The heat-stricken life – Treatment in time only saves lives!
Kalaimuhilan
Second-year Emergency Medicine Resident, Kauvery hospital, Chennai, India
Abstract
Heatstroke is the most hazardous condition in a spectrum of illnesses progressing from heat exhaustion to heatstroke, in which a shared finding is hyperthermia (i.e., the rise in core body temperature when heat accumulation overrides heat dissipation during exercise or exposure to environmental heat stress). In this case series, we discuss about acute onset presentations of heat stroke which mimic as sepsis and discuss the treatment, management and prognosis of heat stroke in patients. This work emphasizes on early recognition and swift treatment to improve the outcome of a patient suffering with heat stroke and avoiding the utter tragedy of mortality.
Background
Heat stroke is characterized by extreme hyperthermia (usually >40.5oC), central nervous system (CNS) dysfunction, and multiorgan failure. Depending on its cause, heatstroke may be categorized as either classic (passive) or exertional. Both types derive from failure to dissipate excessive body heat, but their underlying mechanisms differ. Classic heatstroke is due to exposure to environmental heat and poor heat-dissipation mechanisms, whereas exertional heat-stroke is associated with physical exercise and results when excessive production of metabolic heat overwhelms physiological heat-loss mechanisms.
Case 1
A 23-years-aged young man, had sudden unresponsiveness and loss of consciousness while running the lap of a marathon (10 km). He was observed to have laboured and noisy breathing. He was taken to an outside hospital within 15 min of onset of loss of consciousness. On arrival at outside hospital, his vitals were temp, 99.6°F; BP, 80/60; GCS, 9/15 (E2V2MS). After initial management, he was shifted to another hospital. On arrival at the other hospital, patient was febrile (temp: 104°F), GCS: 5/15 (E1VIM3), and still hypotensive. In view of severe shock, patient was started on inotropes (Noradrenaline infusion). In view of low GCS, he was intubated, and he has transfused 4 units of FFP due to increased PT INR: 5.14.
Patient was shifted to Kauvery hospital for further management on day 3.
On examination, patient was comatose, GCS, 2T/15; HR, 112/min; SpO2, 100% at FiO2, 100%, BP, 100/60 on inotrope support (Noradrenaline infusion).
Blood investigations here revealed altered coagulation and deranged liver function tests.
In view of severe coagulopathy – he was transfused with multiple blood products (4 units of FFP and 5 units of Cryoprecipitate).
CT Chest showed features suggesting non-cardiogenic pulmonary edema. Mild pneumopericardium was present. CT abdomen showed severe fatty liver. MRI Brain showed few microhemorrhages in bilateral posterior parietal subcortical white matter, right corona radiata, and features of suggestive of cerebral edema.
EEG done showed evidence of widespread slow activity reflecting fairly severe cortical dysfunction.
Urine c/s & Mini BAL c/s showed no growth.
A multidisciplinary team was involved in the aggressive management of this patient. He was treated with high doses of inotropes, sedatives, maximum ventilator support. On day 4 of stay at our hospital, the patient had cardiac arrest, and despite all resuscitative measures, patient could not be revived and was declared dead.
Case 2
An 86-years-aged lady presented to ER with complaints of vague generalised weakness and was found to be in agitated state, and acute confusional state, with history of high-grade fever for 2 days. She had history of abdominal discomfort for 2 days.
On arrival here, the patient was conscious, oriented, febrile at 100.4°F, dehydrated (++), BP, 90/60 mmHg; PR, 102/min; RR, 20/min; SpO2, 98% with 1O L 02. The initial blood investigations done here ravealed severe metabolic acidosis on ABG, and associated elevated LFT, CRP, D- dimer, Sr. LDH, urea, Ammonia and altered coagulation profile. Trop I was positive.
Echo showed global hypokinesia (LVEF ~30%). Urine C/S done showed Gram Negative Bacteria (GNB) growth for which appropriate antibiotics were initiated.
In view of persistent desaturation, patient was put on Non-invasive ventilator support.
