crucial clue for ventricular tachycardia that is present in up to 50% of all wide-complex tachycardias.2 Frequently, there is no attempt to scrutinize for dissociated P waves or, as in the case presented, parts of the QRS complexes or ST segments are incorrectly identified as P waves. Second, the cause of the wide-complex tachycardia is incorrectly deduced from the patient’s relatively benign clinical and hemodynamic status. In patients with structural heart disease, regardless of the clinical status, most wide-complex tachycardia is ventricular tachycardia.2 Third, because ventricular tachycardia in acute coronary syndrome is usually polymorphic,3 a ventricular origin of monomorphic tachycardia with normal QT duration is not even considered. Although rare, the SWEDE HEART registry reported early monomorphic ventricular tachycardia during ST elevation myocardial infarction in 1.5% of the cases. These were high-risk patients with high all-cause mortality during 8 years of follow-up.4 In ventricular tachycardia with hemodynamic instability, direct current electrical shock followed by intravenous amiodarone is the most effective treatment.5 However, in stable ventricular tachycardia that is associated with an acute ischemic syndrome, intravenous lidocaine can also be effective.6
Take-home Points
In a case of wide QRS tachycardia, a ventricular origin should always be considered if the patient has known structural heart disease.
Patients with ventricular tachycardia can be clinically stable even in the setting of acute coronary syndrome.
Atrioventricular dissociation is the most reliable sign in identifying ventricular tachycardia. If you are not sure, repeat the ECG with a longer rhythm strip.
Although polymorphic ventricular arrhythmias are most often seen in acute ischemia, monomorphic ventricular tachycardia can also occur. This is especially true if there is scar tissue present from a previous event.
During wide QRS tachycardia, it is difficult to interpret repolarization abnormalities. A significant ST-T change occurring at similar heart rates usually indicates acute ischemic origin of the chest pain.
(10). Pacheco LD, et al. Tranexamic Acid to Prevent Obstetrical Hemorrhage after Cesarean Delivery. 2023
Prophylactic use of tranexamic acid at the time of cesarean delivery has been shown to decrease the calculated blood loss, but the effect on the need for blood transfusions is unclear.
We randomly assigned patients undergoing cesarean delivery at 31 U.S. hospitals to receive either tranexamic acid or placebo after umbilical-cord clamping. The primary outcome was a composite of maternal death or blood transfusion by hospital discharge or 7 days post partum, whichever came first. Key secondary outcomes were estimated intraoperative blood loss of more than 1 liter (prespecified as a major secondary outcome), interventions for bleeding and related complications, the preoperative-to-postoperative change in the hemoglobin level, and postpartum infectious complications. Adverse events were assessed.
A total of 11,000 participants underwent randomization (5529 to the tranexamic acid group and 5471 to the placebo group); scheduled cesarean delivery accounted for 50.1% and 49.2% of the deliveries in the respective groups. A primary-outcome event occurred in 201 of 5525 participants (3.6%) in the tranexamic acid group and in 233 of 5470 (4.3%) in the placebo group (adjusted relative risk, 0.89; 95.26% confidence interval [CI], 0.74 to 1.07; P=0.19). Estimated intraoperative blood loss of more than 1 liter occurred in 7.3% of the participants in the tranexamic acid group and in 8.0% of those in the placebo group (relative risk, 0.91; 95% CI, 0.79 to 1.05). Interventions for bleeding complications occurred in 16.1% of the participants in the tranexamic acid group and in 18.0% of those in the placebo group (relative risk, 0.90; 95% CI, 0.82 to 0.97); the change in the hemoglobin level was -1.8 g per deciliter and -1.9 g per deciliter, respectively (mean difference, -0.1 g per deciliter; 95% CI, -0.2 to -0.1); and postpartum infectious complications occurred in 3.2% and 2.5% of the participants, respectively (relative risk, 1.28; 95% CI, 1.02 to 1.61). The frequencies of thromboembolic events and other adverse events were similar in the two groups.
Prophylactic use of tranexamic acid during cesarean delivery did not lead to a significantly lower risk of a composite outcome of maternal death or blood transfusion than placebo.
(11). Manisha Balwani, et al. Dersimelagon in Erythropoietic Protoporphyrias. N Engl J Med 2023; 388:1376-1385.
Erythropoietic protoporphyria and X-linked protoporphyria are inborn errors of heme biosynthesis that cause elevated circulating levels of metal-free protoporphyrin and phototoxicity. Both disorders are characterized by excruciating phototoxic attacks after exposure to visible light. Dersimelagon is a new, orally administered, selective melanocortin 1 receptor agonist that increases levels of skin eumelanin.
We conducted a randomized, placebo-controlled, phase 2 trial to investigate the efficacy and safety of dersimelagon with respect to the time to onset and the severity of symptoms associated with sunlight exposure in patients with erythropoietic protoporphyria or X-linked protoporphyria. Patients 18 to 75 years of age were randomly assigned in a 1:1:1 ratio to receive placebo or dersimelagon at a dose of 100 or 300 mg once daily for 16 weeks. The primary end point was the change from baseline to week 16 in the time to the first prodromal symptom associated with sunlight exposure. Patients recorded daily sunlight exposure and symptom data in an electronic diary. Quality of life and safety were also assessed.
Of the 102 patients (93 with erythropoietic protoporphyria and 9 with X-linked protoporphyria) who underwent randomization, 90% completed the treatment period. The mean daily time to the first prodromal symptom associated with sunlight exposure increased significantly with dersimelagon: the least-squares mean difference from placebo in the change from baseline to week 16 was 53.8 minutes in the 100-mg dersimelagon group (P=0.008) and 62.5 minutes in the 300-mg dersimelagon group (P=0.003). The results also suggest that quality of life improved in patients receiving dersimelagon as compared with placebo. The most common adverse events that occurred or worsened during treatment were nausea, freckles, headache, and skin hyperpigmentation.
