C. Vishnu
Deputy Nursing Superintendent, Kauvery Hospital, Hosur, India
*Correspondence: +91 90870 30738; nursing.hosur@kauveryhospital.com
Success story of a patient with Haemangioma
Background
The aim of this article is to highlight the significance of Giant Hemangioma, the term reserved for lesions larger than 5 cm. Giant hemangiomas are uncommon, even rare, and often difficult to diagnose because of exophytic development.
The most prevalent type of liver tumor is hemangioma with a prevalence of upward of 10%. Treatment is recommended for symptomatic tumors, fast growth, rupture, or doubts about the diagnosis. The best surgical treatment option for hepatic hemangiomas is still being debated. Hemangioma can develop in a variety of organs, including the brain, where they can occasionally cause complications. They never do in the liver. They do not develop into cancer and only produce symptoms if they get very big.
Case Presentation
A 45-year-old female patient presented to the OPD with complaints of diffuse discomfort in the abdomen on and off for 4 to 6 months, abdominal pain, fever on and off since 1 week and low appetite. There was no history of hematuria or black stools.
Patient was shifted to the ward and got admitted. On admission, she was conscious, oriented and vitals were stable.
After evaluation with the relevant investigations such as CT chest, ECG, Echo, and CT Abdomen. Patient was diagnosed with Giant Haemangioma in the right lobe of liver and was hospitalized for right Hepatectomy.
On Clinical Assessment
| Temperature | Pulse | Respiration | BP | SpO2 |
| 97 | 84 | 22 | 90/60 | 99 |
Investigations
CECT abdomen revealed e/o large ill-defined hypo-dense lesion which showed peripheral puddling enhancement in arterial phase and centripetal filling in delayed phase involving right lobe of liver, segments V, VI, VII. Areas of central scarring were noted with calcification – s/o large hepatic hemangioma. Small cyst was noted in the right kidney, a right renal tiny non obstructive intra renal calculus, and a bulky uterus.
Surgery Plan
Patient was planned for right hepatectomy. Patient was kept on NPO from midnight.
OT preparation was done, given Inj. Magnex Forte 1.5 g 1V before half an hour surgery.
Intra-operative period:
- Intra-operative period analgesia administered was:
- Inj. Fentanyl 100 mcg
- Inj. Fentanyl Infusion- IV 2 ml/h,
- Inj. Morphine 4 mg.
- Intra-op blood loss was 500 ml
- Intra-op- 1 PRBC Transfusion done.
- Patient was intubated and placed on mechanical ventilator.
- Lines and drains: Patient was on Ryles tube, Foleys catheter, drain-1, Arterial line, CVP line, Epidural analgesia present.
- Biopsy specimen sent to lab.
- Overall intra-operative period was uneventful.
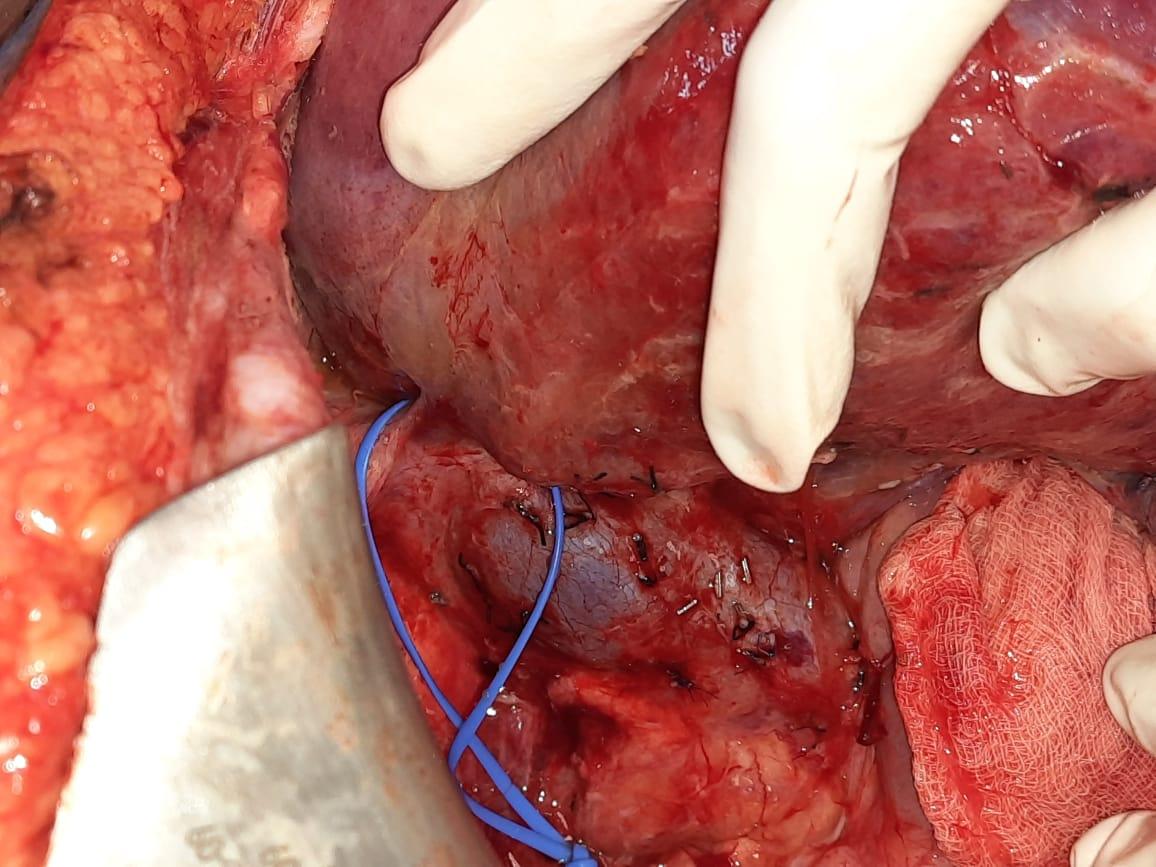