Multidisciplinary team of specialists were involved in the care of this patient. On day 4 of hospital stay here, the patient’s condition worsened progressively with severe refractory metabolic acidosis. She went into bradycardic arrest, and despite all resuscitative measures, return of spontaneous circulation could not be achieved and she was declared dead.
Case 3
A 59-years- aged lady, known DM, RA, ILD, presented to ER with complaints of high-grade fever with worsening knee pain for 2 days. H/o sudden onset of worsening drowsiness for 2 h on day 3.
On arrival at ER, patient was drowsy, mildly arousable, dehydrated ++. Temp, 106.3 F; SpO2, 96 room sir, pulse, 128 bpm; BP, 120/60 mmHg; RR, 14; CBG, 260; GCS-9/15.
She lived in a house on the fourth floor above which was the terrace and she stayed in a room with barely any cross ventilation. When she was brought here systemic examination revealed bilateral fine crepitations in both lung fields.
She was started on IV fluid (bolus + maintenance), and then intubated in view of the low GCS. Following intubation, she developed hypotension, hence she was started on inotropes. Initial ABG showed mild metabolic acidosis and here initial blood investigations showed elevated total count, mildly deranged renal and liver functions and deranged coagulation profile. Pan cultures were done which was negative for any growth.
Patient has managed aggressively with rapid cooling measures like cold sponges, ice packs application, cooling blanket, cooling fans bedside of patient in the ICU along with cold IV fluids, and prophylactic IV antibiotics, and IV steroids. On day 2 of hospital stay, she was afebrile and she was extubated as she regained full consciousness. Her repeat blood parameters should resolution and eventually, she got discharged after 4 days with full recovery.