At both doses evaluated, dersimelagon significantly increased the duration of symptom-free sunlight exposure in patients with erythropoietic protoporphyria or X-linked protoporphyria
(12). Michaí«l Chassé et al. Effect of Donor Sex on Recipient Mortality in Transfusion. N Engl J Med. 2023;388(15):1386-1395.
Conflicting observational evidence exists regarding the association between the sex of red-cell donors and mortality among transfusion recipients. Evidence to inform transfusion practice and policy is limited.
In this multicenter, double-blind trial, we randomly assigned patients undergoing red-cell transfusion to receive units of red cells from either male donors or female donors. Patients maintained their trial-group assignment throughout the trial period, including during subsequent inpatient and outpatient encounters. Randomization was conducted in a 60:40 ratio (male donor group to female donor group) to match the historical allocation of red-cell units from the blood supplier. The primary outcome was survival, with the male donor group as the reference group.
A total of 8719 patients underwent randomization before undergoing transfusion; 5190 patients were assigned to the male donor group, and 3529 to the female donor group. At baseline, the mean (±SD) age of the enrolled patients was 66.8±16.4 years. The setting of the first transfusion was as an inpatient in 6969 patients (79.9%), of whom 2942 (42.2%) had been admitted under a surgical service. The baseline hemoglobin level before transfusion was 79.5±19.7 g per liter, and patients received a mean of 5.4±10.5 units of red cells in the female donor group and 5.1±8.9 units in the male donor group (difference, 0.3 units; 95% confidence interval [CI], -0.1 to 0.7). Over the duration of the trial, 1141 patients in the female donor group and 1712 patients in the male donor group died. In the primary analysis of overall survival, the adjusted hazard ratio for death was 0.98 (95% CI, 0.91 to 1.06).
This trial showed no significant difference in survival between a transfusion strategy involving red-cell units from female donors and a strategy involving red-cell units from male donors.
(13). Caroline F. Wright. Genomic Diagnosis of Rare Pediatric Disease in the United Kingdom and Ireland. N Engl J Med. 2023
Pediatric disorders include a range of highly penetrant, genetically heterogeneous conditions amenable to genomewide diagnostic approaches. Finding a molecular diagnosis is challenging but can have profound lifelong benefits.
We conducted a large-scale sequencing study involving more than 13,500 families with probands with severe, probably monogenic, difficult-to-diagnose developmental disorders from 24 regional genetics services in the United Kingdom and Ireland. Standardized phenotypic data were collected, and exome sequencing and microarray analyses were performed to investigate novel genetic causes. We developed an iterative variant analysis pipeline and reported candidate variants to clinical teams for validation and diagnostic interpretation to inform communication with families. Multiple regression analyses were performed to evaluate factors affecting the probability of diagnosis.
A total of 13,449 probands were included in the analyses. On average, we reported 1.0 candidate variant per parent-offspring trio and 2.5 variants per singleton proband. With the use of clinical and computational approaches to variant classification, a diagnosis was made in approximately 41% of probands (5502 of 13,449), of whom 76% had a pathogenic de novo variant. Another 22% of probands (2997 of 13,449) had variants of uncertain significance in genes that were strongly linked to monogenic developmental disorders. Recruitment in a parent-offspring trio had the largest effect on the probability of diagnosis (odds ratio, 4.70; 95% confidence interval [CI], 4.16 to 5.31). Probands were less likely to receive a diagnosis if they were born extremely prematurely (i.e., 22 to 27 weeks’ gestation; odds ratio, 0.39; 95% CI, 0.22 to 0.68), had in utero exposure to antiepileptic medications (odds ratio, 0.44; 95% CI, 0.29 to 0.67), had mothers with diabetes (odds ratio, 0.52; 95% CI, 0.41 to 0.67), or were of African ancestry (odds ratio, 0.51; 95% CI, 0.31 to 0.78).
Among probands with severe, probably monogenic, difficult-to-diagnose developmental disorders, multimodal analysis of genomewide data had good diagnostic power, even after previous attempts at diagnosis. (Funded by the Health Innovation Challenge Fund and Wellcome Sanger Institute.)
(13). Paul M Ridker et al. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: a collaborative analysis of three randomised trials. Lancet 2023;401(10384):P1293-1301.
Inflammation and hyperlipidaemia jointly contribute to atherothrombotic disease. However, when people are treated with intensive statin therapy, the relative contributions of inflammation and hyperlipidaemia to the risk of future cardiovascular events might change, which has implications for the choice of adjunctive cardiovascular therapeutics. We aimed to evaluate the relative importance of high-sensitivity C-reactive protein (CRP) and low-density lipoprotein cholesterol (LDLC) as determinants of risk for major adverse cardiovascular events, cardiovascular death, and all-cause-death among patients receiving statins.
We did a collaborative analysis of patients with-or at high risk of-atherosclerotic disease, who were receiving contemporary statins and were participants in the multinational PROMINENT (NCT03071692), REDUCE-IT (NCT01492361), or STRENGTH (NCT02104817) trials. Quartiles of increasing baseline high-sensitivity CRP (a biomarker of residual inflammatory risk) and of increasing baseline LDLC (a biomarker of residual cholesterol risk) were assessed as predictors of future major adverse cardiovascular events, cardiovascular death, and all-cause death. Hazard ratios (HRs) for cardiovascular events and deaths were calculated across quartiles of high-sensitivity CRP and LDLC in analyses adjusted for age, gender, BMI, smoking status, blood pressure, previous history of cardiovascular disease, and randomised treatment group assignment.