Fig 1. Liver Resection
Intra-operative Findings
- Large hemangioma involving segment 6, 7, & 8.
- Long right hepatic artery.
- IOC: Type I bile duct anatomy.
- Post bile duct transformation IOC, good right duct stump.

Fig 2. No leak (propofol cholangiogram)
Patient was shifted to ICU for further management and observation.
On admission to ICU, the observations noted were;
- Patient on ventilator support.
- Inj. Fentanyl 2 ml/h on flow.
- Extubated the patient, nebulization given and encouraged for spirometry.
- Chest physio given.
- IV fluid 200 ml/h.
- As per consultant advice, to remove Epidural line.
- Inj. Fentanyl 4 ml/h on flow.
- N4 aspiration 6th hourly.
Nursing Care
Pre-Op
- On admission, she had abdomen pain, fever.
- Diagnosed giant haemangioma right lobe of liver.
- Advised to undergo right hepatectomy
Post-Op
- Post-operatively patient was on ventilator support.
- Intake/output chart was maintained accurately.
- Nutritional support was enhanced with soft solid diet.
- Patient vitals were monitored hourly.
- Aseptic precautions were followed during patient handling.
- Staff Nurses maintained care of patients.
- Calm and quiet environment was given to promote sleep.
Nursing management
The patient was managed for post OP care for right hemangioma right lobe of liver surgery.
On POD 1: Patient on ventilator support and Ryles tube, Foleys catheter, Arterial line, CVP line, Epidural line present, biopsy sent to Lab. Back care given.
On POD 2: Extubated the patient and nebulization given and encourage spirometry. Continued antibiotic and IV fluids 200 ml/h. Monitored the BP and continued the IV fluids, Epidural Line was removed.
On POD 3: Patient shifted from ICU to ward, conscious and oriented, Inj. Fentanyl 3 ml/h on flow and LFT CBC were normal. Patient followed the normal diet and enema was given.
On POD 4: Foley’s (+), Drain (+) 26 ml, Hb – 7.7, To add the T. Heptagon and to remove Foley’s removed, CVC, drain to remove before discharge. Follow normal diet.
On POD- 5, Advised to discharge, Venflons were removed.
At the time of discharge patient was conscious, oriented and stable.
Dietary Advice
Iron-rich diet/high protein diet
Discharge Medications:
Discharge Medications:
| Drugs | Dosage | Right Time |
| Cap. Katadol 100 mg | 1-0-1 | After food |
| Tab. Esoz 40 mg | 1-0-0 | Before food |
| Tab. Heptogon | 1-0-1 | After food |
| Tab. Fefol Z | 1-0-0 | After food |
| Syp. Duphalac 15 ml | 0-0-1 | After food |
Conclusion
With careful patient selection, surgical treatment of hepatic hemangiomas is a very effective treatment with no mortality or significant morbidity. Patient’s intra and post operative period was uneventful, tolerated soft diet, and was mobilized well.

Mr. C. Vishnu
Deputy Nursing Superintendent