Discussion
There are 2 major types of heat strokes:
(1) Classic Heatstroke
Classic heatstroke frequently occurs as an epidemic among elderly persons whose ability to adjust physiologically to heat stress has become compromised, chronically ill persons, and those who cannot care for themselves.
Prepubertal children are also regarded as a population at risk. Children’s susceptibility to classic heatstroke is attributed to a high ratio of surface area to mass (leading to an increased heat-absorption rate), an underdeveloped thermoregulatory system (impairing effective heat dissipation), small blood volume relative to body size (limiting the potential for heat conductance and resulting in greater heat accumulation), and a low sweating rate (reducing the potential for heat dissipation through sweat evaporation).
(2) Exertional heatstroke
It is a medical emergency, sporadic in nature, and directly related to strenuous physical activity. It can strike athletes, laborers (e.g., firefighters and agricultural workers) and soldiers. Exertional heatstroke can occur even within the first 60 min of exertion and may be triggered without exposure to high ambient temperatures.
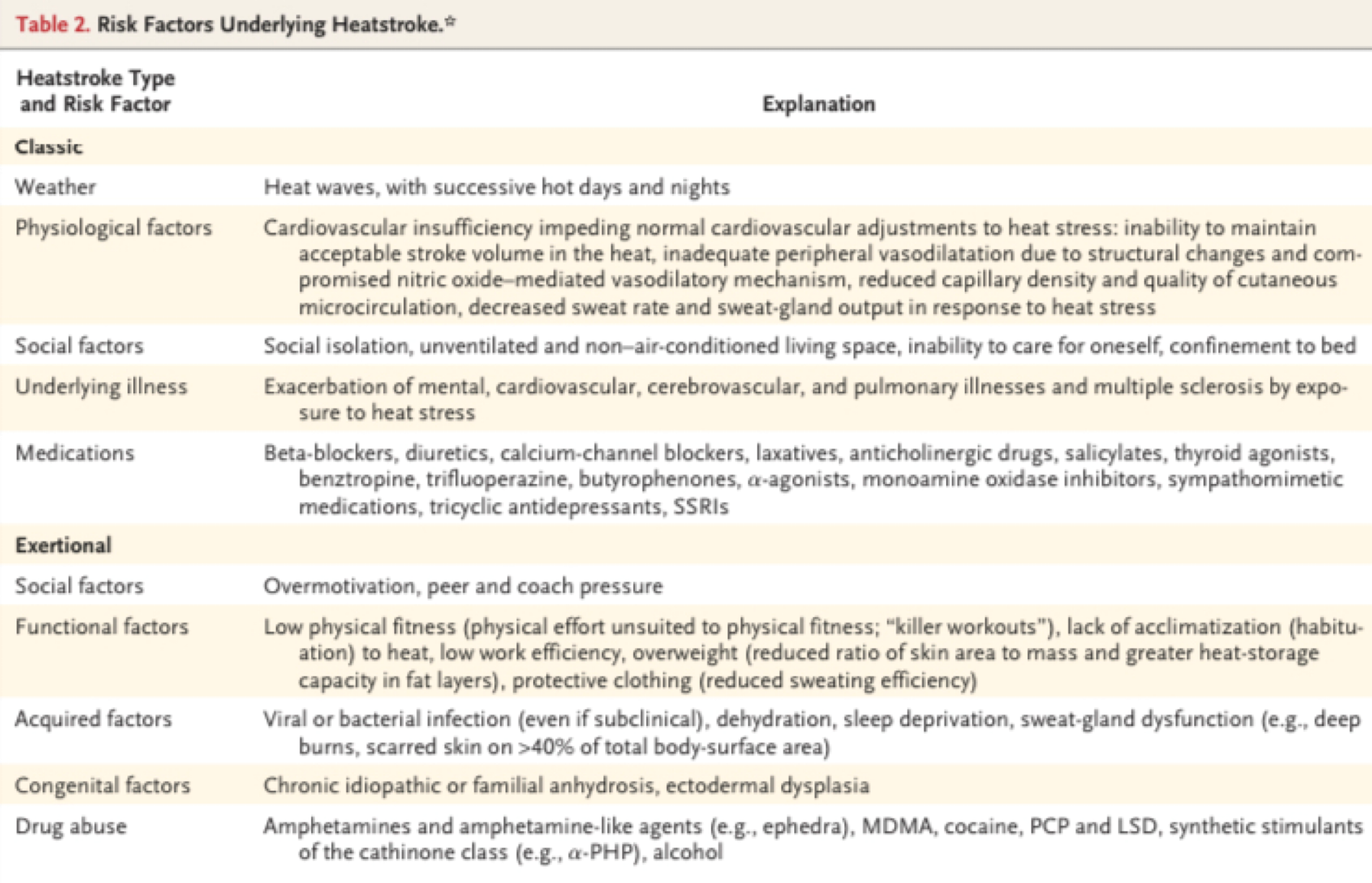
The risk factors for heat stroke are as follows:
The disorder has three phases, which are seen more clearly in exertional heatstroke than in classic heatstroke:
(a). A hyperthermic- neurologic acute phase,
(b). A hematologic-enzymatic phase (peaking 24 to 48 h after the event), and
(c). A late renal-hepatic phase (if clinical symptoms are sustained for 96 h or longer).
Most critical for primary care practitioners is the acute phase, since prompt recognition and treatment of heatstroke in the acute phase may be lifesaving.