31 245 patients were included in the analysis from the PROMINENT (n=9988), REDUCE-IT (n=8179), and STRENGTH (n=13 078) trials. The observed ranges for baseline high-sensitivity CRP and LDLC, and the relationships of each biomarker to subsequent cardiovascular event rates, were almost identical in the three trials. Residual inflammatory risk was significantly associated with incident major adverse cardiovascular events (highest high-sensitivity CRP quartile vs lowest high-sensitivity CRP quartile, adjusted HR 1.31, 95% CI 1.20-1.43; p<0.0001), cardiovascular mortality (2.68, 2.22-3.23; p<0.0001), and all-cause mortality (2.42, 2.12-2.77; p<0.0001). By contrast, the relationship of residual cholesterol risk was neutral for major adverse cardiovascular events (highest LDLC quartile vs lowest LDLC quartile, adjusted HR 1.07, 95% CI 0.98-1.17; p=0.11), and of low magnitude for cardiovascular death (1.27, 1.07-1.50; p=0.0086) and all-cause death (1.16, 1.03-1.32; p=0.025).
Among patients receiving contemporary statins, inflammation assessed by high-sensitivity CRP was a stronger predictor for risk of future cardiovascular events and death than cholesterol assessed by LDLC. These data have implications for the selection of adjunctive treatments beyond statin therapy and suggest that combined use of aggressive lipid-lowering and inflammation-inhibiting therapies might be needed to further reduce atherosclerotic risk.
(14). Gregg EW, et al. Improving health outcomes of people with diabetes: target setting for the WHO Global Diabetes Compact. Lancet 2023;401(10384):P1302-1312.
The Global Diabetes Compact is a WHO-driven initiative uniting stakeholders around goals of reducing diabetes risk and ensuring that people with diabetes have equitable access to comprehensive, affordable care and prevention.
We describe the development and scientific basis for key health metrics, coverage, and treatment targets.
Four domains: factors at a structural, system, or policy level; processes of care; behaviours and biomarkers such as glycated haemoglobin (HbA1c); and health events and outcomes
Three risk tiers (diagnosed diabetes, high risk, or whole population).
This process led to five core national metrics and target levels:
- of all people with diabetes, at least 80% have been clinically diagnosed;
- For people with diagnosed diabetes,
- (2) 80% have HbA1c concentrations below 8.0% (63.9 mmol/mol);
- (3) 80% have blood pressure lower than 140/90 mm Hg;
- (4) at least 60% of people 40 years or older are receiving therapy with statins;
- (5) each person with type 1 diabetes has continuous access to insulin, blood glucose meters, and test strips.
We also propose several complementary metrics that warrant scale-up in population-based surveillance systems.
These include estimation of cause-specific mortality, and incidence of end-stage kidney disease, lower-extremity amputations, and incidence of diabetes.
Primary prevention of diabetes and integrated care to prevent long-term complications remain important areas for the development of new metrics and targets.
These metrics and targets are intended to drive multisectoral action applied to individuals, health systems, policies, and national health-care access to achieve the goals of the Global Diabetes Compact.
Although ambitious, their achievement can result in broad health benefits for people with diabetes.
(15). Chandyo RK, et al. The effect of vitamin B12 supplementation during pregnancy on infant growth and development in Nepal: a community-based, double-blind, randomised, placebo-controlled trial. 2023.
Vitamin B12 is required for healthy infant growth and development, but low and marginal vitamin B12 status is endemic in low-income and middle-income countries. We aimed to measure the effect of vitamin B12 supplementation from early pregnancy until 6 months post partum on infant growth and neurodevelopment.
In this community-based, double-blind, placebo-controlled trial, we randomly assigned (1:1) 800 pregnant women (aged 20-40 years) who were up to 15 weeks pregnant – recruited from home visits and outpatient departments at three hospitals in Nepal – to daily supplementation with 50 μg oral vitamin B12 or placebo until 6 months postpartum. Independent scientists generated the list that linked allocation to participants’ study identification number. Participants were masked to group assignment and all investigators were masked until data cleaning was completed. The primary outcomes were length-for-age Z score (LAZ) at age 12 months and the cognitive composite score of the Bayley Scales of Infant and Toddler Development (3rd edition) at age 6 months and 12 months. The primary and secondary outcomes, including adverse events, were assessed in the intention-to-treat population, for all participants with available outcome data. This trial is registered with ClinicalTrials.gov, NCT03071666.
800 eligible pregnant women were enrolled in the trial between March 28, 2017, and Oct 15, 2020, with 400 women randomly assigned to each group. Follow-up was completed on May 18, 2022. At baseline, 569 (71%) of 800 women had plasma vitamin B12 indicating low or marginal status (<221 pmol/L). We found no effect of vitamin B12 on the primary outcomes. The mean LAZ at age 12 months were -0.57 (SD 1.03) in the B12 group and -0.55 (1.03) in the placebo group (366 infants in the vitamin B12 group vs 363 infants in the placebo group) with a mean difference of -0.02 (95% CI -0.16 to 0.13). The mean cognitive composite scores were 97.7 (SD 10.5) in the B12 group and 97.1 (10.2) in the placebo group, with a mean difference of 0.5 (95% CI -0·6 to 1.7) measured in 364 and 361 infants. Stillbirths or infant deaths occurred in three (1%) of 374 women in the vitamin B12 group and nine (2%) of 379 women in the placebo group.
Although vitamin B12 deficiency was prevalent in our study population and vitamin B12 supplementation from early pregnancy substantially improved vitamin B12 status, supplementation did not improve infant growth or neurodevelopment. Our findings support the current WHO recommendations of no routine vitamin B12 supplementation during pregnancy.
(16). Song-Jie Shen et al. Chemotherapy for early-stage breast cancer: the more the better? 2023;401(10384):P1243-1245.
Breast cancer is the most common malignancy in women worldwide1 and treatment de-escalation of early-stage breast cancer has been a contentious topic of discussion. Breast-conserving surgery has gradually replaced mastectomy, eliminating the need for breast surgery in patients with a pathological complete response on image-guided vacuum-assisted core biopsy after neoadjuvant systemic therapy shows highly promising results.2 Sentinel lymph node biopsy, rather than axillary lymph node dissection, is the standard of care for clinical node-negative breast cancer, and some patients with node-positive disease also do not need further surgery.3 Chemotherapy substantially reduces the risk of recurrence and death due to early-stage breast cancer, but it can cause short-term and long-term side-effects. Multigene assays have been used to avoid chemotherapy in patients with hormone receptor-positive tumours, human epidermal growth factor receptor 2 (HER2)-negative tumours, and a low recurrence score, in addition to individuals with nodal involvement.4
For more than a decade, a combination of anthracycline and taxane has been considered optimal chemotherapy for women with early-stage breast cancer. However, due to the toxicity of anthracyclines, non-anthracycline regimens, such as docetaxel plus cyclophosphamide for HER2-negative breast cancer and paclitaxel plus trastuzumab for HER2-positive breast cancer, have been recommended as preferred regimens in clinical guidelines5, 6 and the latest National Comprehensive Cancer Network guidelines (version 4.2022).
In The Lancet, the Early Breast Cancer Trialists’ Collaborative Group reported a patient level meta-analysis of 100 000 women in 86 randomised trials on the benefits and risks of anthracycline and taxane-containing chemotherapy for early-stage operable breast cancer, focusing on trials comparing taxane-based regimens with versus without anthracycline.7 Recurrence rates were about 14% lower (rate ratio [RR] 0.86, 95% CI 0.79-0.93; p=0.0004) with taxane regimens including anthracycline than without anthracycline, equating to an absolute reduction of 2.6% (95% CI 0.9-4.2) in 10-year recurrence risk. The 10-year breast cancer mortality was reduced by 1.6% (0.1-3.1). Reductions in recurrence were larger with concurrent anthracycline plus taxane regimens (RR 0.58, 0.47-0.73; p<0.0001) than with sequential anthracycline plus taxane regimens (0.94, 0.83-1.06; p=0.30) because of the higher cumulative anthracycline and taxane doses in concurrent regimens. There was a 13% average reduction in recurrence in anthracycline regimens with taxane compared with those without (0·87, 0·82-0·93; p<0·0001), which translates to an absolute reduction of 3.3% (1.3-5.3) in 10-year risk of recurrence, and the absolute reduction in 10-year breast cancer mortality was 3.6% (1.8-5.4) with the addition of a taxane. By contrast with the so-called less is more conception, the results showed that combined anthracycline and taxane was more efficacious than either anthracycline or taxane alone, and women assigned to higher cumulative doses and more dose-intense schedules had greater reductions in breast cancer recurrence and mortality.
De-escalation in local therapy has been the standard of care for many years, whereas in systemic therapy of early-stage breast cancer, escalation has become more common. In endocrine therapy for patients with hormone receptor-positive tumours, ovarian function suppression is recommended for premenopausal women with an indication for chemotherapy or for women younger than 35 years. The standard duration of endocrine therapy has been extended from 5 years to 5-10 years, and CDK4/6 inhibitors (abemaciclib) have been suggested to be added for patients at high-risk. For anti-HER2 adjuvant therapy, the recommended regimen has evolved from trastuzumab to the dual-HER2 blockade strategy (pertuzumab plus trastuzumab), and to intensive therapy with trastuzumab emtansine or extended adjuvant therapy with neratinib. Several limitations should be recognised to consider whether the EBCTCG meta-analysis findings support chemotherapy escalation in clinical practice. First, there were some heterogeneities among the trial designs that could confound the treatment effects, including different taxanes (paclitaxel or docetaxel) and anthracyclines (doxorubicin or epirubicin), administering schedules (concurrent or sequential), cumulative doses, frequency of administration, treatment duration, and concomitant use of non-anthracycline drugs (cyclophosphamide, capecitabine, or carboplatin). Consequently, these results, based on comparing a range of trials, should be interpreted with caution. Second, the balance of benefit versus toxicity needs to be considered carefully for escalation in chemotherapy. According to the results, concurrent taxane and anthracycline for six cycles seems to be the preferred regimen to achieve optimum survival benefit, with similar proportional reductions irrespective of patient age or tumour characteristics, including size, grade, nodal involvement, hormone receptor status, or HER2 expression. However, even for patients at high risk, sequential taxane and anthracycline is the guideline-recommended option.8 Although the Early Breast Cancer Trialists’ Collaborative Group meta-analysis showed no significant difference between treatment groups for the overall incidence of new, non-breast primary cancers and death without recurrence, including from cardiovascular disease or other primary cancers, individual patient-level data on non-fatal toxicity and quality of life were not available.
For this common cancer in women, health-care providers should weigh therapeutic benefits against short-term and long-term risks.9 The results of this meta-analysis are clinically important. For patients at sufficient risk of recurrence, and fit enough to be offered chemotherapy, the combination of taxane and anthracycline can be suggested to achieve the best possible reductions in breast cancer recurrence and mortality. However, one chemotherapy regimen cannot fit all subtypes of breast cancer. In particular, with the escalation of anti-HER2 therapy, prospective studies will be warranted to validate the more-the-better rule in chemotherapy within this setting.
(17). Jessica Catchpole. A search for salvation, a semi- autobiographical book on psychiatric care. The Lancet 2023;401(10384):P1257.
Daniele Mencarelli’s semi-autobiographical second novel. Everything Calls for Salvation follows the involuntary hospitalisation of a 20-year-old eponymous Daniele in 1994, his week of confinement, the people he meets, and the insight he gains. Each character on the psychiatric ward serves a purpose. Frantic Madonnina, whose identity is unknown and who only prays to the Virgin Mary, stands in contrast to Alessandro, who lies motionless in a catatonic state. Jaded Mario, a former teacher, lectures on the nature of mental illness and the bleakness of treatment. Flamboyant Gianluca, determined to appear jovial to hide his pain, is treated as subhuman by his mother, serving as a foil for Daniele’s loving and doting parents. “[E]motional giant” Giorgio shows how a single incident during childhood can ruin a life.