Pathophysiological mechanism
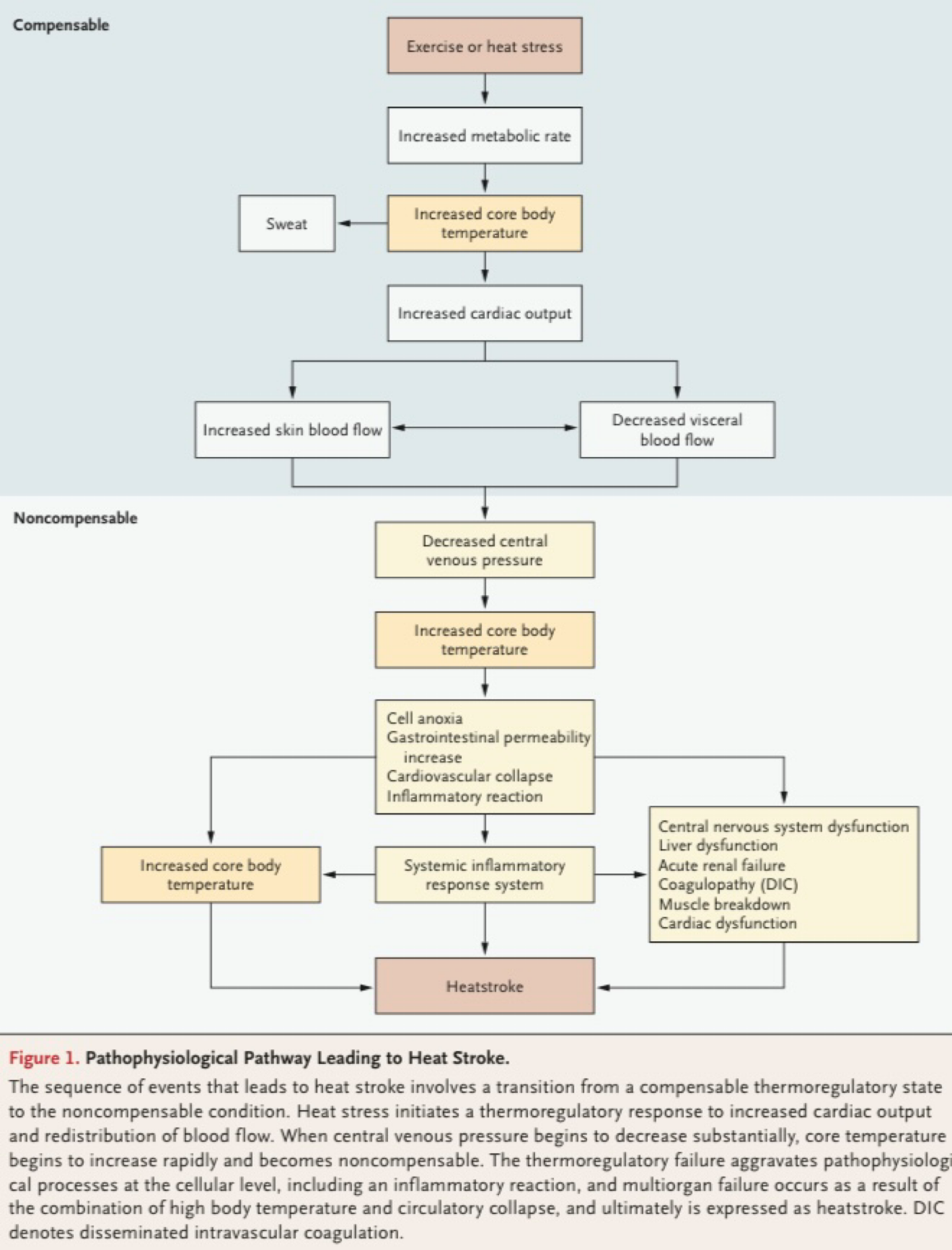
Given the brain’s extreme sensitivity to hyperthermia, CNS disturbances are inevitable in heat- stroke. Early symptoms include behavioral changes, confusion, delirium, dizziness, weakness, agitation, combativeness, slurred speech, nausea, and vomiting. Seizures and sphincter incontinence may occur in severe cases, mainly in exertional heatstroke.
Heat cramps | Heat Stress (Exhaustion) | Heat Stroke |
Muscle cramps | Symptoms seen in heat cramps Plus | Symptoms seen in heat stress (exhaustion) plus |
Normal to mildly elevated temperature | Normal to elevated temperature (<40°CI<104°F1)
| Elevated temperature (>40°C>104°F1) |
Sweating | Nausea, vomiting, headache, malaise, dizziness orthostatic hypotension | Neurologic abnormalities: inappropriate behavior, confusion, delirium, ataxia, coma, seizures, Anhidrosis or sweating |
Consciousness commonly deteriorates but is usually regained once the temperature falls below the critical level of 40.5°C. In severe cases, brain edema ensues. Brain injury appears to be concentrated in the cerebellum, with generalized atrophy and evidence of involvement of the Purkinje cell layer. Neuronal injury to the autonomic and enteric nervous systems may be long-lasting. The hypothesis that damage to the preoptic anterior hypothalamus is responsible for the loss of thermoregulation has not been proved.
Multiorgan system dysfunction and failure (more pronounced in exertional heatstroke than in classic heatstroke) may peak within 24 to 48 h. If treatment is prompt, clinical signs become milder in most cases and abate within a few days. Possible complications range from sustained alteration in consciousness to DIC, acute respiratory distress syndrome, and acute renal, cardiac, and hepatic dysfunction and failure.
Rhabdomyolysis, although not pathognomonic, is typical of exertion. Some neurologic sequelae (e.g., cerebellar ataxia, dysarthria, cognitive disorders, and anterograde amnesia) may persist for several weeks to months.
Management of heatstroke patients
Management of heat stroke includes ensuring adequate airway protection, breathing, and circulation. After ABC’s, rapid cooling measures like using cold sponging, cooling blankets, ice packs, cooling fans, cold IV fluids become the mainstay of treatment with ancillary management in response to other end-organ damage. Intubation for profound unconsciousness is rarely needed, as rapid cooling quickly improves the Glasgow coma scale. Adequate rehydration is essential without over-correcting the sodium if derangements exist. It is mandatory to measure core temperature with a rectal or esophageal probe continually and cooling measures should be stopped once the temperature is 38 to 39℃. No definitive studies support any cooling method over another. Ice bath immersion is the timeliest to reduce core body temperature, however, in older populations, it may not be realistic as cardiac monitoring may not be feasible and extreme agitation may hinder compliance. Other common methods include ice pack applications to the groin or axilla and evaporative cooling using a fan with cool saline on the skin of patients.
Several pharmacologic adjuncts also merit consideration in the treatment of heat stroke. Dantrolene is a skeletal muscle relaxer, shown to reduce heat production in sustained muscle contracture, and is useful for the treatment of malignant hyperthermia. However, it has been shown to have no effect on patient outcomes with heat stroke. A small study suggested that high-dose benzodiazepine may blunt the shivering reflex and decrease oxygen consumption, therefore providing a theoretical benefit to patients. The problem is that heat stroke patients may be unable to compensate through mechanisms such as shivering. Therefore, the universal use of benzodiazepines is not the current recommendation but could be tailored to the shivering, agitated patient. There is no role for antipyretics in the treatment of heatstroke patients and may be toxic to the liver.
Prognosis
Patients presenting with heat stroke have high mortality depending on the etiology of the presentation. When therapy is delayed, the mortality rate may be as high as 80%; however, with early diagnosis and immediate cooling, the mortality rate can be reduced to 10%. The increased mortality rate is likely due to the higher prevalence of comorbidities and older age in the classic population.
Conclusion
In our case series – the first 2 patients succumbed to the disease due to delay in recognition of heat stroke and delay in initiating aggressive cooling measures, whereas the 3rd patient survived despite developing multiorgan dysfunction due to prompt aggressive cooling measures and correction of dehydration status in the patient.
Heatstroke is a life-threatening condition if it is not promptly recognized and effectively treated at the acute phase. Recognising and treating the patient at the earliest can significantly reduce the outcome and mortality rate. For this one must have a high index of suspicion of heat stroke and this is possible with a detailed history taking of the patient. Certain simple preventive measures, such as avoiding strenuous activity in hot environments and reducing exposure to heat stress, as well as changing attitudes in sports and addressing socio-economic issues that augment risk, can reduce the prevalence of both classic and exertional heatstroke. Our understanding of the pathophysiology of heatstroke and mechanism-based treatment approaches is still incomplete.
Future research is likely to focus on three areas:
Identifying genetic traits that might reduce a person’s ability to cope with heat stress, searching for new biomarkers that can better predict short and long-term outcomes of heatstroke, and developing new adjuvant treatments that can effectively control the inflammatory reaction and counteract multiorgan complications.
References
[1] Epstein Y, Yanovich R. Heatstroke. Heatstroke. N Engl J Med. 2019;380(25):2449-59.
[2] Hifumi T, Kondo Y, Shimizu K, et al. Heat stroke. J Intensive Care 2018;6:30.
[3] Morris A, Patel G. Heat Stroke. In: StatPearls. Treasure Island (FL): StatPearls Publishing;2022