The novel also highlights failings in care. The people Daniele meets in hospital live shunted from doctor to doctor, diagnosis to diagnosis, and treatment to treatment without continuity of care or hope of cure. Each character has a story of callousness by the health-care system that is meant to provide care and support-“the very people who came running to help them, who are worse than the malady itself”, writes Mencarelli. No clinician discusses Giorgio’s care with him because he is “demented”. Mario laments the “kind of race… nowadays to put the label of disorder on things that until a short while ago were simply a person’s characteristics, sometimes even considered virtues”. Gianluca remembers a doctor who “needed a brass band to wake him up”. They do not expect miracles, but they lament clinicians who seem “disaffected with themselves and the entire human race”.
Mencarelli’s characterisation of Daniele and the individuals who share his compulsory time on the ward is nuanced. None of them is perfect. Yet all show that amid suffering, kindness and camaraderie can flourish. The reader feels at home with these men.
But living with mental health conditions is no cosy holiday. The climax of Everything Calls for Salvation, when it unexpectedly comes, is brief but unsettling. Here, too, is tenderness and compassion, as well as the preventable harsh consequences of a mental health crisis.
The real beauty of the novel is Mencarelli’s poetic prose, transfixing and transporting the reader into the world he has created. This grace and subtlety is not fully captured in the subsequent Netflix series Everything Calls for Salvation. There are things the Netflix series gets right. The acting is sublime, particularly Lorenzo Renzi, who plays Giorgio. All the actors faithfully convey the book’s passion. Another win is the more even-handed treatment of health-care professionals. Doctor Mancino in the book personifies clinical callousness. He falls asleep during an appointment. He looks at Daniele “as if [he] were a flea…an absolute annoyance”. The novel references overwork and inadequate funding for mental health care, but the Netflix series makes the message starker. A humanised Mancino eats his dinner alone in his office. His colleague explains he often sleeps there too, not having time to leave due to a heavy caseload. He is not heartless for heartlessness’s sake; he is exhausted. The problem of overwork and burnout among clinicians is real, especially in the context of the lasting impacts of the COVID-19 pandemic. Amid the backdrop of Italy’s austerity in the face of the government debt crisis and the worsening economic state of Europe given inflation, gas shortages, and war, there is gloom over the future of public services, including health. The message that health-care professionals are already at breaking point hits home.
The story Mencarelli wrote is one that needs to be told. Like Daniele, many of us who live with mental health conditions inwardly pray “Holy Medicine, please watch over me and guide me, make me become normal, make me be worthy of my home. Amen.” For me, I’ve never heard my pain spoken so eloquently, and I want to tell the world.
(18). Geoff Watts. Jared Randall Curtis, OBITUARY. Lancet 2023;401(10384):P1260.
The High lights:
Critical care physician and champion of palliative care in the US. He was born on Feb 14, 1960 and died of amyotrophic lateral sclerosis, on Feb 6, 2023 aged 62 years.
He wondered if the focus of critical care medicine might be unduly narrow and overlooked the broader wellbeing of patients.
Curtis felt that patients in intensive care units (ICU) were too often treated as failing organisms rather than sick people who, along with their families, also needed other forms of close attention.
“Randy was a scientist at heart, but he was also a caring person. He understood early on that people needed help when dying in the ICU. It was an unmet need.
” Bringing change to this aspect of critical care medicine became Curtis’s principal objective. His impact has been evident in terms of changing culture. He opened people’s perspectives to [better communication] as an important part of the care we deliver to seriously ill patients.”
Curtis established the Cambia Palliative Care Center of Excellence in 2012.
“Improving communication between clinicians and patients and their families, talking about their illness…was at the core of a lot of his work”,
The importance Curtis attached to this was no arbitrary choice. He aimed to make patient assessments more systematic by devising outcome measures to rate their feelings about their experiences. One such was the QODD, or Quality of Dying and Death score, that compares an individual’s previously expressed preferences with what could be seen to happen when the processes of dying and death came about.
“It was an attempt to assess objectively whether someone has a good death. Randy believed it was possible to train physicians and nurses to be better communicators with patients dying in the ICU.”
Empirical studies showed that improved communication is indeed associated with a better quality of death.
But widespread acceptance was not immediate., “It took time for the field to understand the importance of evolving their communication skills.
“Clinicians do not mind being updated on the technicalities of medical equipment, “But if I tell a clinician I’d like to teach how to communicate better, there’s a natural resistance…nobody likes to be told this.”
Curtis was a great communicator. “And this skill was a factor in his ability to champion his work”,
“He could be very stubborn, he didn’t give up on his ideas and he didn’t give up on people
He was a man of great integrity, incredibly rigorous in his belief that science should address these questions.”
“Curtis’s illness prevented him seeing patients during the last year of his life. But he was still mentoring people by Zoom calls until 3 weeks before he died.”
(19). Blue toes in a neonate

Laboratory investigations showed normal complete blood count, coagulation studies, and infection parameters-including C-reactive protein concentration (0.13 mg/dL; normal <0.5) and interleukin-6 concentration (18.6 ng/L; normal <50). The day after presentation, the lesions evolved into acral necrosis.
The baby’s mother reported infection with SARS-CoV-2 in mid-pregnancy with mild COVID-19 symptoms of a cough, rhinitis, aching limbs, and a sore throat. Serological testing of neonatal serum collected on the sixth day of the baby’s life showed an anti-SARS-CoV-2 IgG antibody concentration against spike protein S1 receptor-binding domain of 766 U/mL. Neonatal RT-PCR for SARS-CoV-2 was negative.
At this stage, our working diagnosis was acral gangrenous necrosis following a thromboembolic event. We decided to manage the case conservatively with the use of dry dressings; one month after the lesions’ appearance, they were healing spontaneously apart from a small crust on the tip of the first toe (figure).
Blue toe syndrome is well described in adults; one or more of the toes become blue or purple, due to decreased arterial flow, impaired venous outflow, and abnormal circulating blood. Specific causes are numerous, and identification depends upon methodical history taking, a complete physical examination, and selected laboratory investigations.
In neonates, blue toe syndrome is mostly a benign condition, related to acrocyanosis caused by peripheral vasoconstriction and increased tissue oxygen extraction. Newborn infants are the most vulnerable group of paediatric patients likely to develop thrombosis and have thromboembolic complications. Pathological processes in the placenta-associated with maternal infections-might be important in the aetiology. Neonatal vascular complications have been reported following intrauterine SARS-CoV-2 exposure and might be caused by a hypercoagulable state in the fetus. In our case, the prepartum SARS-CoV-2 infection was possibly related to the patient’s blue toes. However, because the maternal infection occurred several months prior to birth, there was no evidence of the neonate being infected, and coagulation tests were all within normal range, it seems unlikely.
(20). How artificial intelligence is matching drugs to patients
https://www.bbc.com/news/business-65260592
A neuroscientist, Dr Talia Cohen Solal is the co-founder and chief executive of Israeli health-tech firm Genetika+.
Established in 2018, the company states its technology can best match antidepressants to patients, to avoid unwanted side effects, and make sure that the prescribed drug works as well as possible.
“We can characterise the right medication for each patient the first time,” adds Dr Cohen Solal.
Genetika+ does this by combining the latest in stem cell technology – the growing of specific human cells – with artificial intelligence (AI) software.
From a patient’s blood sample its technicians can generate brain cells. These are then exposed to several antidepressants, and recorded for cellular changes called “biomarkers”.
This information, taken with a patient’s medical history and genetic data, is then processed by an AI system to determine the best drug for a doctor to prescribe and the dosage.
The technology is currently still in the development stage.
There are more than 280 million people globally who suffer from depression, according to the World Health Organization. And while taking antidepressants certainly won’t be the correct treatment for all, it has long been estimated that almost two thirds of initial prescriptions for depression or anxiety may not work properly.
A senior lecturer of biomedical AI and data science at King’s College London, she says that AI has so far helped with everything “from identifying a potential target gene for treating a certain disease, and discovering a new drug, to improving patient treatment by predicting the best treatment strategy, discovering biomarkers for personalised patient treatment, or even prevention of the disease through early detection of signs for its occurrence”
However, Dr Sailem emphasises that the pharmaceutical sector shouldn’t be tempted to race ahead with AI, and should employ strict measures before relying on its predictions.
“An AI model can learn the right answer for the wrong reasons, and it is the researchers’ and developers’ responsibility to ensure that various measures are employed to avoid biases, especially when trained on patients’ data,” she says.
Hong Kong-based Insilico Medicine is using AI to accelerate drug discovery. “Our AI platform is capable of identifying existing drugs that can be re-purposed, designing new drugs for known disease targets, or finding brand new targets and designing brand new molecules,” says co-founder and chief executive Alex Zhavoronkov. Its most developed drug, a treatment for a lung condition called idiopathic pulmonary fibrosis, is now being clinically trialled.
Mr Zhavoronkov says it typically takes four years for a new drug to get to that stage, but that thanks to AI, Insilico Medicine achieved it “in under 18 months, for a fraction of the cost”.
Back in Israel, Dr Cohen Solal says AI can help “solve the mystery” of which drugs work.
(21). Gilmar Reis. Oral Fluvoxamine With Inhaled Budesonide for Treatment of Early-Onset COVID-19: A Randomized Platform Trial. Ann Intern Med. 2023
Previous trials have demonstrated the effects of fluvoxamine alone and inhaled budesonide alone for prevention of disease progression among outpatients with COVID-19.
Objective:
To determine whether the combination of fluvoxamine and inhaled budesonide would increase treatment effects in a highly vaccinated population.
Design:
Randomized, placebo-controlled, adaptive platform trial. (ClinicalTrials.gov: NCT04727424)
Setting:
12 clinical sites in Brazil.
Participants:
Symptomatic adults with confirmed SARS-CoV-2 infection and a known risk factor for progression to severe disease.
Intervention:
Patients were randomly assigned to either fluvoxamine (100 mg twice daily for 10 days) plus inhaled budesonide (800 mcg twice daily for 10 days) or matching placebos.
Measurements:
The primary outcome was a composite of emergency setting retention for COVID-19 for more than 6 hours, hospitalization, and/or suspected complications due to clinical progression of COVID-19 within 28 days of randomization. Secondary outcomes included health care attendance (defined as hospitalization for any cause or emergency department visit lasting >6 hours), time to hospitalization, mortality, patient-reported outcomes, and adverse drug reactions.
Results:
Randomization occurred from 15 January to 6 July 2022. A total of 738 participants were allocated to oral fluvoxamine plus inhaled budesonide, and 738 received placebo. The proportion of patients observed in an emergency setting for COVID-19 for more than 6 hours or hospitalized due to COVID-19 was lower in the treatment group than the placebo group (1.8% [95% credible interval (CrI), 1.1% to 3.0%] vs. 3.7% [95% CrI, 2.5% to 5.3%]; relative risk, 0.50 [95% CrI, 0.25 to 0.92]), with a probability of superiority of 98.7%. No relative effects were found between groups for any of the secondary outcomes. More adverse events occurred in the intervention group than the placebo group, but no important differences between the groups were detected.
Limitation:
Low event rate overall, consistent with contemporary trials in vaccinated populations.
Conclusion:
Treatment with oral fluvoxamine plus inhaled budesonide among high-risk outpatients with early COVID-19 reduced the incidence of severe disease requiring advanced care.
(22). Yan Chen. Challenges in Clinical Electrocardiography. JAMA Intern Med. 2023.
A patient in their late teens presented to the outpatient department stating that they had felt the implanted cardioverter defibrillator (ICD) deliver a shock 3 times within the past 6 months. The patient had a history of cardiac arrest due to ventricular fibrillation and had received an ICD 20 months ago. On admission, the patient’s vital signs were as follows: temperature, 36.4 °C; blood pressure, 114/69 mm Hg; pulse rate, 70 beats/min; and respiratory rate, 18 breaths/min. Cardiopulmonary examination was unremarkable. Troponin I, N-terminal probrain natriuretic peptide (NT-pro BNP), and D-dimer levels were normal. The 12-lead electrocardiogram (ECG) obtained at admission is shown in the Figure.
Figure. Electrocardiogram (ECG) Findings on Admission
Electrocardiogram (ECG) Findings on Admission
Standard 12-lead ECG showed sinus rhythm (heart rate, 69 beats/min), right axis deviation (108deg), tall P waves with a consistent PR interval, slightly widened, fragmented QRS complexes (112 ms) (red arrows), ST-segment elevation of 1 to 2 mm with T-wave inversion in the right precordial leads (V1 to V3), and bidirectional T wave in lead V4. There was a low-amplitude signal (amplitudes <1 mm, duration 40 ms) occurring after the QRS complex and before the onset of the T wave in the right precordial leads (blue arrows).
Question: What is the reason for ST-segment elevation? What is the most likely diagnosis?
Interpretation and Clinical Course
The ECG (Figure) showed sinus rhythm (heart rate, 69 beats/min), slightly widened, fragmented QRS (f-QRS) complexes (112 ms) (red arrows), ST-segment elevation of 1 to 2 mm with T-wave inversion in the right precordial leads (V1 to V3), and bidirectional T wave in lead V4. ST-segment elevation with T-wave inversion in the right precordial leads can occur in various conditions, including acute anterior myocardial infarction, pulmonary embolism, myocarditis, Takotsubo cardiomyopathy, athlete’s heart, type 1 Brugada pattern, and ventricular aneurysm. The patient was not an athlete and had no symptoms of chest pain. Moreover, troponin I, NT-pro BNP, and D-dimer levels were all normal. Therefore, the first 4 possibilities were considered less likely. Type 1 Brugada pattern is characterized by a coved-type ST-segment elevation in the right precordial leads. However, the ST-segment elevation was convex in this case, which is inconsistent with the type 1 Brugada pattern. A closer evaluation of the ECG revealed a low-amplitude signal (amplitudes <1 mm, duration 40 ms) occurring after the QRS complex and before the onset of the T wave in the right precordial leads, which were very subtle, the so-called “epsilon wave.”1 In combination with ventricular fibrillation, the epsilon wave suggested that the diagnosis might be arrhythmogenic right ventricular cardiomyopathy (ARVC). Further echocardiographic examination revealed RV enlargement accompanied by regional thinning, and an aneurysm in the RV apex. The 24-hour Holter monitoring showed multifocal premature ventricular complexes (10 138 per 24 hours). The pacemaker’s programming control revealed that all 3 shocks were delivered to terminate ventricular fibrillation with conversion to sinus rhythm after ICD shocks. The patient was diagnosed with ARVC due to the presence of at least 2 major diagnostic criteria (aneurysm, epsilon waves, and inverted T waves in the right precordial leads).2 Amiodarone was prescribed as an antiarrhythmic therapy and to reduce the frequency of ICD shocks.
Arrhythmogenic right ventricular cardiomyopathy is a heritable cardiomyopathy that predominantly affects the RV, and its prevalence is estimated to be 1 in 2000 to 5000. Approximately 20% of sudden cardiac deaths in young people and athletes are caused by previously undiagnosed ARVC.3 Progressive fibrofatty replacement of the RV myocardium is the characteristic histopathologic feature, which results in wall thinning and aneurysmal dilatation, typically localized in the inflow and outflow tract and apex (“triangle of dysplasia”). The fibrofatty tissue that replaces the myocardium is thought to contribute to the development of ventricular arrhythmias by slowing intraventricular conduction and acting as a substrate for arrhythmias.3 A 12-lead ECG is a valuable diagnostic test for ARVC and records repolarization or depolarization abnormalities in up to 90% of patients with ARVC.4 Negative T waves in the right precordial leads are the most common finding (repolarization abnormalities).4 The epsilon wave is a low-amplitude deflection located between the end of the QRS and the onset of the T wave in the right precordial leads. Whereas the f-QRS is defined as the presence of additional spikes in the QRS complex without bundle branch block. In the current ECG, the deflections in the QRS complexes are called the f-QRS (Figure, red arrows); the deflections that occurred after the end of the QRS complexes are called the epsilon wave (Figure, blue arrows). It represents delayed potentials resulting from slow intraventricular conduction due to islands of surviving myocardium interspersed with fatty and fibrous tissue, and is the major diagnostic criterion (depolarization abnormality) for ARVC. However, the epsilon wave may be too small to be recorded and has a detection rate ranging from 15% to 30% on a standard 12-lead ECG.5 The Fontaine bipolar precordial lead ECG placement is a modified technique for ECG recording, where the left arm electrode is placed on the xiphoid process, the right arm electrode on the manubrium, and the left leg electrode in the location of V4. The detection rate of the epsilon wave significantly increases to 57% when the Fontaine lead system is used.5 However, the epsilon wave can also be present in other pathologic conditions, such as RV myocardial infarction, Uhl anomaly, after repair of Fallot tetralogy, and cardiac sarcoidosis. Therefore, the diagnosis of ARVC should not be based solely on the epsilon wave and other clinical features (such as RV aneurysm, RV dilatation, inverted T waves in the right precordial leads, and ventricular arrhythmias) are required to make this diagnosis.
The typical ECG manifestation of ventricular aneurysm is persistent ST elevation, with or without Q waves. The frequency of ST-segment elevation varies from 84% to 100% in patients with ventricular aneurysm.6 Right ventricular aneurysm is present in 10.6% of patients with ARVC, and a lower RV ejection fraction is associated with a higher risk of RV aneurysm.7 In addition, patients with ARVC with right precordial ST-segment elevation have a higher risk of sudden death compared with patients without ST-segment elevation.8
This case demonstrated the diagnostic challenges confronted by clinicians when treating ventricular arrhythmia with ST-segment elevations and T-wave inversions in the right precordial leads. Clinicians should carefully analyze the ECG to search for clues for its possible etiology, such as the epsilon wave in ARVC. Overall, ventricular arrhythmia, ST-segment elevation with T-wave inversion in the right precordial leads, and epsilon waves can provide evidence for the diagnosis of ARVC with RV aneurysm.
Take-home Points
Epsilon wave is a major diagnostic criterion (depolarization abnormality) for ARVC.
The diagnosis of ARVC should not be based solely on the epsilon wave, and other clinical features (such as RV aneurysm, RV dilatation, inverted T waves in the right precordial leads, and ventricular arrhythmias) are required to make this diagnosis.
Right precordial leads ST elevation in ARVC usually indicates RV aneurysm.
Patients with ARVC with right precordial ST-segment elevation have a higher risk of sudden death compared with patients without ST-segment elevation.
Ventricular arrhythmia, ST-segment elevation with T-wave inversion in the right precordial leads, and epsilon waves can provide evidence for the diagnosis of ARVC with RV aneurysm.
(23). Jacob John et al. Burden of Typhoid and Paratyphoid Fever in India. N Engl J Med. 2023;388:1491-1500.
In 2017, more than half the cases of typhoid fever worldwide were projected to have occurred in India. In the absence of contemporary population-based data, it is unclear whether declining trends of hospitalization for typhoid in India reflect increased antibiotic treatment or a true reduction in infection.
Methods
From 2017 through 2020, we conducted weekly surveillance for acute febrile illness and measured the incidence of typhoid fever (as confirmed on blood culture) in a prospective cohort of children between the ages of 6 months and 14 years at three urban sites and one rural site in India. At an additional urban site and five rural sites, we combined blood-culture testing of hospitalized patients who had a fever with survey data regarding health care use to estimate incidence in the community.
Results
A total of 24,062 children who were enrolled in four cohorts contributed 46,959 child-years of observation. Among these children, 299 culture-confirmed typhoid cases were recorded, with an incidence per 100,000 child-years of 576 to 1173 cases in urban sites and 35 in rural Pune. The estimated incidence of typhoid fever from hospital surveillance ranged from 12 to 1622 cases per 100,000 child-years among children between the ages of 6 months and 14 years and from 108 to 970 cases per 100,000 person-years among those who were 15 years of age or older. Salmonella enterica serovar Paratyphi was isolated from 33 children, for an overall incidence of 68 cases per 100,000 child-years after adjustment for age.
The incidence of typhoid fever in urban India remains high, with generally lower estimates of incidence in most rural areas. (Funded by the Bill and Melinda Gates Foundation; NSSEFI Clinical Trials Registry of India
(24). Hoeper MM, et al. Phase 3 Trial of Sotatercept for Treatment of Pulmonary Arterial Hypertension. N Engl J Med. 2023;388:1478-1490.
Pulmonary arterial hypertension is a progressive disease involving proliferative remodeling of the pulmonary vessels. Despite therapeutic advances, the disease-associated morbidity and mortality remain high. Sotatercept is a fusion protein that traps activins and growth differentiation factors involved in pulmonary arterial hypertension.
Methods
We conducted a multicenter, double-blind, phase 3 trial in which adults with pulmonary arterial hypertension (World Health Organization [WHO] functional class II or III) who were receiving stable background therapy were randomly assigned in a 1:1 ratio to receive subcutaneous sotatercept (starting dose, 0.3 mg per kilogram of body weight; target dose, 0.7 mg per kilogram) or placebo every 3 weeks. The primary end point was the change from baseline at week 24 in the 6-minute walk distance. Nine secondary end points, tested hierarchically in the following order, were multicomponent improvement, change in pulmonary vascular resistance, change in N-terminal pro-B-type natriuretic peptide level, improvement in WHO functional class, time to death or clinical worsening, French risk score, and changes in the Pulmonary Arterial Hypertension-Symptoms and Impact (PAH-SYMPACT) Physical Impacts, Cardiopulmonary Symptoms, and Cognitive/Emotional Impacts domain scores; all were assessed at week 24 except time to death or clinical worsening, which was assessed when the last patient completed the week 24 visit.
Results
A total of 163 patients were assigned to receive sotatercept and 160 to receive placebo. The median change from baseline at week 24 in the 6-minute walk distance was 34.4 m (95% confidence interval [CI], 33.0 to 35.5) in the sotatercept group and 1.0 m (95% CI, -0.3 to 3.5) in the placebo group. The Hodges-Lehmann estimate of the difference between the sotatercept and placebo groups in the change from baseline at week 24 in the 6-minute walk distance was 40.8 m (95% CI, 27.5 to 54.1; P<0.001). The first eight secondary end points were significantly improved with sotatercept as compared with placebo, whereas the PAH-SYMPACT Cognitive/Emotional Impacts domain score was not. Adverse events that occurred more frequently with sotatercept than with placebo included epistaxis, dizziness, telangiectasia, increased hemoglobin levels, thrombocytopenia, and increased blood pressure.
Conclusions
In patients with pulmonary arterial hypertension who were receiving stable background therapy, sotatercept resulted in a greater improvement in exercise capacity (as assessed by the 6-minute walk test) than placebo
(25). Accompanying Editorial
Pulmonary arterial hypertension is a devastating disorder characterized by precapillary pulmonary hypertension not caused by respiratory disease, obstruction of the pulmonary arteries, or certain less-common conditions. Idiopathic pulmonary arterial hypertension, heritable pulmonary arterial hypertension, and pulmonary arterial hypertension associated with a connective-tissue disease or exposure to drugs such as methamphetamine account for most cases in the developed world. For years, pulmonary arterial hypertension was considered to be an untreatable, progressive, and rapidly fatal condition.1 A new era of treatment for patients with pulmonary arterial hypertension began three decades ago. Investigations that were focused on imbalanced vasoconstriction and vasodilation produced groundbreaking research findings
